1. Background
Cardiovascular disease (CVD) is a leading cause of mortality in patients with hemodialysis (HD). Many patients with end-stage renal disease (ESRD) suffer from atherosclerotic vascular events such as coronary artery disease (CAD), cerebrovascular disease, and peripheral vascular disease. These events are the main causes of mortality and morbidity (1), accounting for 44% of overall mortality in this group (2). To evaluate CAD, history taking, physical examination, electrocardiography (ECG), and cardiac biomarkers can be used (3).
The risk of myocardial ischemia or infarction is higher in patients with ESRD compared to the general population (4). Cardiac troponins (cTn) can be used to diagnose CAD (5). However, the troponin level is thought to be increased in ESRD patients without coronary events (6). There is little evidence about the relationship between ESRD and cTn level; hence, more evidence is needed to clarify this correspondence.
2. Objectives
This study aimed to investigate the correlation between ESRD and the frequency of positive cardiac troponin-I (cTnI) and the relationship between the cause of admission and positive cTnI in ESRD patients.
3. Methods
This study was extracted from an internal medicine resident thesis (398413) approved by Isfahan University of Medical Sciences (ethics code: IR.MUI.MED.REC.1398.315). In this cross-sectional study, all ESRD patients on regular dialysis [either hemodialysis (HD) or peritoneal dialysis (PD)] admitted to the wards and emergency departments of Al-Zahra and Noor-Ali Asghar university hospitals in Isfahan, Iran from January 2018 till January 2020 were enrolled. The inclusion criteria were ESRD patients aged above 18 years; being on dialysis for more than three months; checked at least once for cTn-I in the first admission; and giving an informed consent. Patients’ characteristics, including gender, age, cause of admission, cause of kidney failure, duration of dialysis, and cTn-I in the first admission were obtained from the patients’ medical charts.
Troponin level was measured in the hospital laboratories with either VIDAS high sensitive troponin I (Abbott diagnostics Ireland, Longford co., Ireland) in Al-Zahra hospital or Immunochromatographic Toyo Troponin I test (Türklab tibbi malzemeler SAN, Izmir, Turkey) in Noor-Ali Asghar hospital.
In 2000, the Consensus Committee of the European Society for Cardiology and the American College of Cardiology recommended that the diagnosis of myocardial necrosis can be made when the level of cardiac troponin is > 99th percentile of a reference control group with imprecision < 10%. The imprecision study result with the smallest measurable concentration of cTnI and an inter-lot coefficient of variation < 10% was 0.11 µg/L (7). The 99th percentile reference range value of the VIDAS Troponin I Ultra kit was 30 pg/mL. The ARCHITECT STAT High Sensitive Troponin-I assay is designed to have within-laboratory (total) imprecision of < 10% coefficient of variation (CV) with a range of 10 to 50,000 pg/mL (8). A value of more than 50 pg/mL was considered significant. The normal level of the immunochromatographic kit was less than 0.5 ng/mL (www.turklab.com.tr). The cTnI level more than 20 ng/mL was defined as significantly high.
Data were reported as frequencies and mean ± standard deviation (SD) for patients’ demographic and clinical variables. For statistical analysis, one-way analysis of variance (ANOVA) and independent sample t‑test were used to compare the cTnI level for continuous variables. Pearson correlation test was performed to find any correlation between demographic and laboratory categorical parameters with cTnI level. Multiple logistic regression analysis was used to evaluate covariates' effect on the dependent variables by using SPSS software version 23 (SPSS, Chicago, IL, USA).
4. Results
In this study, out of a total of 1,044 ESRD patients admitted to two university hospitals in Isfahan, 348 patients met the inclusion criteria and were enrolled. According to the results, diabetes mellitus (DM), hypertension (HTN), glomerulonephritis (GN), urologic and other causes of dialysis had no significant correlation with cTnI positivity. The cTnI positivity did not have any significant correlations with sex, time of dialysis, and type of dialysis, whereas age and cTnI had positive correlations (P = 0.05). Moreover, the patients admitted to Al-Zahra hospital had more positive cTnI compared to those admitted to Noor-Ali Asghar hospital (P = 0.002) (Table 1).
