1. Background
Nephrotic syndrome is defined as some signs and symptoms that result from damage to the basal membrane of the kidney glomeruli. This syndrome is characterized by a manifestation of glomerular nephrotic proteinuria, with high levels of hypoalbuminemia, edema, hyperlipidemia, and protein loss in urine (1). Nephrotic proteinuria is defined as a protein excretion of more than 40 mg/m2 of body surface per hour or a protein-to-creatinine ratio of more than 2 - 3 in the first morning urine sample. Its incidence in most Western countries is 2 - 3 cases per 100,000 children per year, and in underdeveloped countries it is often higher due to malaria (2, 3).
Nephrotic syndrome is divided into several categories in response to treatment, one of them is relapse of nephrotic syndrome, which is referred as reperfusion of proteinuria with edema 28 days after completion of treatment (4). The next category is drug-dependent nephrotic syndrome, which is a recurrence of proteinuria at the time of dose reduction or up to 28 days after complete discontinuation (5). Another category is drug resistant nephrotic syndrome, which means no response to treatment after 8 weeks of initial treatment and the last category is recurrent nephrotic syndrome, which is the 4 or more times of relapses of nephrotic syndrome in 1 year (6, 7). Now, based on the high prevalence of nephrotic syndrome, lack of full effectiveness of steroid treatments, the side effects of these drugs, and due to previous limited studies on the role of this drug in the course of the disease and its inconsistent results, we conducted a study and evaluated the impact of vitamin D on nephrotic syndrome as an alternative treatment.
2. Objectives
The aim of this study was to evaluation the efficacy of vitamin D consumption on nephrotic syndrome condition.
3. Methods
3.1. Study Setting
Patients were evaluated in Amir Kabir Hospital, Arak, Iran.
3.2. Study Population
In total, 30 patients with nephrotic syndrome were evaluated as study group, these cases were patients with nephrotic syndrome confirmed by a pediatric urologist.
3.3. Measurement
In this study, all patients diagnosed with nephrotic syndrome were enrolled in study. The disease was assessed by measuring the amount of urinary protein (proteinuria as excretion of protein more than 40 mg/m2), per hour or protein to creatinine ratio more than 2 - 3 to 1 as defined in the first morning urine sample).
In this study, in addition to the usual treatment of nephrotic syndrome in these patients, vitamin D was used as a treatment, in which vitamin D was in the form of a 4,000 unit ampule with a volume of 1 cc and dissolved in 5 cc olive oil, and was injected. The amount of used drug depended on the age of the patients and their vitamin D level. In children under 2 years with vitamin D levels less than 2, one thousand units, in children under 2 years with vitamin D levels of 2 to 3, 5 thousand units, in children over 6 years with vitamin D levels below 2, 4 thousand units and in children above 7 years, with vitamin D levels as 2 to 3, 5,000 units of this drug were used.
The drug was administered within 1 hour for 1 cc every hour and then 6 months later vitamin D levels were checked and their nephrotic syndrome status was assessed and the two indices were compared. Initially, the patients were evaluated through interviews and demographic questionnaires. Urinary protein levels were measured to evaluate the renal status of nephrotic syndrome. The general treatment for patients with nephrotic syndrome based on prednisolone was that of children with nephrotic syndrome taken at the start of a CBC and then for each child 60 mg/m2/day prednisolone (maximum dose 80 mg/m2/day) was prescribed for 4 - 6 weeks. After 6 weeks in response to appropriate treatment (no protein excretion in urine for 3 consecutive days determined by urine test every 2 weeks) the dose of prednisolone was reduced to 40 mg/m2/day. We followed patients for 2 months, so based on patient response to treatment, nephrotic syndrome type was determined. The results of patients' evaluation before and after treatment were analyzed by SPSS software and a final report was presented.
3.4. Ethical Considerations
In this study for the total period of research and treatment of patients, the study group adhered to the principles of medical ethics announced by the Ministry of Health and the Helsinki Declaration and approved by the Medical Ethics Committee of Arak University of Medical Sciences, with ethical code as IR.ARAKMU.REC.1397.271, and IRCT code as IRCT20130518013366N11.
