1. Background
Pain is a mental and unique phenomenon that depends on various biological, psychological, as well as social factors, and different groups of the population experience it differently (1). In 1979, the International Association for the Study of Pain (IASP) described it as an unpleasant experience and sensation, which accompanies acute or potential tissue damage (2, 3). Patients admitted to treatment centers undergo multiple painful processes. Several studies have shown that painful procedures could give rise to significant physiological and psychological complications. Children are among the groups for whom treatment pains entail significant consequences on their physiological parameters (4, 5). In this context, some of the most important physiological effects are increased heart rate, respiration, as well as blood pressure, and decreased arterial oxygen saturation. If uncontrolled, any of these problems can lead to adverse outcomes to individuals’ functioning systems (6).
One of the most painful experiences that a child has when admitted to the hospital is inserting the needle into the vein (7, 8). For this reason, some researchers have recently focused on studying possible methods of managing and reducing the physiological effects of needle insertion in children (9).
In general, the physiological effects of painful procedures can be alleviated through pharmaceutical and non-pharmaceutical methods. Not requiring a physician’s prescription nor entailing physical complications, non-pharmaceutical methods are now widely available and cost-effective (10). These methods encompass a wide range of interventions, which do not involve taking drugs for pain management. Cognitive-behavioral and physical approaches are the two principal categories in this context (11). Evidence shows that cognitive-behavioral approaches actively engage children and help them divert their attention from the painful procedure. Music, distraction, and relaxation techniques are among these interventions (12). There is another strand of non-pharmaceutical interventions that include physical approaches such as putting children in a comfortable state (13), heat and cold treatment (14), massage and skin stimulation (10, 15), caressing, swaddling, sucking, acupuncture, and electrical stimulation of the skin (6, 16).
In this category, massage therapy is an effective control technique that can mitigate the emotional components of pain and reduce stress and anxiety (17). A massage stimulates skin nerve fibers and prevents the transmission of pain signals, thus reducing pain. Furthermore, a massage can make patients feel that other people are helping reduce their stress (18). Several studies have confirmed the application of massage to control pain caused by cancer (19) and musculoskeletal problems (20). Celebioglu et al. reported the positive effect of a massage on relieving the pain due to bone marrow aspiration (17). Chik et al. (21) employed massage therapy to control the pain associated with the insertion of a needle into the vein of newborns.
Although a wide range of skin stimuli such as vibration (22) have been deployed to control the pain of intravenous insertion in children, there are few studies concerning the effects of a massage on reducing physiological changes in this population group during this procedure.
2. Objectives
The present research is an attempt to address this lack in the case of children aged three to six years who had been admitted to the Surgery Ward of Tabriz Children Hospital.
3. Methods
This clinical trial was performed between 2016 and 2017 on 70 children aged three to six years who had been hospitalized in the Surgery Ward of Tabriz Children Hospital. The study began after obtaining the approval of the Ethics Committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1395.134).
The sample size was calculated using the mean difference formula, 95% confidence interval, 90% power, and 0.05 accuracy based on the study by Sahiner et al., which was conducted to measure pain in children (9). Considering the possible sample attrition, 10% was added to the original 35 so that the sample size consisted of 39 children in each group. Equation 1 shows the formula used to determine the sample size.
Where the values used for each of the variables are as follows:
μ1 = 0.4, μ2 = 1.2,
The criteria for entering the study included age from six to three years, lack of pain due to illness during venipuncture, full vigilance and physiological stability, lack of intellectual disability, as well as no use of painkillers, sedatives, corticosteroid, and relaxants. In the event of any incompatibility with the inclusion criteria and if the IV catheter were not inserted correctly in the first attempt, the child in question would be excluded from the study.
After acquiring parental consent and registering demographic characteristics, the researcher randomized qualified children into the control and experimental groups by using envelopes containing the name of one of the two groups. A hand massage was used to manage fluctuations of physiological parameters of children in the experimental group; in the control group; however, intravenous insertion was performed without any intervention. In order to have access to the study samples, the researcher referred to the ward at the end of the morning shift and chose the candidates who had been assigned for the next morning surgery and had been administered intravenous insertion and at the same time met the criteria for entering the study. After the goals of the study were explained to the parents and children were randomized to the control and experimental groups, IV line insertion was carried out at the end of the afternoon shift. All children underwent venipuncture in the presence of their mother using the catheter 22 (manufactured by Biçakcilar Inc.). This was carried out on patients’ bed by an experienced nurse. Intravenous insertion was performed on the dorsal vein of the non-dominant hand of children in both groups. To perform the intervention, five minutes before venipuncture and during the insertion, the researcher performed the massage procedure by slow caressing motions using the moderate pressure of the palm on the skin of the hand and arm and also slow taps around the venipuncture site. The control group underwent venipuncture according to the routine procedure.
Data on physiological parameters were measured and recorded by the assistant nurse through examining respiratory rate, heart rate, systolic blood pressure, and arterial oxygen saturation before and immediately after the intervention. A calibrated pulse oximeter (Novametrix Medical Systems Inc.) was used to measure heart rate and oxygen saturation, and a pressure gauge (fmt model) fitted to the child's arm size was used to determine systolic blood pressure. Besides, respiration was calculated for one minute and recorded accordingly. In order to ensure the reliability of systolic blood pressure and respiratory rate, the measurements were performed by two nurses for the first 10 samples and agreement coefficients were calculated. For other samples, one nurse undertook the measurement and Kappa coefficients above 0.9 were subsequently obtained. The sampling process was terminated once 35 children were examined in each group.
SPSS version 24 and descriptive statistical tests were used to analyze the resulting data. It should be added that p-values less than 0.05 were considered statistically significant.
