1. Background
Evidence suggests that medical errors occur to an unacceptably high degree during medical care procedures. In the US hospitals, for instance, 44,000 - 98,000 patients annually die only due to errors in the provision of hospital services (1).
Multiple studies all over the world have regarded effective communication between healthcare providers as the most critical factor in preventing medical errors (2). Recently, the Joint Accreditation Committee reported that the most frequent root causes of medical errors are associated with human factors and communication between the members of care teams (3).
Several studies have demonstrated the vital link between the safety of healthcare and collaborative work of the members of treatment teams (4, 5). This has prompted researchers to pay more attention to human factors and the relationships between care providers in hospitals. Clearly, improving communication indicators among care providers will be an enormous step towards making hospitals secure for patients. Surgery has especially attracted the attention of healthcare policy-makers, as well as safety researchers. The fact that globally 234 million surgical operations are performed each year highlights the importance of this integral part of the health system (6).
In its 2002 report, the World Bank announced that surgery prevented over 164 million disability-adjusted life years (7). Nevertheless, there are widespread errors in this part of the health system that jeopardize patients’ safety. Though quite common, these errors are avoidable (6). While the details of these errors are not documented in developing countries, various studies have shown that 0.4% - 0.8% of surgical procedures in developed countries end in death, and 3% - 17% of these operations entail grave side effects for patients (8, 9). However, studies have estimated that these values are far greater in developing countries (10, 11).
In this regard, the World Health Organization has designed and released guidelines in the form of a checklist to ensure the safety of surgical procedures. This checklist is applicable to all types of surgeries to coordinate surgical teams with different tasks and responsibilities through the verbal and non-verbal communication. Thus, it minimizes the risk of injury to the patient (12). Effective implementation of this tool in the operating room and thus realizing its optimal safety outcomes will occur provided that there is adequate information on both the current state of communication between the members of surgical teams and the shortcomings in these communications, as assessed based on this international tool. Several studies have been conducted across the world to examine the real communication between the members of surgical teams and to design interventions based on the items addressed in this checklist (13). Meanwhile, this issue has not been seriously pursued in Iran, despite the fact that medical errors are considered one of the most pressing challenges in Iranian hospitals, especially public hospitals, which dominate the hospital market in the country (14, 15).
2. Objectives
This study was carried out to investigate the patterns of communication between surgical teams in the operating room of a public hospital in Tehran, Shahid Lavasani, affiliated to the Social Security Organization. The WHO surgical safety checklist (SSC) was used to identify and classify the possible types of communication failure.
3. Methods
This observational, descriptive, cross-sectional study was carried out in the operating room of Dr. Lavasani Hospital, Tehran. General surgeries were observed during a two-month period from late September to late November 2018. According to some studies, various types of communications in the operating room are assigned to the general surgery field (16).
Cochran’s formula was used to determine the sample size of surgical operations:
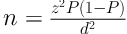
To estimate the prevalence of communication failure, three surgical operations were observed and analyzed. The prevalence of the examined variable (communication failure) in these operations was calculated to be 0.15%. Given the confidence of 95% and the precision of 0.1, the sample size was calculated to include 48 surgical operations. Proportional to size sampling (based on the number of general surgical procedures) was used to make the sample representative of all types of general surgeries. Overall, 19 cases of herniorrhaphy, seven cases of pilonidal sinus excision, 12 cases of cholecystectomy, and 10 other cases of general surgeries were chosen for observation. The surgical procedures were randomly selected among these groups. In each procedure, all the members of the surgical team were monitored, including surgeons, anesthesiologists, head nurses, head nurse assistants, anesthesia secretary and related personnel, and scrub and circulating nurses. The inclusion criteria were participants’ consent for taking part in the study and the contribution of study subjects to the surgical process as a member of the team. On the other hand, the exclusion criteria were outpatient surgeries that did not require anesthesia, emergency procedures due to the lack of uniformity of the patient’s admission protocol to the operating room, and the absence of all relevant roles. In addition, it was decided to exclude any surgical process in which a member of the surgical team, despite prior consent, expressed his/her opposition to the researcher’s observation.
