1. Background
End-stage of renal disease (ESRD) has become a global public health challenge because of high prevalence of cardiovascular diseases (CVD) and premature death (1-6). Patients with ESRD have lower quality of life and shorter life expectancy compared with individuals of the same age in the general population (4). Studies have shown the association between metabolic syndrome (MeS) and increased risk of CVD (7). According to Adult Treatment Panel (ATP) III criteria (8), a person with three or more of the following criteria can clinically be considered as having MeS: 1) abdominal obesity, waist circumference > 102 cm in men and > 88 cm in women; 2) hypertriglyceridemia, triglyceride (TG) ≥ 150 mg/dL (1.695 mmol/L); 3) low high-density lipoprotein (HDL) cholesterol < 40 mg/dL (1.036 mmol/L) in men and < 50 mg/dL (1.295 mmol/L) in women; 4) high blood pressure (≥ 130/85 mm Hg); and 5) high fasting blood glucose (FBS) (≥ 110 mg/dL). Identifying MeS has several advantages. Some researchers consider MeS a multiple risk factor for CVD (8, 9) that its diagnosis will help treatment of important causes of CVD (10). However, there are those who disagree (11, 12). The role of MeS in the CHD in hemodialysis (HD) population has not been meticulously studied.
2. Objectives
The aim of this study was to see whether MeS caused adverse cardiovascular events (CVEs) in patients on HD.
3. Patients and Methods
This study was conducted during March 2012 in four HD centers affiliated with Shahid Beheshti University of Medical Sciences, Tehran, Iran, and in two HD centers affiliated with Zanjan University of Medical Sciences, Zanjan, Iran. We studied the presence of MeS in 300 patients on HD (173 males (57.7%) and 127 females (42.3%)), with the mean age of 61.7 ± 14.2 years. In this study, MeS was defined according to ATP III criteria (8). The subjects were divided into two groups regarding presence of MeS criteria. All of the patients gave informed consent prior to data collection. Subjects were given a questionnaire to provide demographic data and medical histories. To assess CHD, we used the medical records of patients with chest pain and change of electrocardiogram (ECG), lab test, and wall motion abnormalities by ECG at cardiac care unit (CCU) admission. Moreover, serum predialysis blood urea nitrogen (BUN), creatinine (Cr), fasting blood sugar (FBS), hemoglobin (Hb), albumin (Alb), cholesterol, TG, phosphor (P), and calcium (Ca) were measured. The two groups’ measurements were compared. All examination and laboratory values were collected when the patients had reached their dry weight following the start of maintenance dialysis.
In addition, waist circumference was measured at 1 cm above the umbilicus at the end of HD session. The subjects who were administered antihypertensive medications were considered to have hypertension (HTN); the individuals who were administered antidiabetic medication were considered to have diabetes mellitus (DM). KT/V was used to evaluate the efficacy of dialysis. The level of blood pressure was recorded before and after HD. Duration of dialysis, age, and sex as well as the causes of ESRD were extracted from the patients’ medical records and were used for the final analysis. The HD protocol for all patients was four hours of using hemophane membrane with an average blood flow rate of 300 to 350 mL per minute and with bicarbonate-basis dialysate. The median duration of dialysis was 48 months (range, 12 to 192 month). Subjects were excluded if they were assumed to have a life expectancy of less than six months or unwilling to sign informed consent.
3.1. Statistical Analysis
Normal distribution of data was assessed by the Kolmogorov-Smirnov test using Lilliefor’s correction. The results were expressed as mean ± SD, frequency (percentage) or median (range). Comparison of demographic and clinical characteristics between those subjects with and without MeS was performed by Student’s t-test, Chi squared test and/or the Mann-Whitney U test. Differences in the proportions of categorical secondary outcome events between those with and without MeS were evaluated by the Chi squared test. Multiple logistic regression-derived odds ratios (OR) and 95% CI were calculated to describe the associations between MeS and the variables. All data were analyzed by SPSS 18.0 (SPSS Inc, Chicago, Illinois, the United States). P < 0.05 were considered statistically significant.