| Variables | cTnI Negative | cTnI Positive | P-Value |
|---|---|---|---|
| Age (y) | 57.5 ± 15.6 | 61.2 ± 17.4 | 0.05 |
| Sex | 0.3 | ||
| Male | 138 (55.6) | 59 (59) | |
| Female | 110 (44.4) | 41 (41) | |
| Cause of end-stage renal disease | |||
| Diabetes | 122 (70.9) | 50 (29.1) | 0.89 |
| Hypertension | 147 (74.2) | 51 (25.8) | 0.16 |
| Glomerulonephritis | 17 (89.5) | 2 (10.5) | 0.07 |
| Urologic | 3 (60) | 2 (40) | 0.58 |
| Other | 58 (69) | 26 (31) | 0.61 |
| Time of dialysis (mon) | 41.4 ± 44.4 | 39.2 ± 43.7 | 0.67 |
| Type of dialysis | 0.42 | ||
| Peritoneal dialysis | 36 (73.5) | 13 (26.5) | |
| Hemodialysis | 212 (70.9) | 87 (29.1) | |
| Hospital | 0.002 | ||
| Al-Zahra | 215 (68.9) | 97 (31.1) | |
| Noor-Ali Asghar | 33 (91.7) | 3 (8.3) |
Abbreviation: cTnI, cardiac troponin I.
a Values are expressed as No. (%) or mean ± SD.
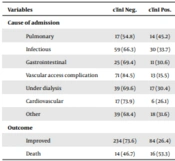
Pearson correlation test was used to evaluate the relationship between causes of admission and positive cTnI. According to the results, while pulmonary complications had positive correlations (P = 0.034), vascular access complications had negative correlations with cTnI (P = 0.002). However, other causes of admission did not have any significant effect on cTnI positivity. In addition, there was a significant correlation between the patients’ in-hospital death and more positive cTnI results (P = 0.003) (Table 2).
| Variables | cTnI Negative | cTnI Positive | P-Value |
|---|---|---|---|
| Cause of admission | |||
| Pulmonary | 17 (54.8) | 14 (45.2) | 0.034 |
| Infectious | 59 (66.3) | 30 (33.7) | 0.23 |
| Gastrointestinal | 25 (69.4) | 11 (30.6) | 0.79 |
| Vascular access complication | 71 (84.5) | 13 (15.5) | 0.002 |
| Under dialysis | 39 (69.6) | 17 (30.4) | 0.77 |
| Cardiovascular | 17 (73.9) | 6 (26.1) | 0.77 |
| Other | 39 (68.4) | 18 (31.6) | 0.60 |
| Outcome | 0.003 | ||
| Improved | 234 (73.6) | 84 (26.4) | |
| Death | 14 (46.7) | 16 (53.3) |
Abbreviation: cTnI, cardiac troponin I.
a Values are expressed as No. (%).
Multiple logistic regression analysis was used to evaluate the relation between cTnI positivity as a dependent variable and age, sex, type and time of dialysis, admission to different hospitals, causes of admission, and causes of ESRD as covariates. The results showed that only age (OR = 1.021; 95% CI = 1.005 - 1.038; P = 0.011) and admission to Al-Zahra hospital (OR = 6.107; 95% CI = 1.760 - 21.189; P = 0.004) were associated with increased cTnI positivity. In contrast, vascular access complication as a cause of admission (OR = 0.24; 95% CI = 0.123 - 0.487; P < 0.001) and HTN as a cause of ESRD (OR = 0.59; 95% CI = 0.356 - 0.993; P = 0.04) were associated with decreased positive cTnI (Table 3).
| Variables | OR | 95% CI | P-Value | |
|---|---|---|---|---|
| Lower Band | Upper Band | |||
| Age | 1.021 | 1.005 | 1.038 | 0.01 |
| Vascular access complication | 0.245 | 0.123 | 0.487 | < 0.001 |
| Hypertension | 0.595 | 0.356 | 0.993 | 0.047 |
| Glomerulonephritis | 0.235 | 0.050 | 1.101 | 0.07 |
| Hospital Al-Zahra/Noor-Ali Asghar | 6.107 | 1.760 | 21.189 | 0.004 |
Multiple logistic regression analysis was used to evaluate the patients’ outcome as a dependent factor. The results showed that factors including age (OR = 1.04; 95% CI: 1.01 - 1.07; P = 0.004) and infections as a cause of admission (OR = 3.1; 95% CI: 1.3 - 7.3; P = 0.009) were associated with increased risk of mortality. In contrary, exit site infections as a cause of admission (OR = 0.11; 95% CI: 0.01 - 0.8; P = 0.03) and hypertension as a cause of patients’ kidney failure (OR = 0.32; CI: 0.14 - 0.77; P = 0.01) were associated with decreased risk of mortality (Table 4).