3.5. Statistical Analysis
In this study, statistical analysis was performed by SPSS software. After normalizing the data, we used chi-square test to compare pre and post treatment status in patients with nephrotic syndrome.
4. Results
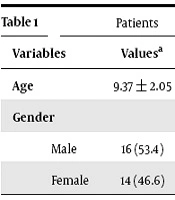
The mean and standard deviation of age was 9.37 ± 2.05 years, also regarding the gender of patients, 14 cases were female, and 16 cases were male (Table 1).
| Variables | Valuesa |
|---|---|
| Age | 9.37 ± 2.05 |
| Gender | |
| Male | 16 (53.4) |
| Female | 14 (46.6) |
aValues are expressed as mean ± SD or No. (%).
In addition, analysis of the results 2 months after treatment of patients with nephrotic syndrome showed that the level of vitamin D has no significant correlation with nephrotic syndrome, based on this, regarding the response to treatment in patients with low level of vitamin D, 3 patients (20%) had mild, 10 patients (66.6%) had moderate and 2 patients (14%) had severe nephrotic syndrome. In the group with normal levels of vitamin D, 3 patients (20%) had mild, 11 (73.3%) patients moderate and 1 patient (6%) had severe nephrotic syndrome (Table 2).
| Serum Vitamin D Level | Severity of Nephrotic Syndromea | P Value | ||
|---|---|---|---|---|
| Mild | Moderate | Severe | ||
| < 30 | 3 (20) | 10 (66.6) | 2 (14) | 0.827 |
| > 30 | 3 (20) | 11 (73.3) | 1 (6) | |
aValues are expressed as No. (%).
5. Discussion
In this study we observed that vitamin D consumption did not have a considerable effect on improving the clinical status of patients with nephrotic syndrome. However in other studies there are some other results that be discussed in the following.
Jafar et al. in a study about vitamin D enzyme polymorphisms in children, examined the prevalence of vitamin D receptor deficiency in idiopathic nephrotic syndrome and reported that 108 children with untreated nephrotic syndrome and 569 healthy children had normal vitamin D receptors (8), accordingly, their results also indicate the importance of using this drug with vitamin D in these patients. In another study, Muske et al. evaluated the effect of 400 and 1000 unit doses of vitamin D on bone mass index and recurrent type of nephrotic syndrome and found that higher doses of vitamin D had higher effects on these patients (9). However, we have not evaluated different doses of this vitamin in our evaluation. In addition Bak et al. evaluated the prophylactic effect of vitamin D and calcium on nephrotic syndrome and concluded that this vitamin had therapeutic effects but had no side effects (10), whereas we did not examine the therapeutic effect of calcium in our evaluation. In a study to evaluate the efficacy of vitamin D in nephrotic syndrome, Gulati et al. evaluated children in both the intervention and control groups and reported that vitamin D had a positive effect on nephrotic syndrome (11), which correlated with the results of our evaluation. Weng et al. in a study, also assessed vitamin D deficiency in children with nephrotic syndrome and found that this deficiency in nephrotic syndrome was not correctly identified (12).
In addition, Huttunen et al. examined various aspects of nephrotic syndrome and found that in one of these patients, abdominal edema and tenderness were present and in all cases more than half of the patients were diagnosed before 2 months of age. They died before the age of 6 months and most of them did not last more than 2 - 3 months. In 14 cases, elevated serum creatinine and urinary nitrogen levels were observed (13). Esfehani et al. have also studied and observed a long term clinical outcome study of 745 children with steroid sensitive nephrotic syndrome from 1996 to 2006. They mentioned that 63.1% of patients were male. Focal Segmental Glumerulosclerosis (25%) was the most common histopathology in minimal change nephrotic syndrome (30.2%) (14). However, the indices evaluated in our study were somewhat different from these results, due to differences in the methods used in the two assessments. Accordingly, the importance of using new and better drugs with lower complications for treatment of nephrotic syndrome were cleared, which necessitates more studies in this field.
5.1. Conclusions
Based on our results, vitamin D consumption did not have a meaningful effect on improving the clinical status of patients with nephrotic syndrome. Based on this we cannot improve nephrotic syndrome in patients with this condition.