1. Background
The prevalence of chronic kidney disease (CKD) is increasing in many countries. This condition is a crucial public health problem. More than 50 million people worldwide have CKD and over 1 million of this population require dialysis and kidney transplantation (1). Patients undergoing hemodialysis (HD) have multiple problems. In the earlier stages of this condition low physical activity begins and gets worse toward the end-stages (2-5). The process of hemodialysis itself induces catabolism (6) Therefore, resistance exercise can help to inhibit this catabolism (7). Hemodialysis treatment is usually an ongoing long-life treatment, which is prescribed twice a week and each session lasts 3 - 6 hours. In combination with muscle wasting, malnutrition is another problem in these patients and studies showed that hemodialysis patients consume less than the recommended daily intake of protein, which is 1 - 1.2 g/kg of body weight daily (8-12). These factors will reduce their physical performance and activity, thus their quality of life decreases and their mortality rates will increase (13-15).
The effectiveness of dialysis or dialysis adequacy is an important standard for evaluating hemodialysis patients. Also, measuring this standard is a crucial goal to all healthcare teams. Parameters like kt/V (k: urea clearance; t: time of dialysis and V: distribution of water or urea) and urea reduction ratio (URR) are among the important issues (10). Based on the guidelines of the international investigations on dialysis outcomes performed by national kidney foundation dialysis outcomes quality initiative (NKF-DOQI) and renal physician association (RPA), kt/V is a better assessment in comparison to URR for dialysis adequacy. According to RPA guideline on adequacy, the recommended kt/v should be at least 1.2 and URR higher than 65% (10). Intradialytic exercise can increase kt/V of these patients (16). Although it is not as effective as increasing HD time for increasing kt/v, some patients cannot tolerate these prolonged sessions. Nevertheless, this exercise did increase phosphate reduction rate (17).
Intradialytic exercises could lead to a higher dialysis efficiency and this means a higher quality of life in these patients (18). Interestingly, intradialytic exercises could be better than non-intradialytic exercises because adherence is better. Moreover, resistance exercise can increase muscle mass and strength. It also can reduce muscle weakness in these patients (7). Dialysis patients need to improve their physical fitness until they can perform the suggested levels of physical activity (19). “The use of intradialytic exercise, as a novel and efficient use of time during HD, is well established in Australia and some European nations”; therefore, we can implement this kind of treatment as a “medicine” for these patients (20). Low dialysis adequacy is associated with high mortality rates and better nutrition intake and exercise can help to reduce this effect (10, 16). What completes the diet is called “supplement” (21). Oral nutritional supplements are products in various forms of powder, liquid, pudding, etc. (22-24) that contain nutrients, including carbohydrates, proteins (amino acid), fats (fatty acids and glycerol), salt, minerals, vitamins, and enzymes (25, 26). Various studies suggest consumption of oral nutritional supplements in these patients to increase their nutritional intake and dialysis adequacy (2, 10, 27).
The combination of exercise and dietary amino acid can lead to better results in these patients (2, 18). Until now no studies have investigated the effect of intradialytic isometric resistance training and supplementation with BCAA on kt/V and URR score of these patients.
2. Objectives
This study aimed to investigate the effect of isometric resistance training and supplementation with BCAA on dialysis adequacy in patients undergoing dialysis.
