1. Background
Varicocele is the abnormal tortuosity and dilation of the testicular veins (the pampiniform plexus) of more than 2 mm caused by venous reflux in the testes (1-5). Varicocele occurs primarily on the left side and is more prevalent at young ages. The prevalence of palpable varicocele is 15% in the general male population and 21% - 39% in subfertile men (6-8). Varicocele is among the most common causes of reduced sperm count and quality, leading to infertility and subfertility (9). Physical examination is the standard diagnostic method for detecting varicocele, but the diagnosis of asymptomatic and impalpable varicocele is difficult. These conditions can be detected only by using ultrasonography (3). Venous reflux is an important standard for the diagnosis of varicocele because reflux of more than 1 s increases the likelihood of infertility (10).
Color Doppler ultrasonography (CDUS) is the most sensitive, non-invasive diagnostic method for diagnosing varicocele. It has a sensitivity of 93%, while clinical examination has a sensitivity of approximately 71% (11). CDUS evaluates varicocele based on venous diameter, the presence or absence of reflux, and other relevant factors.
2. Objectives
In this study, we explored the correlation between ultrasonography (US) and semen analysis parameters.
3. Methods
This cross-sectional study was conducted in a university hospital, and the local research and ethics committee approved the research protocol. Patients with clinically confirmed or suspected varicocele (n = 134) were recruited for the study. Informed consent was obtained from each participant. Patients with secondary varicocele, traumatic injury, other pathologic disorders of the testis (e.g. tumor, hydrocele, spermatocele), or inflammation of the testis or epididymis were excluded. Using a Toshiba ultrasonography instrument (Tokyo, Japan) with a linear, multi-frequency probe (5 - 8.5 MHZ), a primary CDUS analysis was performed with all cases, and patients with venous diameters of more than 2 mm were selected for more analyses. Finally, 99 patients were selected for the study.
The selected cases were further evaluated using CDUS. The patients underwent normal scans using the Valsalva maneuver in the supine position. The evaluated parameters were the venous diameter of the pampiniform plexus, the presence or absence of venous reflux on both sides, and the longitude and transverse diameters of the testes. Reflux was quantified by duration and flow volume. Reflux of longer than 1 s was considered pathologic, while flow volume was calculated by multiplying the area by the mean velocity. Varicocele in the selected cases was classified as grade 0 (2 - 2.5 mm), grade 1 (2.5 - 3 mm), grade 2 (3 - 3.5 mm), or grade 3 (> 3.5 mm).
Then patients were referred to a laboratory for semen analysis, including semen volume and sperm morphology, count, and motility. Analysis was performed based on the world health organization laboratory manual issued in 1993 (9).
Statistical analysis was perfumed using the SPSS 17 package (Chicago, USA). The correlations between the variables were assessed using Spearman coefficients. The semen analysis parameters and CDUS findings for the samples with venous reflux of longer than 1 s and those with venous reflux of less than 1 s were compared between using student’s t-test. P-values of less than 0.05 were considered to be significant.
4. Results
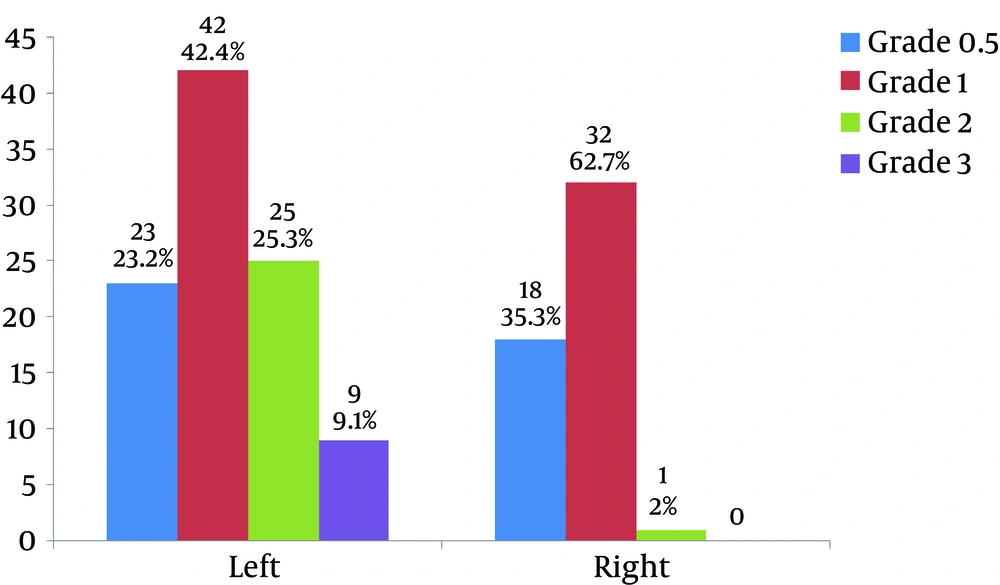
This study was performed with 99 patients with varicocele confirmed by CDUS. The mean age of the selected patients was 34.3 ± 6.2 years (range: 23 - 50 years). Among the participants, 19 had a history of cigarette smoking (19.2%), 12 a history of alcohol use (12.1%), and 9 (9.1%) a history of mumps, while 41 had a history of surgery (6 bilateral and 7 unilateral varicocele surgery). The results for testes size measured in two dimensions and varicocele size are summarized in Tables 1 and 2. All patients had left varicocele, while right varicocele was observed in 53 cases (Table 2). The average size of varicocele on the left side was significantly greater than that of right-side varicocele (P < 0.001). Additionally, the grades of varicocele on the right and left sides were recorded. Most varicocele on both sides was grade 1 (42.4%) (Figure 1).