4. Results
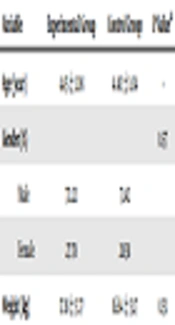
Given the lack of sample attrition, the study was conducted on 35 children in each group, and the results were drawn correspondingly. Therefore, a total of 70 eligible children were randomly assigned to the control and experimental groups and underwent intravenous administration. Statistically, there was no significant difference between the personal and demographic characteristics of children in the two groups (Table 1).
| Variable | Experimental Group | Control Group | P Valuea |
|---|---|---|---|
| Age (year) | 4.45 ± 1.08 | 4.40 ± 1.04 | - |
| Gender (%) | 0.57 | ||
| Male | 72.22 | 71.42 | |
| Female | 27.78 | 28.58 | |
| Weight (kg) | 17.18 ± 3.77 | 16.64 ± 3.17 | 0.51 |
Comparison of Personal Characteristics of Children in the Control and Experimental Groups
At first, the physiological parameters of children in the two groups were compared before intravenous administration. As shown in Table 2, physiological parameters (including respiratory rate, heart rate, and arterial oxygen saturation) did not significantly differ in the control and experimental groups prior to intravenous insertion.
| Variable | Experimental Group | Control Group | P Valuea |
|---|---|---|---|
| Respiratory rate | 24.06 ± 2.65 | 24.71 ± 2.37 | 0.27 |
| Heart rate | 118.43 ± 7.46 | 119.57 ± 8.12 | 0.54 |
| Systolic blood pressure | 93.57 ± 5.63 | 92.14 ± 6.09 | 0.31 |
| Arterial oxygen saturation | 95.77 ± 1.49 | 95.74 ± 1.70 | 0.94 |
Comparison of Physiological Parameters of Children in the Control and Experimental Groups Prior to IV Insertion
Table 3 presents the physiological characteristics of children in the two groups after intravenous insertion. As can be seen, the heart rate of children after IV insertion in the experimental group is significantly lower than that of the control group.
| Variable | Experimental Group | Control Group | P Valuea |
|---|---|---|---|
| Respiratory rate | 25.63 ± 2.91 | 27.00 ± 3.14 | 0.06 |
| Heart rate | 122.37 ± 7.85 | 126.74 ± 6.07 | 0.01 |
| Systolic blood pressure | 94.43 ± 5.39 | 93.00 ± 5.58 | 0.28 |
| Arterial oxygen saturation | 96.54 ± 1.54 | 96.50 ± 1.97 | 0.94 |
Comparison of Physiological Parameters of Children in the Control and Experimental Groups After IV Insertion
Physiological parameters of children before and after intravenous administration were compared in both groups, and the results of the statistical analysis demonstrated that there was a significant difference between the values of systolic blood pressure before and after venipuncture in the experimental group. However, this value did not statistically change after venipuncture in the control group. Table 4 provides the p-values obtained from statistical analyses of both groups.
| Variable | Experimental Group (P Value) | Control Group (P Value) |
|---|---|---|
| Respiratory rate | < 0.001 | < 0.001 |
| Heart rate | < 0.001 | < 0.001 |
| Systolic blood pressure | 0.01 | 0.08 |
| Arterial oxygen saturation | < 0.001 | < 0.001 |
Comparison of Physiological Parameters of Children in the Control and Experimental Groups Before and After IV Insertiona
5. Discussion
In this study, the effects of massage therapy on changes in the physiological parameters induced by intravenous line insertion (including increased respiratory rate, heart rate, and blood pressure, and decreased arterial blood saturation) were investigated in children aged three to six years. The results indicated that the respiratory rate and heart rate of children in both experimental and control groups were significantly higher after IV insertion than before this administration, which is consistent with previous reports (6, 7, 22, 23).
Thus, Ackerman et al. examined the effect of massage therapy on children undergoing cell transplantation. The results showed that although massage alleviates the physiological outcomes of the painful procedure, it does not eliminate all of these effects (24). Similar results were also observed by Agarwal et al., in 2005 (25) and O'Flaherty et al., in 2012 (26), who confirmed the salubrious impact of massage therapy in reducing - though not abolishing - the effects of painful procedures in children.
Another finding of the present study was that a hand massage is effective in controlling the increase in heart rate due to painful interventions. Thus, the heart rate of the group receiving the massage was significantly lower than that of the control group. While no study has been reported so far concerning the effect of massage on the physiological characteristics of children during insertion of an intravenous line, Pouraboli et al. verified the generally favorable impact of massage in children and recommended that nurses employ it during this painful procedure (27).
On the other hand, the current study observed that massage therapy does not bring a positive effect on other physiological parameters including respiration, systolic blood pressure, and arterial oxygen saturation. In fact, the values of these parameters did not fare much better in the experimental group than the control group. In this regard, van Dijk et al. exhibited that massage therapy has no considerable influence on the reduction of respiratory changes in children who suffered from burns (28). Similarly, Staveski et al. reported that massage does no significantly mitigate post-surgical pain in children (29).
It is worth noting that in the current study factors such as crowdedness of the ward and the excessive number of patients, excessive noise, and the mood of the child were regarded as confounding factors beyond the control of the researcher. This comprises the major limitation of the present research.
5.1. Conclusion
In the present study, hand massage was utilized during the insertion of the intravenous line to control the physiological parameters of children aged three to six years. The results showed that this non-pharmaceutical therapy could be used as an easy, inexpensive, and practical method for managing changes in heart rate during venipuncture. Although massage therapy has limitations such as the absence of experienced staff and the need for specialized training, it can be facilitated and turned into a standard treatment by providing appropriate training programs to the staff in charge. It is suggested that future studies focus on training massage therapy to parents in order to make children feel more safe and relaxed.