3. Methods
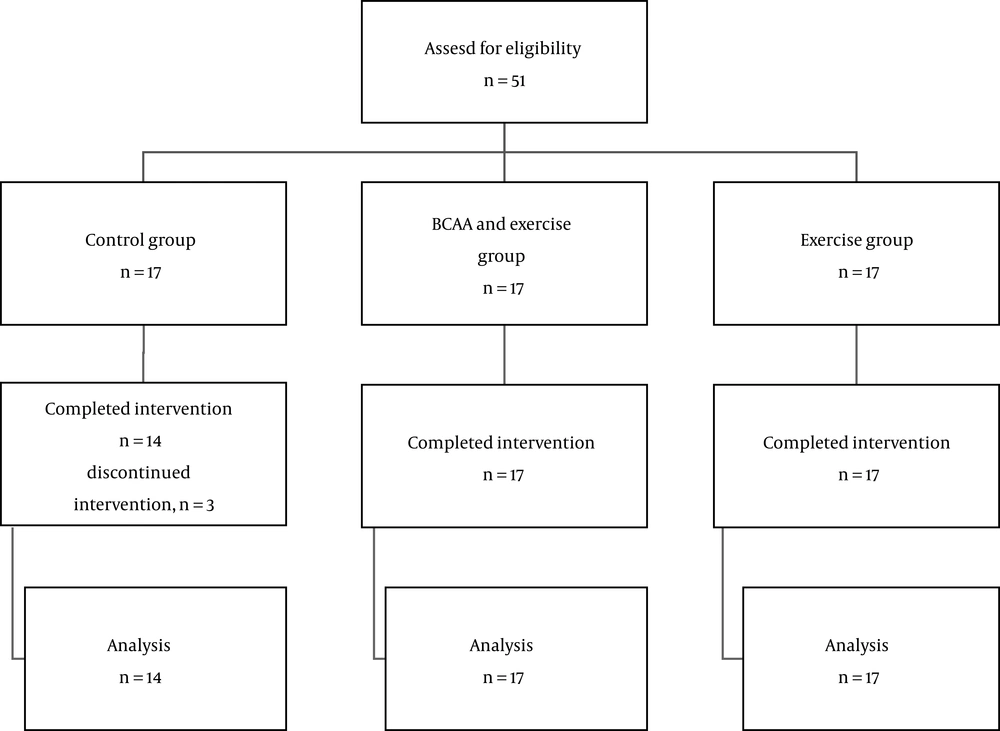
The present study was a clinical trial and was conducted in Baqiyatallah Hospital in Tehran. A total of 51 patients were randomly divided into three exercise (EX), exercise and BCAA (EXBCAA), and control groups and the number of the subjects in each group was 17 patients (Figure 1). The inclusion criteria for participation in this study were the patients over eighteen, no severe cardiovascular problem, no severe infections, patients who had undergone hemodialysis for a at least six months; no unknown chronic disease, cancer, nephritic syndrome, no chronic liver disease, hepatitis B or C, no recent infections, no neurologic related diseases, no recent surgery during the last three months, as well as the lack of parenteral nutrition and oral supplements.
3.1. Ethical Considerations
IR.SSRI.REC.1396.127 and IRCT2017101014998N2 codes are the ethical code and the Iranian Registry of Clinical Trials code, respectively. We received the ethical code from the Physical Education and Sports Science Research Center for this study. After coordination with hospital administrators and research committee of Baqiyatallah University of Medical Sciences, the study process started by complete explanation to the patients and caregivers and the aim of the study was explained. Also, they filled and signed written informed consent forms.
3.2. Measurement Tools and Method
Personal data, including height, net weight, age, gender, marital status, education, the reason for dialysis, and dialysis treatment duration, were collected using a demographic questionnaire. For patients who had problems such as vision complications or needed help in any way to complete the questionnaire, the questionnaire was read and the answers were recorded without any changes or judgment. Dialysis adequacy rate was measured by determining kt/V, which was calculated using the Daugirdas II and URR equations (28). The kt/V is a ratio that shows the volume of cleared plasma over urea distribution volume as follows:
Ln, natural logarithm; R, ratio of post-dialysis blood urea nitrogen (BUN) to predialysis BUN (R = BUN2/BUN1); T, duration of each dialysis session; UF, ultrafiltration volume; W, weight after dialysis.
