1. Context
Infertility is a failure in getting pregnant after one year of regular sexual interaction without using of the contraceptive methods (1). The prevalence of infertility in couples of fertility ages has been estimated to be over 15% and has increased in recent decades (2, 3). Many environmental factors can reduce a male's fertility. Male fertility disorder may appear as a decrease in sperm count, mobility disorder, or structural disorder. Its causes include biochemical factors, stress, ionizing radiation, and electromagnetic waves (1). In addition, cellphones are one of the devices that emit low levels of RF (radiofrequency) in the microwave range when they are in use (4). Nowadays, over 700 million cellphone users are in the world. In different countries and areas, the cellphones produce varied frequencies. Telephone, digital phone, and third-generation phones produce respectively 450 - 900 MHz, 850 - 1900 MHz, and almost 2000 MHz (5). The SAR (specific absorption rate) values always decrease when the skin is exposed to the cellular radio antenna, or this cellular radio antenna passes through the skin. Tissues that are close to mobile devices are more susceptible to damage than the tissues that are distant from cellular antennas. Therefore, keeping a cellphone in your pants pocket can lead to male sperm infertility because they are near the reproductive organs, especially the testicles where sperms are produced and stored. Moreover, the use of cellphones in the long-term may have adverse outcomes on the sperm motility (6). Generally, energy during irradiation can absorb testicular tissues; this EMW (electromagnetic wave) easily converts to thermal energy and can disrupt sperm production, which eventually results in a reduction of sperm numbers and results in infertility. This heat energy can also reduce sperm motility, which can play a role in infertility. If sperm velocity is reduced, access to the female ovary may become difficult during ovulation (7, 8). The EMWs produced from cellphones are thought to interfere with normal spermatogenesis; thus, it reduces the quality of sperm. Some reports express that motility of sperm reduces due to mobile phone usage (7, 9). Studies on the animals show that testicular and germ cell function in men may have a variety of deleterious influences from EMWs. Dasdage et al. reported no effect of cellphone use on the rat testis, while Davoudi et al. observed a progressive sperm velocity deceleration in a small study group regarding cellphone usage the (9, 10). However, in modern social life, the use of mobile devices or computer Wi-Fi has increased significantly in the last two years (11, 12), and male infertility is also a contemporary problem. Infertile men are characterized by abnormal semen characteristics (13).
2. Objectives
The purpose of this research was to examine men's infertility due to the effect of radiofrequency waves.
3. Methods
In this systematic review, no language restrictions were considered in searching the databases. PubMed, Cochrane Library (Wiley), Scopus MEDLINE (Ovid), EMBASE, Google Scholar, ProQuest, Science Direct, and CINAHL (EBSCO) were used to obtain the data from them). The data were collected from the year 2000 until 5 July 2019. In all articles, references and reports were confirmed. Global Thesis & ProQuest Thesis and the International Clinical Trials Registry Platform were included as gray literature. Medical terms were used to obtain the data as well as "RF", "RF-EMFs", "phone", "mobile phone", "radiofrequency, "cellphone", "electromagnetic field", "electromagnetic waves", "EMF"," EMW", "male", "men", "sperm" as keywords. The studies were evaluated for study inclusion by their title and abstracts. Evaluation of the article was done, and any disagreement over articles was resolved by authors through the discussions. Articles were evaluated to fit the purpose of this systematic review. For searching, any observational reproductive system was used. The search study designs were included to confirm that all related articles were included. Some articles were excluded, such as case studies, case series, reviews, and letters to editor. Inaccurate and insufficient articles were excluded. This study contained all articles with or without a control group. Studies with infertile pairs that were defined by failure in getting pregnant after one year of regular sexual interaction without the use of the contraceptive methods in males and females with an age range from 18 to 65 and studies with device usage that were emitting the RF-EMF for different exposures were included in this systematic review. Moreover, researchers who used different procedures of examination to measure the reproductive system, hormonal valuations, spermatograms, recognition imaging procedures, and biopsies were included. Only studies on humans and interference by using any device that exposed a user to RF-EMFs for any frequency and period were included in this systematic review. No restrictions were applied on exposure time, type of device, exposure condition, location of users, and distance for methodological validation. Two independent referees examined the papers that were selected for retrieval before evaluating the quality of cohort studies using the Newcastle-Ottawa Scale and evaluating the nonrandomized controlled trials using CONSORT (14). Disagreements on the review were resolved by discussion or with a third reviewer. The extracted data include precise details about the interferences, populations, study approaches, and outcomes that are essential to the purposes of the review.