Verbal and non-verbal behaviors of surgical teams were observed and qualitatively recorded based on the SSC by an expert with sufficient technical knowledge and 12 years of experience in the operating room. The obtained data were categorized and analyzed as quantitative data in SPSS version 25. In this study, the term “communication” refers to any verbal and non-verbal interactions (conveying the content of patients’ written records and other information) between two or more members of the surgical team.
After approval of the study by the Research Council and obtaining the required permits from the University’s Ethics Committee (IR.IAU.TMU.REC.1397.027), as well as the relevant authorities of the hospital, the researcher introduced herself to the study subjects and briefly described the purpose of the study to the selected surgical teams. Then, before starting the observation, the researcher acquired the consent of all members of the surgical teams and assured them about the confidentiality of information. The SSC was completed with the researcher while monitoring communication patterns of team members and choosing the appropriate options for the success/failure of verbal/non-verbal communication.
This checklist was completed for each of the surgical procedures at three stages, including patient’s admission until entry to the operating room, entry to the operating room until anesthesia induction, and anesthesia induction until patient’s transfer from the operating room. The observer monitored the surgical procedures in two different days of the week. Doing the observation, she took notes to better identify communication failures and recorded the most important points related to communication patterns between team members.
4. Results
Totally 31 individuals (eight surgeons, two anesthetists, one head nurse, one secretary, three head nurse assistants, and 16 personnel of the anesthesia and operating room) were studied in 48 surgical procedures. No surgical team was identical to other teams. In addition, none of the members was excluded from the study during the surgical process.
Table 1 presents the frequency of verbal and non-verbal communication among the members of the surgical teams. As seen, a significant portion of communication happened non-verbally. This included the complete examination of patient’s records, encompassing leaflets, identification bracelets, photographs, etc. Table 2 gives the incidence of communication failure associated with 11 items of the SSC. According to these results, the third stage of surgical procedures (anesthesia induction until patient’s transfer from the operating room) had the highest percentage of failure in verbal communication. The second stage of surgical procedures (patient’s entry to the operating room until anesthesia induction) was associated with the second highest incidence of failure in verbal communication. Eventually, the lowest level of verbal communication failure was related to the first stage (patient’s admission until entry to the operating room) (17.14%).
| Items of Surgical Safety Checklist | Frequency of Verbal/Non-Verbal Communication Out of 48 Cases (%) | |||||
|---|---|---|---|---|---|---|
| Admission Until Entry to the Operating Room | Entry to the Operating Room Until Anesthesia Induction | Anesthesia Induction Until Transfer from the Operating Room | ||||
| Verbal | Non-Verbal | Verbal | Non-Verbal | Verbal | Non-Verbal | |
| Frist name and last name | 27 (56.3) | 47 (97.9) | 10 (20.8) | 36 (0.75) | 6 (12.5) | 44 (91.7) |
| Type and site of surgery | 26 (54.2) | 47 (97.9) | 22 (45.8) | 38 (79.2) | 4 (8.3) | 42 (66.7) |
| Required documents for surgery | 12 (25.0) | 48 (100) | 5 (10.4) | 15 (31.2) | 1 (2.1) | 3 (6.2) |
| Prophylactic antibiotic administration | 0 (0) | 48 (100) | 1 (2.1) | 9 (18.7) | 3 (6.3) | 5 (10.4) |
| Patient’s known sensitivity | 23 (47.8) | 47 (97.9) | 5 (10.4) | 10 (20.8) | 0 (0.0) | 2 (4.2) |
| Considerations for patient management | 32 (66.7) | 43 (89.6) | 15 (31.2) | 15 (31.2) | 11 (22.9) | 8 (16.7) |
| Anesthetic equipment | * | * | 22 (45.8) | 48 (100) | 24 (50.0) | 47 (79.9) |
| Operating room equipment | * | * | 11 (22.9) | 45 (93.8) | 41 (85.4) | 48 (100) |
| Sterility of surgical instruments | * | * | 1 (2.1) | 14 (29.2) | 1 (2.1) | 39 (81.2) |
| Counting instruments, sponges, and needles | * | * | 0 (0.0) | 15 (31.2) | 13 (27.1) | 44 (91.7) |
| How the patient’s specimen labeled | * | * | 0 (0.0) | 0 (0) | 22 (45.8) | 30 (62.5) |
a Starred cases did not meet at the stage of patient’s admission to the operating room.