3.3. Interventions
Before the intervention, in all of the three groups, the patients’ height was measured in centimeters and their body weight was recorded using a Seca scale (with an accuracy of 100 g). After the patients were placed in beds, about 4 mL of their blood was taken for blood urea nitrogen (BUN) and creatinine (Cr) tests before they were connected to the dialysis machine. Their body mass index (BMI) was calculated by dividing the body weight (kg) by the square of height (m2). After the dialysis session, the second sampling was done for the BUN test, and the patients were weighed again. An arterial needle was used for blood sampling before dialysis, and the blood pump speed was reduced to approximately 50 - 100 mL/min for 10 - 20 s for sampling after dialysis. Then, the blood pump was stopped, and the blood sample was taken from the arterial line (10). Before starting the intervention, adequacy of dialysis was determined by kt/V and URR of the patients. Patients were explained about the exercise plan on the first day of the intervention. After the first 30 minutes of hemodialysis session, the exercise program was begun; isometric handgrip contraction was the first exercise, we used a plastic ring grip and the patients contracted their plastic rings for ten seconds. After the first exercise, which activated the muscles in their arms, the second part of the exercise was performed. This was ten seconds of isometric contraction and raising the legs from the bed while the patients were lying on the hospital beds, in this part of exercise quadriceps and abdominal muscles were active. The starting point of the exercise program was 10 seconds; each week 2 - 4 seconds of contraction was applied as overloading based on the capability of the patients. The longest time of contraction was 20 seconds; at first 10 sets were performed for each session, which gradually increased to 15 sets. With nephrologist supervision, BCAA were given to participants in EXBCAA group and they were prescribed 6 g of BCAA per day. The BCAA was made by Karen pharma and food supplement company, which is an approved food and supplement company by Iran food and drug administration. The patients were reminded daily and in their exercise sessions so that do not forget to take their supplements. If patients had any questions regarding the exercise and supplement, the project executive was responsible for answering. Moreover, exercise and nutrition counseling was given throughout the intervention. Subsequently, blood samples were taken again at the end of the first and second months of the intervention, and kt/V and URR were assessed.
3.4. Statistical Analysis
The Kolmogorov-Smirnov test was used for testing the normal distribution of data. Also, the one-way analysis of variance (ANOVA) test was used for analyzing the data. The SPSS version 22 was the software used for all of the statistical analyses. The minimum significant level was 0.05.
4. Results
In this study, 48 patients completed the study. Three patients out of seventeen were excluded from the control group because one of them underwent surgery and two of them admitted to other hospitals. The most prevalent complications reported by the patients were gastrointestinal problems such and tablets were hard to swallow. It was recommended that a lower dosage like 4 - 5 grams could be well tolerated and gradually increase it to 6 grams. Here, 28 patients (58.3%) were male with an average age of 60.9 years and 23 patients (41.7%) were female with an average age of 61.4 (Tables 1 and 2). All of the three groups were homogeneous based on URR and kt/V in the pre-test (Table 3). However, at four weeks of intervention in both kt/V and URR variables, a significant difference was observed between the groups (P = 0.001 for kt/V) (P = 0.003 for URR) (Table 3) and at eight weeks of intervention (P = 0.02 kt/v and URR) (Table 3). EXBCAA group, which received amino acids and performed intradialytic isometric resistance exercise, had the most effective improvements. In this regard, their kt/V and URR improved 20% and 12.5% at 8 weeks of intervention, respectively (Table 3). EX group also had a 14% improvement in their kt/V score and 7% in URR at 8 weeks of intervention (Table 3). Control group had a non-significant decline in kt/v score.
Abbreviations: BMI, body mass index; HD, hemodyalisis; SD, standard deviation.
aValues are expressed as mean ± SD.