| N | Min | Max | Mean ± SD | |
|---|---|---|---|---|
| Right testis size (L) | 99 | 19.00 | 50.00 | 41.5152 ± 4.28420 |
| Right testis size (T) | 99 | 8.00 | 29.00 | 21.9000 ± 3.87877 |
| Left testis size (L) | 99 | 23.00 | 49.00 | 40.2929 ± 4.57645 |
| Left testis size (T) | 99 | 11.00 | 29.00 | 20.8889 ± 3.35605 |
| N | Min | Max | Mean ± SD | |
|---|---|---|---|---|
| Left varicocele size | 99 | 2.00 | 4.40 | 2.8323 ± 0.54969 |
| Right varicocele size | 53 | 2 | 3.30 | 2.4047 ± 0.41721 |
We also determined sperm analysis parameters, as summarized in Table 3. The average semen volume of participants was 2.6 ± 1.2 mL, the average sperm motility was 48.9 ± 24.4%, and the average sperm count was 45.1 ± 58.2 million.
| N | Min | Max | Mean ± SD | |
|---|---|---|---|---|
| Semen volume, mL | 65 | 0.50 | 7.80 | 2.6031 ± 1.22219 |
| Total sperm motility, % | 83 | 0.00 | 96.00 | 48.8955 ± 24.37332 |
| Normal sperm morphology, % | 83 | 0.00 | 83.00 | 16.0635 ± 17.86094 |
| Count (× 106) | 86 | 0.00 | 437.00 | 45.0556 ± 58.24126 |
The correlation between the sperm analysis parameters and varicocele or testes size was calculated. The correlation coefficients between varicocele size and sperm count in the left and right testes were -0.6 and -0.7, respectively (P = 0.001). The correlation coefficients between varicocele size and sperm motility in the left and right testes were -0.61 and -0.78, respectively (P = 0.035). The correlation coefficients between varicocele size and abnormal sperm morphology in the left and right testes were 0.53 and 0.74, respectively (P = 0.04). The correlation coefficient between varicocele size and semen volume in the left and right testes was -0.61 (P = 0.045). The correlation coefficients of testes size with sperm count, sperm motility, abnormal sperm morphology, and semen volume were 0.35 - 0.49, 0.3 - 0.48, 0.25 - 0.45, and 0.15 - 0.25, respectively (P = 0.3).
Seventy-one (71) of 99 patients with left varicocele (71.7%) had reflux of longer than 1 s, while 14 of 53 patients with right varicocele (26.4%) had reflux of longer than 1 s. The sperm analysis parameters, varicocele size, and testes size were compared between the samples with reflux of longer than 1 s and reflux of less than 1 s in each testis (Tables 4 and 5). For the left testis, the groups had significant differences in semen volume, motility, morphology, and count (P < 0.05) but not testis size (P > 0.05). Patients with reflux had significantly greater varicocele size than patients without reflux (P < 0.05) (Table 4).
