1. Background
Pyelonephritis induced by renal parenchyma infection is considered as a potentially life-threatening condition which leads to the renal scarring (1, 2). According to pyelonephritis physiopathology, Bactria by entering into the kidney from the blood circulation, can influence and infect the kidney. In children, most common signs/symptoms of urinary tract infection probably exert as failure to thrive, feeding difficulty, fever, and vomiting (3, 4). For pyelonephritis diagnosis, a physical and historical evaluation as well as a urinalysis are requested to perform. Antibiotics therapy is considered as the first therapeutic choice for acute pyelonephritis treatment to prevent the progression of condition (5-7). According to the previous studies, it has also been proposed that vitamin A, as a micronutrient supplementary agent, can influence pyelonephritis occurrence. Vitamin A with retinal-derived product named retinol, several pro-vitamin A carotenoids, and retinoic acid could be used in many critical conditions (8, 9). There are several reported disorders following vitamin A deficiency, particularly impaired immunity that increases the risk of urinary tract infections (10, 11).
2. Objectives
Given that the importance of Pyelonephritis and vitamin A effect on the immune system, in this study, we aimed to investigate vitamin A potential effect on pyelonephritis treatment in children.
3. Methods
3.1. Study Design and Population
This study conducted in Amir-Kabir Hospital, Arak, Iran. We selected all female children aged between 2 - 12 years who suffered from Pyelonephritis for two years, and treated with IV ceftriaxone 75 mg/kg/day and oral cefixime 8 mg/kg for 14 days. Based on previous studies, we considered 106 children in total, assigned in treatment (n = 53) and control groups. We administrated 25,000 units of vitamin A and placebo in treatment and control groups, respectively. It should also be noted that our study was two-sided blind. For inclusion criteria, we considered pyelonephritis patients at the ages between 2 - 12 years who have no other kidney anomalies, in addition exclusion criteria were children at the age lower than 2 years, patients or their parents who have not cooperation, the children with underlying medical conditions or recurrent urinary tract infections.
3.2. Pyelonephritis Assessment
Clinical manifestations of Pyelonephritis evaluated continually during 14 days and the children information were inserted in the prepared questionnaire; 48 h after treatment, we collected urine sample from both control and treatment groups. In addition, 10 days after treatment, we performed a urine analysis as well as urine culture for further confirmation of sterile urine.
3.3. Ethical Considerations
Base on the safety of low dose vitamin A, there is no complication in this agent consumption. In addition, double publication, data fabrication, and plagiarism have been observed by the authors and approved by the Ethical Committee of Arak University of Medical Sciences.
3.4. Statistical Analysis
Data analysis was conducted by χ2 test for qualitative variables, and t-test for quantitative variables in the SPSS program and significance level (P < 0.05) were considered.
4. Results
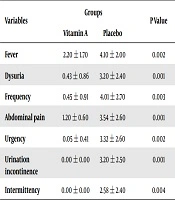
Children were equal in age and mean ± SD of age in total patients were 5.02 ± 2.40 years (treatment group = 4.60 ± 2.60 years, placebo group = 5.40 ± 2.10 years). As shown in Table 1, there were significant statistically differences between treatment and placebo groups in terms of dysuria (P = 0.001), abdominal pain (P = 0.001), frequency (P = 0.003), incontinency (P = 0.001), urgency (P = 0.002), intermittency (P = 0.004) and fever (P = 0.002). Interestingly, the duration of treatment to cut off the disease-related symptoms was substantially lower in the treatment group.
| Variables | Groups | P Value | |
|---|---|---|---|
| Vitamin A | Placebo | ||
| Fever | 2.20 ± 1.70 | 4.10 ± 2.00 | 0.002 |
| Dysuria | 0.43 ± 0.86 | 3.20 ± 2.40 | 0.001 |
| Frequency | 0.45 ± 0.91 | 4.01 ± 2.70 | 0.003 |
| Abdominal pain | 1.20 ± 0.60 | 3.54 ± 2.60 | 0.001 |
| Urgency | 0.05 ± 0.41 | 3.32 ± 2.60 | 0.002 |
| Urination incontinence | 0.00 ± 0.00 | 3.20 ± 2.50 | 0.001 |
| Intermittency | 0.00 ± 0.00 | 2.58 ± 2.40 | 0.004 |
aValues are expressed as mean ± SD.