| Variables | OR | 95% CI | P-Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age | 1.045 | 1.014 | 1.078 | 0.004 |
| Cardiac troponin I positivity | 2.038 | 0.890 | 4.670 | 0.092 |
| Infectious | 3.114 | 1.323 | 7.334 | 0.009 |
| Vascular access complication | 0.110 | 0.014 | 0.888 | 0.038 |
| Hypertension | 0.329 | 0.140 | 0.773 | 0.01 |
5. Discussion
Cardiac-specific troponin T (cTnT) and cTnI were incorporated in the definition of acute myocardial infarction (AMI) by the American College of Cardiology and the American Heart Association guidelines. Troponins were also considered as the preferred indicator for myocardial injury and early risk stratification of patients who presented with suspected acute coronary syndrome (ACS) (7). It was shown that the release of cardiac troponins was not only relevant to cardiac myocyte necrosis, but it was also identified in circulation in some clinical conditions without an apparent cardiac injury (9). A high level of cTnI with complementary clinical presentation and other parameters such as electrocardiogram are indicative of acute myocardial infarction (10). The application of troponins as a diagnostic agent in patients with ESRD is challenging, even though the upper reference limits were initially derived in subjects without kidney diseases (11). Moreover, the reason and the precise mechanism for cTnI elevation in HD patients is unclear (10, 12, 13).
In this cross-sectional study, the results of t-test demonstrated that age correlated with increased cTnI positivity, which was confirmed in multiple logistic regression analysis. Accordingly, for each year of increase in the patient’s age at admission, we observed a 2.1% increase in cTnI positivity. This correlation could be due to more comorbidities in elderly patients like DM, CVD, etc. Consistent with our results, Chen et al. found that age, diastolic blood pressure, and congestive heart failure were associated with an elevated cTnI level in non-ACS patients with CKD (OR = 2.30, 95% CI = 1.08, 4.88; P = 0.03) (14). However, inconsistent with our results, Taheri et al. showed that age, body mass index (BMI), and time on PD had no significant correlation with serum cTnI level on 103 ambulatory PD patients (15). This difference could be due to much more complicated patients admitted to the hospital.
The results of Pearson correlation showed more positive cTnI in patients admitted to Al-Zahra hospital than Noor-Ali Asghar hospital; this difference persisted in multiple logistic regression analysis. This is probably because Al-Zahra hospital is a referral hospital and its patients are more complicated than Noor-Ali Asghar hospital.
We also examined the relationship between positive cTnI and the cause of admission and cause of ESRD. The results of Pearson correlation illustrated that pulmonary diseases were associated with an increase in cTnI positivity, but the vascular access complications were associated with a decrease in cTnI positivity. Meanwhile, in multiple logistic regression analysis, the pulmonary diseases became ineffective, but the effects of vascular access complications persisted. This difference between the results of Pearson correlation and multiple logistic regression analysis can be due to the fact that patients with pulmonary diseases had different causes of admission, including pneumonia, pulmonary thromboembolism, chronic obstructive pulmonary disease (COPD), etc. Therefore, there were more confounding factors in Pearson correlation, which increased cTnI positivity.
While the results of Pearson correlation indicated only marginal correlations between hypertension as a cause of ESRD and cTnI positivity (P = 0.158), the results of multiple logistic regression analysis showed a threefold decrease in the risk of positive cTnI.
According to the results of Pearson correlation, in-hospital mortality was associated with more positive cTnI. However, the multiple logistic regression analysis results showed a twofold increase in cTnI positivity and mortality, but its effect was only marginal (P = 0.092). This might be due to the small sample size or the fact that most patients who died in the hospital were elderly and had more positive cTnI levels (Table 3). Similar to our results, in a study by Khan et al. conducted on 102 patients, no significant difference in all-cause hospital admissions was present between the patients with normal cTnI levels and those with elevated cTnI levels. Serum cTnI was not significantly different between patients who died versus those who survived (16).
The results of a study carried out by Hussein et al. on 93 asymptomatic HD patients showed that cTnI significantly correlated with the outcome of all‑cause mortality after one year (17).
The relationship between different factors and mortality was investigated in multiple logistic regression analysis. The results showed that infectious diseases and vascular access complications, as cause of admission, and older age and hypertension, as cause of dialysis, were associated with mortality. Therefore, infectious diseases and older age increased mortality; this may be due to the fact that these patients often were ill and had different causes such as sepsis, diabetic foot ulcer, pneumonia, etc. The vascular access complications had less mortality because most of these patients were young and were admitted with such problems as infection, obstruction, or bleeding of vascular access. Also, in multiple logistic regression analysis, hypertension as a cause of dialysis decreased mortality, which can be justified by the fact that hypertension is a protective factor in ESRD patients. In a reverse epidemiological study by Ahmadi et al., it was shown that hypertension in ESRD patients decreased mortality (18).
5.1. Conclusion
Our results show that although positive cTnI had a borderline association with in-hospital mortality in ESRD patients, further multicenter studies with a larger sample size are required to confirm the results.