4. Results
A total of 300 patients on HD including 173 males (57.7%) and 127 females (42.3%), with mean age of 61.7 ± 14.2 years, were enrolled. Out of the 300 subjects, 156 patients (52%) had DM and 251 (83.7%) had HTN. The participants’ general characteristics are presented in Table 1. The cause of ESRD in the subjects were as follows: HTN in 103 patients (34.3%), diabetic nephropathy in 109 (36.3%), chronic glomerulonephritis in 11 (3.6%), polycystic kidney disease in 14 (4.7%), urological problem in 9 (3%), poisoning in 1 (0.33%), autoimmune diseases in 3 (1%), and idiopathic in 53 (17.7%).
Prevalence of MeS was 50.3% (151 patients). Characteristics of study participants with MeS are shown in Table 2. The most common element of MeS was HTN (135 patients (89.4%)), followed by DM (117 patients (77.5%), low HDL cholesterol (116 patients (76.8%)), evidence of abdominal obesity (102 patients (67.5%)), and elevated TG (85 patients (56.3%)). Moreover, MeS was significantly associated with sex (Table 3). Its prevalence was 40.5% (70 patients) in males and 68.8% (81 patients) in females (P < 0.0001). However, MeS was not significantly associated with patient’s age.
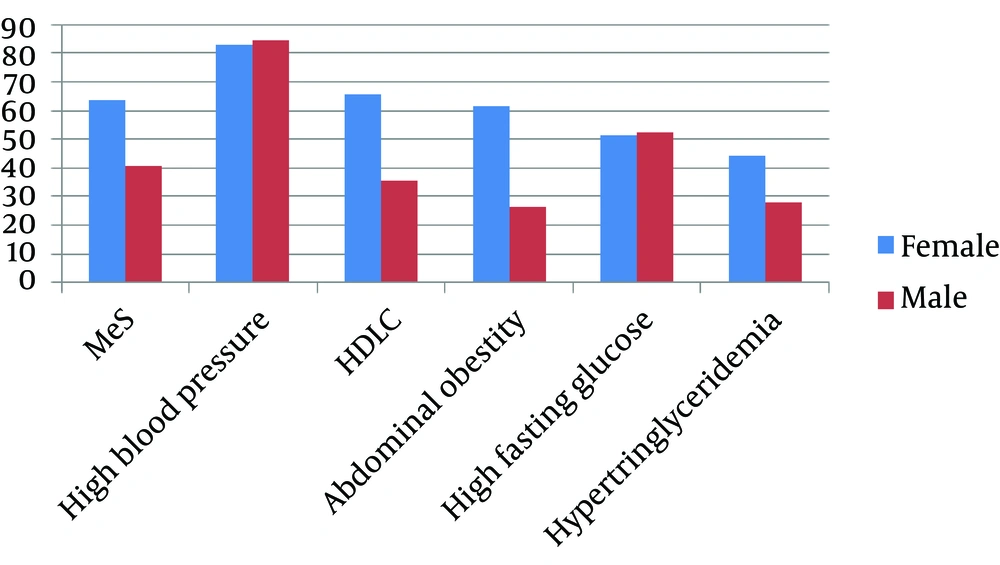
Figure 1 displays the frequency of components of MeS in patients on HD according to sex. Patient’s sex did not show significant association with abnormality in glucose metabolism (P = 0.86), but prevalence of low HDL was significantly higher in females than in males (65.4% vs. 35.8%; P < 0.001). In addition, MeS was not significantly associated with age and duration of HD and was not significantly associated with BUN, Cr, Ca, P, immunoreactive parathyroid hormone (iPTH), Alb, Hb, iron, total iron binding capacity (TIBC), ferritin, C-reactive protein (CRP), and Kt/V.