| Parameter | EXa | EXBCAAa | Controla | ANOVA |
|---|---|---|---|---|
| Before intervention | ||||
| Kt/v | 1.11 ± 0.04 | 1.10 ± 0.12 | 1.15 ± 0.08 | F = 0.37; P = 0.69 |
| URR | 59.13 ± 5.16 | 58.51 ± 7.29 | 58.83 ± 4.06 | F = 0.20; P = 0.83 |
| At 4 weeks | ||||
| Improvements in % compared with baseline | +8% kt/v; +5% URR | +15% kt/v; +9% URR | -5% ktv | |
| Kt/v | 1.20 ± 0.11 | 1.27 ± 0.08 | 1.09 ± 0.07 | F = 7.16; P = 0.001 |
| URR | 61.91 ± 8.16 | 63.38 ± 5.05 | 58.03 ± 8.11 | F = 6.97; P = 0.003 |
| At 8 weeks | ||||
| Improvements in % compared with baseline | +14% kt/v; +7% URR | 20% ktv; 12% URR | -4% ktv | |
| Kt/v | 1.26 ± 0.14 | 1.33 ± 0.12 | 1.10 ± 0.02 | F = 4.95; P = 0.02 |
| URR | 63.33 ± 6.33 | 65.73 ± 6.76 | 59.05 ± 7.10 | F = 4.77; P = 0.02 |
aValues are expressed as mean ± SD.
5. Discussion
The purpose of the present study was to investigate the effect of eight weeks of intradialytic isometric training and BCAA supplementation on dialysis adequacy of hemodialysis patients. None of the groups showed a significant difference regarding quantitative or qualitative variables as well as kt/V or URR. Before the intervention, all of the patients in this study had kt/V scores lower than 1.2, which showed low dialysis adequacy, for each 0.1 decrease in kt/V score, mortality rates were increased by 7% and for each 5% decrease in URR, mortality rates were increased by 11% (10). Our result showed that isometric exercise during the dialysis session and receiving BCAAs could increase kt/V score by 0.23 and URR by 7%. However, this improvement in the exercise only group was lower; hence, kt/V increased by 0.14 and URR by 4%. These improvements sound to be related to the increase of blood flow to the working muscles, and exercise during dialysis can open the surface area of capillaries; therefore, increases the urea flux from the exercised tissue to the vascular system. Thus serum urea can be cleared more efficiently and this will improve the dialysis efficacy (29). Although other studies examined the effect of aerobic and combined exercise in these patients (7, 13, 29), none of those studies examined the isometric resistance exercise, which is one of the most efficient forms of a simple exercise that can be done during a dialysis session. These findings showed that exercise during the dialysis could be used as adjunctive therapy to make dialysis more efficient. Our previous study showed that intradialytic isometric resistance exercise could improve the albumin levels as well as handgrip strength. These results can also indicate the importance of exercise because albumin and handgrip strength are also linked to mortality rates and exercise can improve them (18). Our study demonstrates that a regular exercise program during dialysis supervised by an exercise physiologist, with a duration of 30 minutes and patients’ RPE of 13 - 16 can improve dialysis adequacy. Some studies have measured the effects of intradialytic exercise on dialysis efficacy urea removal. Paluchamy et al. investigated the kt/V changes to a 12-week intradialytic exercise program and observed that kt/V was increased significantly (16). Also, the result of Mohseni et al. study, which examined the effect of a 15-minute aerobic session combined with flexion of joints and other movements on dialysis adequacy for 8 weeks, revealed a 38% significant improvement in kt/V score (29). These studies are in agreement with our results of 20% increase in kt/V score. Our findings also support Afaghi et al. and Bolasco et al. findings. In fact, their study showed that receiving oral amino acids could also increase dialysis adequacy (10, 27). We observed better results by combining the exercise and supplements. This method agrees with Majchrzak et al. (2) who showed that the group, which performed the exercise and received the supplement, had a significantly higher muscle protein turnover versus the supplement only group. In another study, Bessa et al. (7) showed the exercise, especially resistance exercise during the dialysis session, is beneficial in improving clinical and biochemical markers. More recent studies suggest the use of intradialytic exercises for these patients to help them achieve a better quality of life and more efficient dialysis process (30, 31).
5.1. Conclusions
The findings of the present study indicate that intradialytic isometric resistance exercise and supplementation with BCAA can increase kt/V and URR in hemodialysis patients, which prove an increase in dialysis adequacy. consequently, higher dialysis adequacy may be a great help to these patients.