4. Results
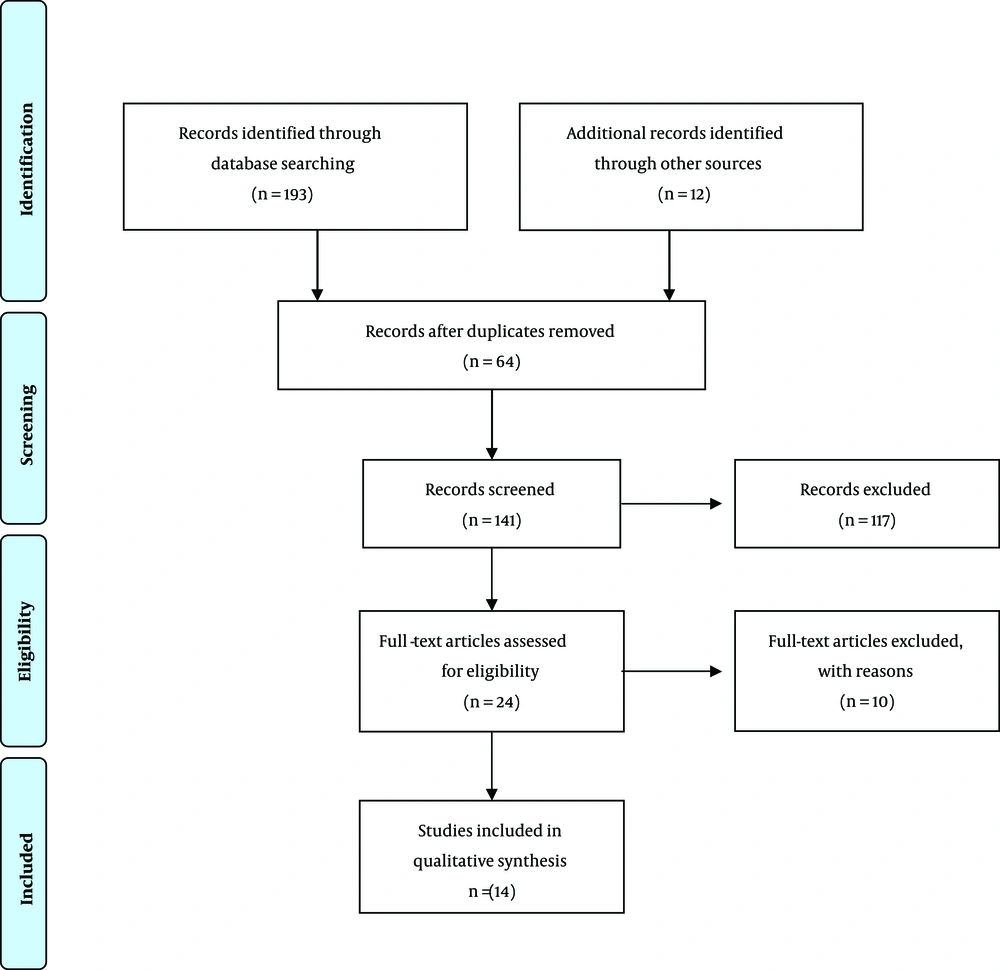
After searching the various databases, 205 articles were reviewed. According to the title and abstract, 181 unrelated articles were performed in vitro or on animals, and after reviewing the full text of the articles, 64 articles were removed due to duplication. Finally, 14 articles were included in this study (Figure 1). Table 1 displays the characteristics of the studies included.