During the study, the CHD occurred more frequently in patients with MeS (42 patients (27.8%)) than in those without MeS (21 patients (14.1%)) (P = 0.004). The rate of death due to CHD was 28.6% (12 patients) in those with MeS and 23.8% (5 patients) in those without MeS, showing no significant differences (Table 2). In addition, stroke happened more frequently in the MeS group (46 patients (30.5%)) than in those without MeS (26 patients (17.4%)) (P = 0.008). The rate of death due to stroke was 28.3% (13 patients) in the MeS group and 23.1% (6 patients) in those without MeS, showing no significant differences (Table 2).
Table 4 shows the rate of CVEs and causes of death in both groups. The mean number of criteria for MeS was significantly associated with the history of stroke (2.91 ± 1.2 vs. 2.49 ± 1.3; P = 0.014), but it was not associated with the history of CHD (2.84 ± 1.1 vs. 2.5 ± 1.3; P = 0.08). The mean number of criteria for MeS was not significantly associated with mortality causes (CHD, 2.7 ± 1.3; stroke, 2.8 ± 0.9; and other causes, 2.9 ± 1.3; P = 0.78). In addition, among the MeS criteria, HTN (89.3%, 25 patients) and DM (53.8%, 15 patients) were associated with an increased risk of mortality (Tables 5-6).
The rate of HTN was 84.4% in males (146 patients) and 82.7% in females (105 patients), while the rate of DM was 52.6% among males (91 patients) and 51.2% among females (65 patients). There was no significant difference between male and female subjects in CHD and death occurrence. Logistic regression showed that patients with MeS had history of HTN (OR, 5.3; 95% CI, 2.67-10.52; and P < 0.001), history of DM (OR, 2.9; 95% CI, 1.49-5.72;and P = 0.002), higher body mass index (OR, 1.1; 95% CI, 1.02-1.19; and P = 0.018), and higher TG (OR, 1.01; 95% CI, 1.008-1.02; and P < 0.001), and were mostly female (OR, 2.53; 95% CI, 1.38-4.63; P = 0.003) (Table 7). In the MeS group, CHD were not significantly associated with serum Alb, Ca-P product, iPTH, Hb, platelet, iron, CRP, uric acid, BUN, Cr, and KT/V; nonetheless, there was significant association with white blood cell count (P = 0.002) (Table 3).
| Variable | Value |
|---|---|
| Age, y | 61.7 ± 14.2 |
| Sex | |
| Female | 127 (42.3) |
| Male | 173 (57.7) |
| Diabetes mellitus | 156 (52) |
| Metabolic features | |
| Hypertension | 251 (83.7) |
| Systolic BP, mm Hg | 132.3 ± 22.3 |
| Diastolic BP, mm Hg | 77.1 ± 11.4 |
| Low HDLC | 145 (48.3) |
| Abnormal glucose metabolism | 140 (46.7) |
| Elevated triglycerides | 102 (34) |
| Obesity | 124 (41.3) |
| Serum laboratory features | |
| HDLC, mmol/L | 1.16 ± 0.27 |
| FBG, mmol/L | 6.74 ± 3.42 |
| Cholesterol, mmol/L | 4.08 ± 1.09 |
| Triglyceride, mmol/L | 1.69 ± 1.02 |
| Blood Urea Nitrogen, mmol/L | 27.38 ± 16.06 |
| Creatinine, μmol/L | 769.08 ± 221.00 |
| Sodium, mmol/L | 138.8 ± 3.5 |
| Potassium, mmol/L | 5.21 ± 0.7 |
| Calcium, mmol/L | 2.26 ± 0.18 |
| Phosphorus, mmol/L | 1.58 ± 0.39 |
| Hemoglobin, mmol/L | 114 ± 76 |
| Albumin, mmol/L | 41 ± 23 |
| Ferritin, mmol/L | 1386.00 ± 1612.89 |
| CRP, nmol/dL | 190.48 [0-1142.88] |
| KT/V | 1.21 ± 0.25 |
| Duration of treatment with hemodialysis, mo | 48 [12-192] |
| WBC | 6.4× 109/L (2.5 × 109/L-15.7 × 109/L) |
| PLT | 178 × 109/L (67 × 109/L-623 × 109/L) |
| iPTH, ng/L | 244.5 [8-2000] |
| Fe, μmol/L | 13.75 [3.40-39.56] |
| TIBC, μmol/L | 51.10 ± 10.95 |
| AST, µkat/L | 0.30 [0.07-3.52] |
| ALT, μkat/L | 0.28 [0.08-2.29] |
| Serum Uric acid, µmol/L | 416.40 ± 88.63 |
a Data are presented as mean ± SD or No. (%), or median [range].