| Items of Surgical Safety Checklist | Frequency of Verbal Communication and Percentage of Failure in All Verbal Communications | ||
|---|---|---|---|
| Admission Until Entry to the Operating Room | Entry to the Operating Room Until Anesthesia Induction | Anesthesia Induction Until Transfer from the Operating Room | |
| Frist name and last name | 27 (0) | 10 (0) | 6 (33.3) |
| Type and site of surgery | 26 (0) | 22 (13.6) | 4 (25) |
| Required documents for surgery | 12 (41.7) | 5 (40) | 1 (100) |
| Prophylactic antibiotic administration | 0 (0) | 1 (100) | 3 (100) |
| Patient’s known sensitivity | 23 (0) | 5 (0) | 0 (0) |
| Considerations for patient management | 31 (3.1) | 15 (13.3) | 11 (18.2) |
| Anesthetic equipment | * | 22 (13.6) | 24 (4.2) |
| Operating room equipment | * | 11 (9.1) | 41 (14.6) |
| Sterility of surgical instruments | * | 1 (0) | 1 (0) |
| Counting instruments, gas, and needles | * | 0 (0) | 13 (7.7) |
| Patient specifications | * | 0 (0) | 22 (0) |
| Relative frequency percentage of all failures | 17.14 | 34.28 | 48.57 |
a Starred cases did not meet at the stage of patient’s admission to the operating room.
5. Discussion
The aim of this study was to explore the communication patterns of the members of surgical teams in the operating room. This was accomplished within the framework of the WHO’s surgical safety checklist in one of the hospitals in Tehran affiliated to the Social Security Organization. These communications were observed during 48 surgical procedures. It was found that the frequency of verbal communication based on the SSC was lower than that of non-verbal communication. This was especially true with regard to the three items of the type and position of surgery, counting instruments, and pathological sampling. This is while the SSC emphasizes the verbal expression of these actions. These results, similar to those obtained by Erestam et al. (17), indicate that it is vital to provide an appropriate context for promoting verbal communication among team members and proper implementation of SSC. In another study, Greenberg et al. (18) suggested that out of 60 study samples, 72% had communication failures, of which 92% were verbal.
One of the most remarkable findings of this study was that the highest rate of verbal communication failure occurred in the period between anesthesia induction and the end of operation, whereas this stage of the surgical process requires the highest degree of safety. In fact, this stage needs the most accurate and clear information.
To overcome this challenge, numerous studies have argued for the necessity of using a checklist that commits all members of the surgical team to implement the required items for realizing effective communication and enhancing teamwork (19). This effect could be the result of creating a shared mental model in the team members and assigning responsibilities to them (20).
In addition, the present study found no failure in terms of recording patient’s name and determining the type and position of surgery at the stage of admission to the operating room. Rather, communication failure happened between entry to the operating room and anesthesia induction. Moreover, no verbal communication took place between personnel responsible for patient delivery in the operating room and the nurse of the ward regarding the administration of prophylaxis antibiotics, which could have the greatest effect within one hour before skin excision. In this stage, the single notable communication was related to checking the patient’s records non-verbally. Besides, in only one out of 48 cases, information about the administration of prophylaxis antibiotics was provided verbally to anesthesia personnel. These results underscore the need for paying more attention to providing clearer, more accurate and comprehensive information at the stage of patient admission to the operating room.
5.1. Conclusions
The results showed that communication failure is common among the members of surgical teams. Considering the significance of communication in the operating room in terms of maintaining patient’s safety, reducing therapeutic errors, and obtaining other desired effects, it is crucial to address verbal/non-verbal interactions between team members during surgical procedures. Much research has proposed the surgical safety checklist as an effective tool for encouraging teamwork and promoting information transfer. In this regard, providing favorable conditions for successful communication seems to be one of the key factors in the proper implementation of this checklist. This will, in turn, cultivate teamwork in the operating room and guarantee the safety of surgical procedures.
It is suggested that future studies attempt to identify factors affecting communication failure among members of surgical teams. Detecting and illustrating disastrous outcomes caused by the lack of proper communication among team members of the operating room can be a further alert to policy-makers for establishing effective communications.