| Author (Year) | Region | Purpose | Type of Study | Sample Size | Measure | Participant Characteristics | Key Findings | Quality Score |
|---|---|---|---|---|---|---|---|---|
| Dkhil et al., 2011 (15) | Libya | The effect of the EMR on sperm function | RCT | 20 healthy donors | Sperm analysis | Mobile use | EMR can decrease vitality, and motility of sperm | 7 |
| Fejes et al., 2005 (7) | Hungary | The relationship between cellphone use and semen quality | Retrospective case- control | 371 infertile men | Semen analysis | Mobile use | Cellphone use was negatively associated with the rate of rapid progressive sperm motility | 9 |
| Zhang et al., 2016 (16) | Chine | The effect of cellphone use on semen parameters | Prospective cohort from | 872 young men | Semen analysis | Mobile use | Mobile use is related to decreased sperm count, semen volume, total sperm count, and sperm concentration | 9 |
| Sajeda and Al-Watter, 2011 (17) | Iraq | The effect of mobile phone use on semen analysis | Cross-sectionalcase- control | 300 infertile men | Semen analysis/serum testosterone measurement | Mobile use | Mobile use is related to a decrease in sperm count, motility, and morphology. | 7 |
| Agarwal et al., 2008 (5) | USA | the impact of mobile phone usage on quality of semen | observational | 361 infertile men | Semen analysis | Cellphone use | Cellphone use related to a decrease in sperm count, motility, viability, and morphology | 8 |
| Shaeer et al., 2013 (18) | Cairo | The effect of mobile radiofrequency waves on the quality of semen in infertile men | Retrospective case-control | 316 infertile men | Semen analysis | Cellphone use and Bluetooth use | Mobile phones decreased the sperm motility, progressive motility and abnormal morphology. | 9 |
| Gutschi et al., 2011 (19) | Austria | The impact cellphone use on semen parameters | Retrospective | 2110 men referred to infertility clinic | Semen analysis, free testosterone, FSH, LH and PLT. | Use of mobile phones | Use of mobile phones can decrease morphology, fast progressive sperm motility and LH. Use of mobile phones increases testosterone level. | 7 |
| Rago et al., 2013 (20) | Italy | The semen quality in call phone user | Observational | 63 healthy and fertile men from 250 participants | Semen analysis | Use of mobile phones | There is a significant positive relationship between mobile phone use and DNA fragmentation | 8 |
| Mostafa et al., 2012 (21) | Egypt | The effect of exposure to RF-EMR on semen quality and DNA damage | Case-control | 100 infertile men | Semen analysis | Mobile usage time | Use of mobile phones correlated to significant decrease in sperm motility ratio, progressive motile sperms and immotile sperm | 8 |
| Al-Bayyari, 2017 (22) | Jordan | The effect of mobile use on the quality of semen | Observational cross sectional | 159 men | Semen analysis | Mobile usage | Mobile usage increased abnormal morphology and reduced semen volume, sperm count and immobilized sperm. | 7 |
| Wdowiak et al, 2007 (1) | Poland | Determination usage effect of cellular phones on the fertility of males | Observational cross sectional | 304 infertile men | Semen analysis | Mobile usage | Mobile usage was associated with a decrease in normal sperm motility and an increase in sperm grade motility | 9 |
| Yildirim et al, 2015 (23) | Turkey | To assess the effects of RF-EM on sperm parameter | Observational cross sectional | The 1082 men | Semen analysis | Use of mobile and mobile internet. | Wireless internet use related to decrease in total removable sperm, total progressive removable sperm count. There was a negative association between duration of cellphone use and wireless internet with total sperm count | 8 |
| Lewis et al., 2017 (24) | USA | To relationship between mobile phone use patterns and semen quality | Longitudinal cohort | 348 infertile men | Semen analysis | Use of mobile | Cellphones increase the total number of removable sperm | 8 |
| Feijo et al., 2011 (25) | Brazil | The association between cellular phones use and sperm parameters | prospective | 571 healthy men | Semen analysis | Mobile use segmentation | Cellular phone use affected by sperm count, progressive motility, viability and morphology. | 7 |
4.1. Volume
In the first study, a comparison of three groups (less than 30 min, between 3 min and 2 hours, more than 2 hours) showed that volume was not influenced by cellphones (P = 0.194) and the internet (P = 0.43) by usage duration (23). In the second study, a significant negative relationship was observed between cellphone usage duration and volume of semen (-8.37; 95% CI, -15.93, -0.13) (26). The volume of sperm in men who kept cellphones in their trouser pocket differed from those who kept mobile phones in the waist pocket and shirt pocket (16). The duration of daily exposure to cellphone was not related to volume (16). Men who use their cellphone elsewhere may have a significant increase in their semen volume; no pattern encountered, and sustainable response between cellphone use and semen volume (24). Reduction of semen volume was observed in those living less than 1 km from the telecommunication tower (22).