b Abbreviations: ALT, alanine transferase; AST, aspartate transferase; BP, blood pressure; CRP, C-reactive protein; FBG, fasting blood glucose; Fe, iron; HDLC, high-density lipoprotein cholesterol; iPTH, immunoreactive parathyroid hormone; PLT, platelet; TIBC, total iron binding capacity; and WBC, white blood cell.
| Variables | Metabolic Syndrome | P Value | |
|---|---|---|---|
| No (n = 149) | Yes (n = 151) | ||
| Sex | < 0.0001 | ||
| Female | 46 (30.9) | 81 (53.6) | |
| Male | 103 (69.1) | 70 (46.4) | |
| Age, y | 65 [20-90] | 65 [36-84] | 0.18 c |
| Diabetes mellitus | 39 (26.2) | 117 (77.5) | < 0.0001 |
| Metabolic features | |||
| Hypertension | 116 (77.9) | 135 (89.4) | 0.007 |
| Systolic BP, mm Hg | 130 [80-200] | 130 [90-200] | 0.43 c |
| Diastolic BP, mm Hg | 80 [50-100] | 80 [50-110] | 0.88 c |
| Low HDLC | 29 (19.5) | 116 (76.8) | < 0.0001 |
| Abnormal glucose metabolism | 34 (22.8) | 106 (70.2) | < 0.0001 |
| Elevated triglycerides | 18 (12.1) | 85 (56.3) | < 0.0001 |
| Abdominal obesity | 22 (14.8) | 102 (67.5) | < 0.0001 |
| Body mass index, kg/m2 | 22.9 ± 3.7 | 25.2 ± 4.2 | < 0.0001 |
| Serum laboratory features | |||
| FBS, mmol/L | 4.88 [3.33-24.98] | 6.83 [3.05-21.15] | 0.39 c |
| Cholesterol, mmol/L | 3.82 ± 0.86 | 4.35 ± 1.23 | < 0.0001 |
| HDLC, mmol/L | 1.26 ± 0.25 | 1.06 ± 0.26 | < 0.0001 |
| Triglyceride, mmol/L | 1.45 [0.43-7.55] | 1.23 [0.59-5.76] | < 0.0001 |
| Blood urea nitrogen, mmol/L | 23.56 [6.78-92.46] | 21.74 [6.07-89.96] | 0.46 c |
| Creatinine, μmol/L | 777.92 ± 238.68 | 751.40 ± 203.32 | 0.22 |
| Sodium, mmol/L | 139.1 ± 3.6 | 138.5 ± 3.4 | 0.17 |
| Potassium, mmol/L | 5.3 ± 0.8 | 5.13 ± 0.6 | 0.08 |
| Calcium, mmol/L | 2.28 ± 0.18 | 2.23 ± 0.18 | 0.12 |
| Phosphorus, mmol/L | 2.56 ±0.42 | 1.58 ± 0.36 | 0.82 |
| iPTH, ng/L | 254 [11-2000] | 225.5 [8-1516] | 0.245 |
| Hemoglobin, g/L | 108 ± 2 | 107 ± 17 | 0.68 |
| WBC | 6 × 109/L (2.76 × 109/L-12.26 × 109/L) | 6.66 × 109/L (2.56 × 109/L-15.76 × 109/L) | 0.002 c |
| PLT | 1766 × 109/L (806 × 109/L-6236 × 109/L) | 1806 × 109/L (676 × 109/L-5016 × 109/L) | 0.602 |
| Fe, μmol/L | 13.60 [3.40-37.95] | 13.96 [4.48-39.56] | |
| TIBC, μmol/L | 52.57 ± 9.81 | 49.49 ± 11.87 | 0.01 |
| Ferritin, mmol/L | 1208.44 [26.90-5605] | 890.07 [29.15-4232.90] | 0.056 c |
| CRP | 20 [0-120] | 0 [0-120] | 0.075 c |
| AST, μkat/L | 0.30 [0.07-1.60] | 0.30 [0.08-3.52] | 0.738 |