Moreover, Table 2 showed the results of urine culture in two groups. As described in Table 2, positive U/C was 22.5% in vitamin A group and 15% in the placebo group 48 h after treatment (P = 0.001). We also took another urine culture test, 7 to 10 days after treatment. Our findings showed that positive U/C were 5.5% and 13% in vitamin A and placebo group, respectively, which implicated a statistically significant difference between two groups (P = 0.012).
| Urine Culture | Groups | P Value | |
|---|---|---|---|
| Vitamin A | Placebo | ||
| 48 hours after treatment induction | 0.001 | ||
| Positive | 12 (22.5) | 8 (15) | |
| Negative | 41 (77.5) | 45 (85) | |
| 7 - 10 days after ends of treatment | 0.012 | ||
| Positive | 3 (5.5) | 7 (13) | |
| Negative | 50 (94.5) | 46 (87) | |
aValues are expressed as No. (%).
5. Discussion
Immunological effects of vitamin A may affect the infection state in our body; therefore, in this study, we evaluated the effects of vitamin A on clinical manifestations of urinary tract infections. Notably, the results of some clinical studies were consistent with our study. For example, Yang et al. (12), evaluated the therapeutic effect of vitamin A in measles. According to their results, it could not find any significant reduction in the mortality rate in groups with vitamin A administration for children with measles (12). Another study conducted by Semba et al. (8), also assessed the efficacy of vitamin A on mortality rate in HIV-infected subjects. According to the reported results, they found that vitamin A was able to decreases the mortality rate in HIV-infected children (8).
Furthermore, Aguayo et al. (13), declared that vitamin A deficiency considered as the main risk factor in children’s survival rate. In this line, another clinical study performed on 141 severely anemic children showed that the administration of vitamin A (100000 or 200000 IU depending on age) significantly decreased the erythropoietin concentration as well as inflammation responses (14). Regarding the vitamin A effect on immune responses and clinical outcomes, there was not considerable evidence to present any desirable effect (15). A review study conducted by Wiysonge et al. (10) showed that it was about vitamin A by modulation of the immune system that could reduce the risk of transmission of HIV infection from mother-to-child. Regarding the dietary supplements mechanism of action on immune response, it has been clarified that vitamin deficiency as a malnutrition in children might have long-term effects on health, because the immune system is relatively inactive from the first hours after birth (16). The evaluation of the long-term vitamin A deficiency showed that that vitamin deficiency could be affected by poor nutrition and public health programs (17). In a case-control study, the levels of vitamin D in the study group, including 82 children with urinary tract infection (UTI) and 64 healthy participants, have been compared. The results showed that vitamin D deficiency could be one of the major risk factors for UTI in children (18). Moreover, the effect of vitamin C on urinary oxalate and pH showed that vitamin C increased the oxalate excretion as well as calcium oxalate crystallization (19). Meanwhile, it has been reported that vitamin D deficiency occurred in kidney diseases can instigate the renal inflammation (20).
5.1. Study Limitation
Limitation of our study were: (1) parental incompatibility who were convinced enough after further explanation about the importance of the issue; (2) Inability of pain assessment with quantitative scale; (3) Limited financial resource detained us to perform radiological investigation.
Overall, we recommend further studies to resolve these restrictions. In addition, despite several clinical studies carried out concerning the impact of different factors on urination management, further studies will be needed to discover any possible correlation.
5.2. Conclusions
Based on fewer side effects and higher efficacy of vitamin A, it has been suggested that vitamin A as a potential therapeutic agent could be used to treat urinary tract infection, particularly in children with vesicoureteral reflux and congenital anomalies.