4.2. Total Sperm Count
In the first study, a comparison of three groups (less than 30 min, between 3 min and 2 hours, more than 2 hours) showed total sperm count was not influenced by cellphone (P = 0.074) and internet (P = 0.093) usage duration (23). In the second study, a significant negative relationship was observed between cellphone usage duration and the total number of sperms (β coefficient -8.23; 95% CI, -14.38, -1.63) (26). No correlation was found between mobile phone usage duration and total sperm count (r = -0.20) (20). There were not any significant differences in terms of sperm count (P = 0.404) between those who kept their cellphone in their pocket or their belt holder among infertile men (18). A significant decrease in sperm count was observed with the increase of daily use of cellphone in infertile men (5). Men who kept cellphones in their pant pocket showed a significant decrease in sperm count in comparison with those keeping mobile phones in the waist pocket and shirt pocket (16). The duration of daily exposure to cellphone was not related to sperm count (16). Reduction of sperm count was observed in those who texted more than 20 min daily (22). An increase in the daily use of mobile phones significantly reduced the number of sperm per ejaculate (21). There was not any encounter patterns/sustainable response between mobile use and total sperm count (24).
4.3. Sperm Concentration
A significant negative relationship was observed between cellphone usage duration and sperm concentration [β coefficient = -6.32%, 95% confidence interval (CI), -11.94, -0.34 (24) in men who kept cellphones in the pant pocket, showing a significant decrease in sperm concentration in comparison with those keeping mobile phones in their waist pocket and shirt pocket (16). The duration of daily exposure to cellphone was not related to sperm concentration (16).
4.4. Morphology
Comparison of three groups (less than 30 min, between 3 min and 2 hours, more than 2 hours) showed morphology was not influenced by cellphone (P = 0.305) and internet (P = 0.909) usage duration (23). In infertility men, a significant decrease (P = 0.001) was seen regarding pathological morphology sperm between the cellphone user (68%) and non-user (58%) (19). There were not any significant differences in terms of abnormal forms between those who keep cellphone in their pocket or their belt holder in infertile men (18). A statistically significant difference was observed between the control group and both group A (the group with less than 1 h/day use of mobile phone) and group B (group with more than 2h/day usage of mobile phone), but this difference was non-significant between the control group and the group C with 1 – 2 h/day of cellphone use. Increasing daily use of cellphone, sperm count significantly decreases, which causes infertile in men. Men keeping cellphones in the trouser pocket showed a significant decrease in morphology in comparison with those who keeping mobile phones in the waist pocket and shirt pocket (16). The duration of daily exposure to cellphone was not related to morphology (16). There was not any encounter patterns –sustainable response between mobile use and normal sperm morphology (24). Significant increase observed in abnormal morphology in cordless phone users (22). increasing the frequency of cellphone use is associated with a decrease in the percentage of normal morphology and an increase in the percentage of mild, moderate, and severe sperm (P < 0.001) (1).
4.5. Sperm Fertility
Sperm fertility was influenced by the operating frequency of 900 MHz, and operating frequency of 1800 MHz were placed near testis (6).