| ALT, μkat/L | 0.28 [0.12-2.29] | 0.28 [0.08-2.29] | 0.47 |
| Albumin, g/L | 41 ± 6 | 39 ± 5 | 0.61 |
| Uric acid, μmol/L | 421.75 ± 93.39 | 410.45 ± 83.28 | 0.28 |
| KT/V | 1.18 ± 0.25 | 1.24 ± 0.24 | 0.06 |
| Duration of treatment with hemodialysis, mo | 48 [12-192] | 36 [12-144] | 0.412 c |
| History of MI | 21 (14.1) | 42 (27.8) | 0.004 |
| History of Stroke | 26 (17.4) | 46 (30.5) | 0.008 |
| Death | 44 | 56 | 0.576 |
| MI | 14 (31.8) | 14 (25) | |
| Stroke | 5 (11.4) | 10 (17.9) | |
| Others (Sepsis, Cancer, Cirrhosis, Pneumonia, GIB, unknown) | 25 (56.8) | 32 (57.1) | |
a Data are presented as mean ± SD or No. (%) or median [range].
b Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; BP, blood pressure; CRP, C-reactive protein; FBG, fasting blood sugar; Fe, iron; GIB, gastrointestinal bleeding; HDLC, high-density lipoprotein cholesterol; iPTH, immunoreactive parathyroid hormone; MI, myocardial infarction; PLT, platelet count; TIBC, total iron binding capacity; WBC, white blood cell.
cMann Whitney U test.
| Variables | Female (n = 127) | Male (n = 173) | P Value |
|---|---|---|---|
| Metabolic syndrome | 81 (63.8) | 70 (40.5) | < 0.0001 |
| Age, y | 62.4 ± 13.5 | 61.2 ± 14.7 | 0.48 |
| Diabetes mellitus | 65 (51.2) | 91 (52.6) | 0.81 |
| Metabolic features | |||
| Hypertension | 105 (82.7) | 146 (84.4) | 0.69 |
| Systolic BP, mmHg | 130 [80-200] | 130 [90-200] | 0.19 c |
| Diastolic BP, mmHg | 80 [50-100] | 80 [50-110] | 0.71 c |
| Low HDLC | 83 (65.4) | 62 (35.8) | < 0.0001 |
| Elevated triglycerides | 56 (44.1) | 47 (27.2) | 0.002 |
| Abnormal glucose metabolism | 60 (47.2) | 80 (46.2) | 0.86 |
| Abdominal obesity | 78 (61.4) | 46 (26.6) | < 0.0001 |
| Body mass index, kg/m2 | 24.2 ± 4.6 | 23.9 ± 3.7 | 0.67 |
| Serum laboratory features | |||
| FBS, mmol/L | 5.44 [3.05-21.15] | 5.38 [3.39-24.98] | 0.39 c |
| Cholesterol, mmol/L | 4.41 ± 1.13 | 3.85 ± 1.00 | < 0.0001 |
| HDLC, mmol/L | 1.21 ± 0.33 | 1.12 ± 0.22 | 0.003 |
| Triglyceride, mmol/L | 1.45 [0.43-7.55] | 1.23 [0.59-5.76] | 0.001 c |
| Blood urea nitrogen, mmol/L | 23.56 [6.78-92.46] | 21.74 [6.07-89.96] | 0.46 c |
| Creatinine, μmol/L | 7.7.20 ± 203.32 | 804.44 ± 221.00 | < 0.0001 |
| Sodium, mmol/L | 138.80 ± 3.5 | 138.84 ± 3.5 | 0.93 |
| Potassium, mmol/L | 5.13 ± 0.7 | 5.27 ± 0.7 | 0.11 |
| Calcium, mmol/L | 2.28 ± 0.18 | 2.25 ± 0.18 | 0.28 |