| Left Varicocele Reflux of Longer Than 1 s | N | Mean ± SD | P Value |
|---|---|---|---|
| Volume | 0.045 | ||
| No | 20 | 2.9 ± 1.3 | |
| Yes | 61 | 2.1 ± 1.1 | |
| Total motility | 0.03 | ||
| No | 22 | 60.8 ± 24.9 | |
| Yes | 64 | 40.7 ± 23.9 | |
| Morphology | 0.04 | ||
| No | 21 | 12.7 ± 16.3 | |
| Yes | 63 | 22.5 ± 19.6 | |
| Count | 0.02 | ||
| No | 25 | 55.8 ± 33.7 | |
| Yes | 60 | 32.4 ± 76.5 | |
| Right testis size 1 | 0.6 | ||
| No | 28 | 41.7 ± 4.5 | |
| Yes | 71 | 41.3 ± 4.0 | |
| Right testis size 2 | 0.36 | ||
| No | 28 | 23.9 ± 13.9 | |
| Yes | 71 | 22.0 ± 3.1 | |
| Left testis size 1 | 0.3 | ||
| No | 28 | 40.8 ± 4.1 | |
| Yes | 71 | 39.8 ± 5.6 | |
| Left testis size 2 | 0.38 | ||
| No | 28 | 21.2 ± 2.8 | |
| Yes | 71 | 20.6 ± 3.9 | |
| Left varicocele size | < 0.001 | ||
| No | 28 | 2.5 ± 0.4 | |
| Yes | 71 | 3.2 ± 0.5 |
| Right Varicocele Reflux of Longer Than 1 s | N | Mean ± SD | P Value |
|---|---|---|---|
| Right testis size (L) | 0.25 | ||
| No | 85 | 41.8471 ± 3.52375 | |
| Yes | 14 | 39.5000 ± 7.28275 | |
| Right testis size (T) | 0.31 | ||
| No | 85 | 23.4235 ± 10.88618 | |
| Yes | 14 | 20.4286 ± 4.73472 | |
| Left testis size (L) | 0.45 | ||
| No | 85 | 40.4353 ± 4.36285 | |
| Yes | 14 | 39.4286 ± 5.82718 | |
| Left testis size (T) | 0.42 | ||
| No | 85 | 21.0000 ± 3.16228 | |
| Yes | 14 | 20.2143 ± 4.44070 | |
| Left varicocele size | 0.088 | ||
| No | 85 | 2.7941 ± 0.54097 | |
| Yes | 14 | 3.0643 ± 0.56515 | |
| Right varicocele size | 0.04 | ||
| No | 39 | 2.3397 ± 0.45914 | |
| Yes | 14 | 2.5857 ± 0.17913 |
Similar findings were obtained for 14 patients with reflux of longer than 1 seconds on the right testis. For right-side varicocele, varicocele size was significantly greater in patients with reflux than patients without reflux (P < 0.05). Right testis size was not significantly different between the two groups (P > 0.05) (Table 5).
In this investigation, the cut-off point for diagnosis of varicocele was 2 mm and had acceptable sensitivity but not adequate specificity. Therefore, we decided to select a cut-off point with higher specificity, PPV, and NPV. Using statistical analysis, we determined that 2.6 mm was a reliable cut-off value to more effectively detect varicocele.
5. Discussion
We showed that semen analysis parameters, including semen volume and sperm morphology, count, and motility, had significant correlations with varicocele diameter but not testes size.
One study (12), which compared sperm analysis data and CDUS findings for 62 patients with varicocele, did not find any significant correlations between the analyzed parameters. This discrepancy with present results can be related to technical faults because ultrasonography is an operator-dependent technique. In addition, semen analysis results depend on the quality of the laboratory tools and technician’s skills.
Two studies (13, 14) found that patients with spermatogenesis disorder had smaller testes. Although the present research also found a relationship between testes size and spermatogenesis disorder, this relationship was not statistically significant, which might be due to the lack of a standard method for measuring testes size in this study.
In the present results, patients with reflux of longer than 1 seconds and those with reflux of less than 1 seconds had significantly different semen analysis parameters and varicocele size. Similar findings were reported by (15), who found a significant correlation between bilateral reflux and persistent reflux with sperm abnormalities.
Our inclusion criterion was varicocele diameter of more than 2mm, resulting in the exclusion of 35 men with a history of infertility from the study. However, further analysis revealed that a cut-off point of 2.6 mm in the supine position during the Valsalva maneuver was more reliable and efficient at detecting patients with varicocele (14) used a cut-off point of 2.48 mm in the standing position without the Valsalva maneuver.
We recommend that patients with a varicocele diameter of less than 2 mm be evaluated for venous reflux because reflux can occur without increasing the diameter of the pampiniform vein.