4.6. Progressive Motile Sperm
In the first study, the length of possession (r = -0.12) and daily transmission (r = -0.19) showed a negative correlation with the proportion of rapid progressive motile sperm. The length of possession (r = 0.12) and daily transmission (r = 0.28) showed a positive correlation with the proportion of slow progressive motile sperm (7). In the second study comparison of three groups (less than 30 min, between 3 min and 2 hours, more than 2 hours) showed total motile sperm number was influenced by cellphone (P = 0.05) and internet using duration (P = 0.032) (23). In the fourth study, no correlation was found between the mobile phone of usage duration and progressive motility (r = -0.22) (20). In infertility men, a significant decrease (P = 0.01) was seen regarding rapid progressive motile sperm between the cellphone user (25.19%) and non-user (23.9%) (19). There were not any significant differences in terms of progressive motility between who keep cellphone in their pocket or their belt holder in infertile men, but there were a significant differences terms of progressive motility amid the mobile phone user groups and the control group (< 1 h, 1 – 2 h, > 2 h) (18). In infertile men, the sperm number was significantly decreased as the daily cellphone users increased (5). The absence of any facing pattern - sustainable response between mobile use and semen volume, the overall mobility of men carrying their mobile in their pockets, the total number of motile sperm increased significantly (24). Significant increase in immotile sperm in the group using mobile near their lumbar spine (78.94%) compared to who put it in their hand (5.26%) or using hands-free (10.52%). Mobile has been associated with a significant decrease in motility sperms ratio and progressive motile sperm (group A: 35.7%, group B: 32.8%, group C: 26.9%, group D: 25.4%) (21). Significant increase in immobilized sperm in who put the phone in their trouser pocket compared to those who put it in waist pocket (P = 0.045) (22). Increased frequency of cellphone use was associated with a decrease in the percentage of normal sperm motility and an increase in sperm grade 3 motility (P < 0.001).
4.7. Sperm Vitality and Membrane Integrity
The sperm vitality and the membrane integrity of men exposed to the electromagnetic radiation decreased about 20 and 12%, respectively (17). No correlation was found between the duration of use of mobile phone and the low mitochondrial membrane potential (r = 0.42) (20).
5. Discussion
The search was updated from 28 October 2018 to 5 July 2019 by using database query terms. Fourteen updated articles were found which evaluated the impact of mobile phone use on the fertility and quality of semen amid men. Overall, there has been a significant decrease in semen analysis parameters worldwide over the last decade. Researchers agree that sperm quality is influenced by certain environmental factors which have a negative effect on it. Environmental factors which have harmful effects are well known. Those are tobacco use, alcohol abuse, and spermicidal food intake. In addition, increase of the negative effect of local testicular temperature on spermatogenesis has been well proved (16, 26, 27). Reproductive toxins such as lead and cadmium should be considered as sperm quality reducing factors, which are relevant to impairment of sperm motility, percentage of viability potential, and most importantly sperm DNA fragmentation, and increase in the levels of reactive oxygen species in semen. While no conclusions can be made from the current evidence, most studies have shown that male fertility declines with mobile use (28). However, the relationship between cellphone use and male infertility has not been clearly determined yet. Possible causes are divided into two general categories: 1. thermal effects 2. Non-thermal effects. Physiologically, testicular temperature needs to be 2 degrees lower than environmental temperature for optimal testicular function. Increasing the temperature by electromagnetic waves can be harmful to spermatogenesis (16). Non-thermal effects of mobile electromagnetic radiofrequency radiation can be increase oxidative stress reactions and dysfunction or testicular structure. In vitro studies have shown that cellphone waves can increase ROS levels in spermatozoa (11). In addition, studies have shown that cellphone waves cause potential changes in sperm cell membranes, transductal signals and apoptosis, as well as DNA damage. It also changes the level of sex hormones (29). Although, comparing the diagnostic parameters collected by using most of the studies showed that the use of mobile phones decreased the sperm motility. In this study, heterogeneity between studies was observed. This heterogeneity may be affected by clinical source factors such as race, age, occupation, place of living, health status, different authors, locations of studies, different measurement environments and instruments, accuracy and calibration of the device, skill, etc. Findings from these studies indicate that prolonged use of cellphones may decrease sperm count, impair motility, or cause apparent structure impairment. Male fertility disorder may appear as a decrease in sperm count, mobility disorder, or structural disorder. Confounding factors such as age, duration of abstinence from sex, drug and alcohol use, body mass index, adequate cola intake have contributory roles in semen fluid change. Lifestyle and age are strong factors associated with semen quality. Therefore, to