| Phosphorus, mmol/L | 1.55 ± 0.29 | 1.58 ± 0.42 | 0.19 |
| iPTH, ng/L | 231 [8-1919] | 248 [11-2000] | 0.32 |
| Hemoglobin, g/L | 108 ± 18 | 107 ± 18 | 0.68 |
| WBC | 6.4× 109/L (2.7 × 109/L-14.8 × 109/L) | 6.4 × 109/L (2.5 × 109/L-15.7 × 109/L) | 0.934 |
| PLT | 182 × 109/L (67 × 109/L-450 × 109/L) | 175 × 109/L (80 × 109/L-623 × 109/L) | 0.249 |
| Fe, μmol/L | 13.96 [4.48-39.56] | 13.43 [3.40-33.29] | 0.99 |
| TIBC, μmol/L | 49.83 ± 10.81 | 52.05 ± 10.99 | 0.08 |
| Ferritin, mmol/L | 1208.44 [26.90-5605] | 890.07 [29.15-4232.90] | 0.56 c |
| CRP | 0 [0-120] | 20 [0-120] | 0.296 |
| AST, μkat/L | 0.32 [0.08-1.06] | 0.28 [0.07-3.52] | 0.34 |
| ALT,μkat/L | 0.28 [0.08-1.92] | 0.28 [0.28-2.29] | 0.22 |
| Albumin, g/L | 41 ± 6 | 39 ± 5 | 0.14 |
| Uric acid, μmol/L | 404.50 ± 71.38 | 422.34 ± 9 | 0.06 |
| KT/V | 1.22 ± 0.3 | 1.21 ± 0.3 | 0.74 |
| Duration of treatment with hemodialysis, mo | 48 (12-144) | 39.6 (12-192) | 0.423 |
| History of MI | 26 (20.5) | 37 (21.4) | 0.84 |
| History of Stroke | 35 (27.6) | 37 (21.4) | 0.216 |
| Death, n | 46 | 54 | 0.55 |
| MI | 13 (28.3) | 15 (27.8) | |
| Stroke | 5 (10.9) | 10 (18.5) | |
| Others (sepsis, cancer, cirrhosis, pneumonia, GIB, unknown) | 28 (60.9) | 29 (53.7) |
a Data are presented as mean ± SD or No. (%) or median [range].
bAbbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; BP, blood pressure; CRP, C-reactive protein; FBG, fasting blood sugar; Fe, iron; GIB, gastrointestinal bleeding; HDLC, high-density lipoprotein cholesterol; iPTH, immunoreactive parathyroid hormone; MI, myocardial infarction; PLT, platelet count; TIBC, total iron binding capacity; WBC, white blood cell.
cMann Whitney U test.
| Variables | With Metabolic syndrome | Without Metabolic Syndrome | ||||||
|---|---|---|---|---|---|---|---|---|
| Female (n = 81) | Male (n = 70) | OR | 95% CI | Female (n = 46) | Male (n = 103) | OR | 95% CI | |
| History of MI | 18 (22.2) | 24 (34.3) | 0.5 | 0.26-1.12 | 8 (17.4) | 13 (12.6) | 1.45 | 0.5-3.8 |
| History of stroke | 26 (32.1) | 20 (28.6) | 1.18 | 0.5-2.3 | 9 (19.5) | 17 (16.5) | 1.23 | 0.5-2.4 |
| Cause of death | ||||||||
| No. | 35 | 21 | 11 | 33 | ||||
| MI | 9 (25.7) | 5 (23.8) | 4 (36.3) | 10 (30.3) | ||||
| CVA | 4 (11.4) | 6 (28.6) | 1 (9.1) | 4 (12.1) | ||||
| Others c | 22 (62.9) | 10 (47.6) | 6 (54.5) | 19 (57.6) | ||||
a Data are presented as No. (%).
b Abbreviations: OR, odds ratio; CVA, cardiovascular accident; GIB, gastrointestinal bleeding; and MI, myocardial infarction.
cSepsis, Cancer, Cirrhosis, Pneumonia, gastrointestinal bleeding, and Unknown.
| Variables | n | Metabolic Syndrome Criteria, No. | |||||
|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | ||
| History of MI | 63 | 0 | 10 (15.9) | 11 (17.5) | 25 (39.7) | 13 (20.6) | 4 (6.3) |
| History of stroke | 72 | 0 | 11 (15.3) | 15 (20.8) | 24 (33.3) | 13 (18.1) | 9 (12.5) |
| Cause of death | |||||||
| MI | 28 | 0 | 5 (17.9) | 9 (32.1) | 6 (21.4) | 5 (17.9) | 3 (10.7) |
| Stroke | 15 | 0 | 1 (6.7) | 4 (26.7) | 6 (40) | 4 (26.7) | 0 |
| Others c | 57 | 0 | 8 (14) | 17 (29.8) | 11 (19.3) | 14 (24.6) | 7 (12.3) |
a Data are presented as No. or No. (%).
b Abbreviations: CVA, cardiovascular accident; GIB, gastrointestinal bleeding; and MI, myocardial infarction.
cSepsis, Cancer, Cirrhosis, Pneumonia, gastrointestinal bleeding, and Unknown.
| Death due to | No. | HTN | DM | Abdominal | HDL | TG |
|---|---|---|---|---|---|---|
| MI | 28 | 25 (89.3) | 15 (53.8) | 16 (57.1) | 12 (42.8) | 8 (28.5) |
| Stroke | 15 | 15 (100) | 8 (53.3) | 5 (33.3) | 10 (66.7) | 5 (33.3) |
| Others c | 57 | 52 (91.2) | 39 (68.4) | 28 (49.1) | 28 (49.1) | 19 (33.3) |
a Data are presented as No. or No. (%).
b Abbreviations: DM, diabetes mellitus; HDL, high-density lipoprotein; HTN, hypertension; MI, myocardial infarction; and TG, triglyceride.
cSepsis, Cancer, Cirrhosis, Pneumonia, gastrointestinal bleeding, Unknown.
| Variables | Beta | Standard Error | P Value | Odds Ratio | 95% CI | |
|---|---|---|---|---|---|---|
| History of Hypertension | 1.66 | 0.35 | < 0.001 | 5.3 | 2.67 | 10.52 |
| History of Diabetes | 1.07 | 0.34 | 0.002 | 2.9 | 1.49 | 5.72 |
| Gender | 0.92 | 0.31 | 0.003 | 2.53 | 1.38 | 4.63 |
| BMI | 0.95 | 0.4 | 0.018 | 1.1 | 1.02 | 1.19 |
| TG | 0.014 | 0.003 | < 0.001 | 1.01 | 1.008 | 1.02 |
| Age | 0.005 | 0.1 | 0.65 | 1.005 | 0.98 | 1.03 |
| FBS | 0.005 | 0.003 | 0.12 | 1.005 | 0.99 | 1.01 |
a Abbreviations: BMI, body mass index; FBS, fasting blood glucose; and TG, triglyceride.
5. Discussion
The CVD affects patients with ESRD and is the leading cause of death in patients on dialysis (13, 14). Increased risks of CVEs in patients on dialysis could be partially explained by traditional and nontraditional cardiovascular risk factors (15-19). Numerous studies have shown MeS to be a significant risk factor for CVD, mortality, and chronic kidney disease (CKD) in the general population (15, 17-20). MeS is a way of approaching traditional CVD risk factors. Secondary therapy can help prevent morbidity and mortality associated with CHD in the general population (17, 21). In addition, MeS has been shown to be an independent predictor of CVD mortality in patients with type 2 DM (22, 23).