evaluate the effect of other factors on semen quality, these factors should be adjusted (17). Fejes et al. examined 371 men who were in infertility assessments for daily cellphone use and reported that daily cellphone talk had a negative association with the moving spermatozoid (7). Davoudi et al. showed that using GSM phones for six hours a day and 5 days a week reduces the moving spermatozoid with rapid progressive movement (9). In addition, Agrawal et al.'s study showed that cellphone use not only reduces sperm motility but also significantly reduced its viability and morphology (5). They reported that these three parameters of sperm declined in all cellphone groups with increasing exposure of daily use (20). On the effects of electromagnetic waves on the quality of sperm parameters based on cellphone location, Kilgallon and Simmons's study of 52 men in the age range of 18 to 35 years found that men who placed their cellphone in a pelvic pocket or in their belt had a lower sperm concentration than those who did not carry the cellphone or place it elsewhere (30). Zhang et al. showed that lifestyle and age are strong factors related to semen quality. Therefore, to evaluate the effect of other factors on semen quality, these factors should be adjusted. In this study, after adjusting for confounding factors, studies showed that specific aspects of cellphone use may have negative effects on sperm amount, volume of semen, and sperm concentration. These outcomes suggest that exposure to cellular electromagnetic radiation may have specific effects on testicular function or structure and may cause spermatogenesis disorders (16). In a retrospective study, Gutschi et al. examined the effect of mobile phones on semen parameters. All parameters that were evaluated had a negative relationship with cellphone use. There was a significant difference in sperm morphology between the two groups. Abnormal morphology of spermatozoa was observed in 68% of the mobile phone group compared to 58.18% of the non-mobile phone use group (19). Teratozospermia was detected in 45.3% of mobile phone users compared to 27.7% of the non-mobile phone users group. The ratio of mobile spermatozoa with rapid progressive movement was significantly reduced in the mobile phone user group (23.98%) compared to 25.19% in the non-mobile phone user group. No significant difference was found in the amount of sperm between the two groups. Regarding to the hormonal profile, the group using the mobile phone had significantly higher testosterone levels and a less LH level than non-usage of mobile phone. No significant difference was found in prolactin and FSH levels between the two groups (20). Mostafa et al. examined the impact of exposure to radiofrequency electromagnetic waves on the quality of human semen and its DNA damage. The results of this study showed that there was a significant difference between radiofrequency electromagnetic waves, production of reactive oxygen species, and mean level of melanodialdehyde MDA in the group that exposed to the radiofrequency, which is significantly higher than the other groups (21). Some studies show the effects of a computer connected to the internet via Wi Fi on human spermatozoa. When the subjects worked with the laptop for four hours, a significant decrease in the progressive motility of spermatozoa and a significant increase in the ratio of sperms to fragmented DNA were observed. The researchers hypothesized that the use of a wireless internet connected to a laptop near the male genital area would decrease sperm quality. DNA degradation can lead to changes in the morphological parameters of spermatozoa (31, 32). Al-Bayyari examined the impact of mobile phone use on the fertility and quality of semen amongst 159 Jordanian men. Regarding the quality of sperm parameters, no statistically significant difference was found between the contestant groups. However, there were no statistically significant difference in sperm count less than 20,000,000, Normal viscosity (71.8% vs 28.2%), complete fluidization within 20 minutes (66.9%), mean percentage of immobilized sperm (52.46 ± 2.58 vs 59.78 ± 3.48), and volume less than 3 ml (62.7% vs 37.3%). There was a mean statistical difference between percentage of sperm and abnormal morphology (63.07 ± 2.95 vs 70.32 ± 4.01) (22). According to the results of Falzone et al. there was a significant decrease between exposed spermatozoa in comparison to unexposed spermatozoa in the head area of sperm and the acrosome's head area's percentage reported. The author concluded that although exposure to radiofrequency electromagnetic fields did not have a detrimental effect on the reaction of the acrosome, it could have an important impact on morphology of sperm. Moreover, there was a significant decrease in sperm binding to Hemizona. These outcomes may show the impact of radiofrequency electromagnetic waves on the potential of male fertility (33). Common metal objects, such as coins, rings or zippers in the pockets of pants, may exacerbate the effects of radio frequency electromagnetic waves. An actual cellphone source located in front pants showed that the human body can uptake a specific SAR. Real metal objects (such as coins, rings and rips) were added daily to the sample's study. The researchers conclude these items increase the level of SAR in the body at altered frequencies. The impact of the accumulation of these three items normally increased the level of SAR in the waist area more than the upper area, and the