Because some usual risk factors associated with the general population have an inverse survival association in the maintenance of dialysis population (24), we decided to evaluate the correlation of the MeS with CHD in patients on HD. There are a few reports about the incidence of MeS among HD population (14, 25). The prevalence of MeS in stages 4 and 5 CKD population in the Australian population is reported to be less than 20% (26). Hamada et al. reported the metabolic syndrome incidence rate of 62% in patients on HD (74.4% in females, 52.7% in males) (25). Stolic et al. demonstrated that approximately 30% of patients on HD had MeS (27). In one of our earlier studies, the prevalence of MeS among patients on HD was 28.7% (39.1% in females, 60.9% in males) (28).
In the present study, we studied a larger sample size. Moreover, the sample included patients on HD from two different geographical regions. The prevalence of MeS was 50.3%, which might be due to larger sample size. Bakker et al. reported that the most common element of MeS was HTN, 85% of subjects had HTN while 46% had DM (29). In the present study, we obtained similar results (89.4% had HTN; 77.5%, DM).
MeS has important preventive implications for certain group of patients. CVD and all-cause mortality has been shown to increase in middle-aged Finnish men with MeS (17). Data from NHANES II (National Health and Nutrition Examination Survey) show that incidence rate of CHD, CVD, and total mortality were increased in the United States adult population with MeS (13). Our study showed that sex had an effect on the rate of MeS, but CHD and mortality due to CHD were not affected by sex (Table 3).
Johnson et al. have shown (30) that MeS happens in 30.5% of patients with stages 4 and 5 CKD. It is also associated with older age and a significant increase risk of future CVEs. However, our study showed that occurrence of MeS was not associated with age. In addition, age was also not associated with the occurrence of CHD and mortality due to CHD (Table 3). Data in patients with type 2 DM are contradictory. Bonora et al. demonstrated that MeS was associated with a significant increase in CVD risk in patients with type2 DM (30). Yet another study showed that identification of MeS in patients with type 2 DM did not improve CVD mortality (22, 23). In the present study, the incidence rate of MeS in patients with DM was 75% (117 patients) and the incidence rate for CHD was 26.5% (31 patients). Among the subjects without MeS, the rate of DM and CHD were 39% (39 patients) 10.3% (4 patients), respectively. Moreover, CHD occurred more frequently in patients with DM and MeS (P = 0.035).
Another study demonstrated that treatments targeting hypercholesterolemia, hyperhomocysteinemia, anemia, and mineral metabolism bone disorder could not adequately explain the increase in cardiovascular risk among patients with CKD and MeS (31). In our study, CVEs were not significantly associated with serum Alb, Ca-P product, BUN, Cr, CRP, ferritin, and KT/V. In our study, MeS occurred in 50.3% of the subjects. The risk of future CHD and occurrence of stroke significantly increased in the MeS group in comparison with those without MeS. There was no significant difference between these two groups in terms of death rate due to CHD and stroke. Hypercholesterolemia, anemia, and bone mineral metabolism disorder had no role in development of CHD and stroke in patients with MeS in the HD population.
The mean number of criteria for MeS was significantly associated with the patients’ history of stroke, but it was not associated with the patients' history of CHD. The mean number of criteria for MeS was not significantly associated with the cause of mortality. Sex had an effect on the rate of MeS in our study population, but it did not have an association with CHD occurrence in the MeS group. Moreover, MeS was not significantly associated with age. Future studies could help determine the prevalence of MeS in the ESRD population and the viability of MeS to predict CVD, CHD morbidity and mortality in ESRD patients.
The limitations of the present study were the prevalence rates of MeS in the general population and in the early stage of patients with CKD as they were unavailable for comparison. Being free of CHD was not documented as coronary angiography was not performed in all patients. The follow-up duration was not sufficient to assess cardiac mortality.