portion of the frequency range is more than allowed in the UK (24). Another interesting finding of the study is that women who wish to have children should take care of their laptops and cellphones. Human sperm has eighty hours or more fertility life in the female genital tract fallopian tube, and the survival of spermatozoa in the cervix may be compromised by electromagnetic waves (21, 22). Men who are preparing for fatherhood or women who wish to have children, especially when there are problems with fertility, should be aware of the different environmental hazards and possibly the direct impact of long-range cellphone waves on the quality of semen and embryo or embryo evolution. The study of Yidimir et al. compared the sperm parameters in four groups of 145 patients who completed the questionnaire. The authors finalized that the periods of cellphone use have no significant difference with sperm amount and motility. Similarly, they found no significant difference between different modes of cellular transport and sperm count and motility. However, according to the data of this study, as the use of wireless internet increased, the sperm motility was reduced. Also, the mobility of spermatozoa in the wireless internet usage group was worse than the non-wireless internet usage group (34). In 2013, Rago et al. examined the quality of semen in mobile consumers. There was no significant difference between the groups in terms of semen volume, sperm density, total sperm count, morphology, and motility of sperm with progressive movement. Also, there was no difference in ultra-sonographic criteria (testicular/prostate volume, cranial diameter, posterior diameter of seminal vesicle) among the study groups. The percentage of spermatozoa with shredded DNA was significantly higher in those who kept their cellphones in their pockets compared to those who kept it in their shirt pockets (20).
To clarify this issue, human studies provide better evidence than animal and laboratory studies; however, they are limited due to organizational and functional problems. Integrated variables or parameters in using the cellphone and standardized empirical methods are essential requirements in human studies. Some studies only considered the duration of talking with a cellphone, while some studies defined broader consumption patterns such as talking, using the internet, and playing with a cellphone. Similarly, changes in the duration, frequency, and pattern of exposure to cellular radio frequency electromagnetic waves may explicate the difference among the outcomes of laboratory studies, animal studies, and human studies. Studies of the effects of electromagnetic waves on the human body have ethical issues (17). The results of current studies need to be followed over a longer period of time and applied to a larger group of men. Such research requires long-term design and healthy volunteers. Obviously, the long-term effects of direct cellphone waves on sperm can progressively damage sperm motility parameters and DNA fragmentation. Accordingly, direct contact with the cellphone waves may damage the sperm and directly affect motility. This probably affects the fertility of healthy men, and it will probably put them at the risk of infertility in the future. Also, despite the positive results mentioned above, and as mentioned in Table 1 empirical and epidemiological evidence of the harmful effects of cellphone on sperm quality is still ambiguous. The contradictory results of cellular radiation studies on sperm motility, viability, and morphology are observed. There are several factors that can influence human outcomes and may lead to discrepancies among studies. Firstly, these men's analysis criterion, which has been mentioned by various studies, is different due to constant changes in the relevant action instructions. Secondly, there is considerable variation in methodology and practice between different laboratories regarding semen analysis. In addition, the frequency and duration of cellphone use is varying. The effect of mobile phone brand has been overlooked in some studies, which may vary their specific uptake. The age of the population under study in most studies was in the same age range, and these optimistic outcomes should be examined in altered age groups of other populations. Other limitations of some studies include low sample size, lack of blood glucose measurement, hormone tests to detect thyroid disorders, adrenal function, which may alter sperm parameters. Overall, the results showed that RF has detrimental effects on semen parameters. Based on other systematic review studies RF exposure is a risk factor for sperm motility and viability and exposure to mobile phones was associated with reduced sperm motility and viability, but it has no effect on sperm concentration (35, 36). Due to an increase of RF waves used currently by people and its role in male infertility, giving information to men about adverse complications of RF is necessary, and the following is recommended to reduce the adverse effects of electromagnetic radiation emitted from mobile phones: 1. Long-term exposure of mobile radiofrequency electromagnetic waves to sperm results in an increase in non progressive motility sperm and a significant decline in the total of progressive motility sperms 2. Sperm DNA fragmentation occurs because of long-term direct access to cellphones 3. Those who have fertility issues and are preparing themselves for parenthood should not carry their cellphone in their pants for a long time.