1. Context
The liver plays a principal role in detoxification and clearance of drugs, and any liver diseases can lead to impairment in drug metabolism; thus, the more progressive the liver disease, the further impairment in drug metabolism (1). This occurs because hepatic blood flow decreases, portosystemic shunting takes place, and the number and function of existing hepatocytes decrease. Liver diseases are divided into acute and chronic types, among which viral infections, the use of alcohol and drug toxicity are the commonest causes (2). Decompensated liver disease and the occurrence of clinical features as ascites, edema, hepatic encephalopathy, and hepatorenal syndrome will affect the pharmacokinetics of most drugs (1). Glomerular filtration rate and creatinine clearance correlate with renal clearance in patients with renal diseases; however, there is no precise measurement for the severity of the liver diseases, which can be used as a guide for dose adjustment (3). Pain management is essential for all patients, including those with liver diseases who are more susceptible to adverse effects due to the hepatic metabolism of these drugs (4). Opiates should be carefully used in patients with liver diseases since they are well-known for constipation, sedation, and hastening of encephalopathy. Opiates are predominantly metabolized via CYP450 (CYP2D6 AND CYP3A4) and glucuronidation, both of which change in liver diseases (5). The leading concern with non-steroidal anti-inflammatory drugs (NSAIDs) in liver diseases is the danger of precipitating and renal impairment via contraction of afferent glomerular arterioles and, consequently, declined renal perfusion. Pre-existing renal dysfunction is fairly usual in patients with liver diseases due to reduced glomerular filtration rate, decreased sodium and water excretion, and efficient renal plasma flow, making these patients principally more susceptible (6). Moreover, NSAIDs exacerbate gastrointestinal bleeding and renal impairment and decrease the efficacy of diuretics in patients with cirrhosis. Acetaminophen (also known as paracetamol, N-acetyl-p-aminophenol, or APAP) is a slight analgesic and antipyretic drug accessible in various preparations (7). Acetaminophen is considered first-line therapy for pain management in patients suffering from liver diseases because of the side effects of other analgesics, including NSAIDs and opioids (8). As acetaminophen is metabolized by the liver and the liver is the key place of injury after the overdose, there is an assumption that patients with chronic liver disease may be in danger when consuming the drug at therapeutic doses. Theoretically, hepatotoxicity can proceed in subjects with chronic liver diseases in conditions that high blood levels of acetaminophen are reached owing to delayed metabolism or if there is augmented production of the toxic metabolite due to increased activity of the cytochrome P-450 enzyme system or as a consequence of decreased glutathione stores (9). This review will provide an overview of acetaminophen use as an analgesic agent in patients with liver diseases.
2. Methods
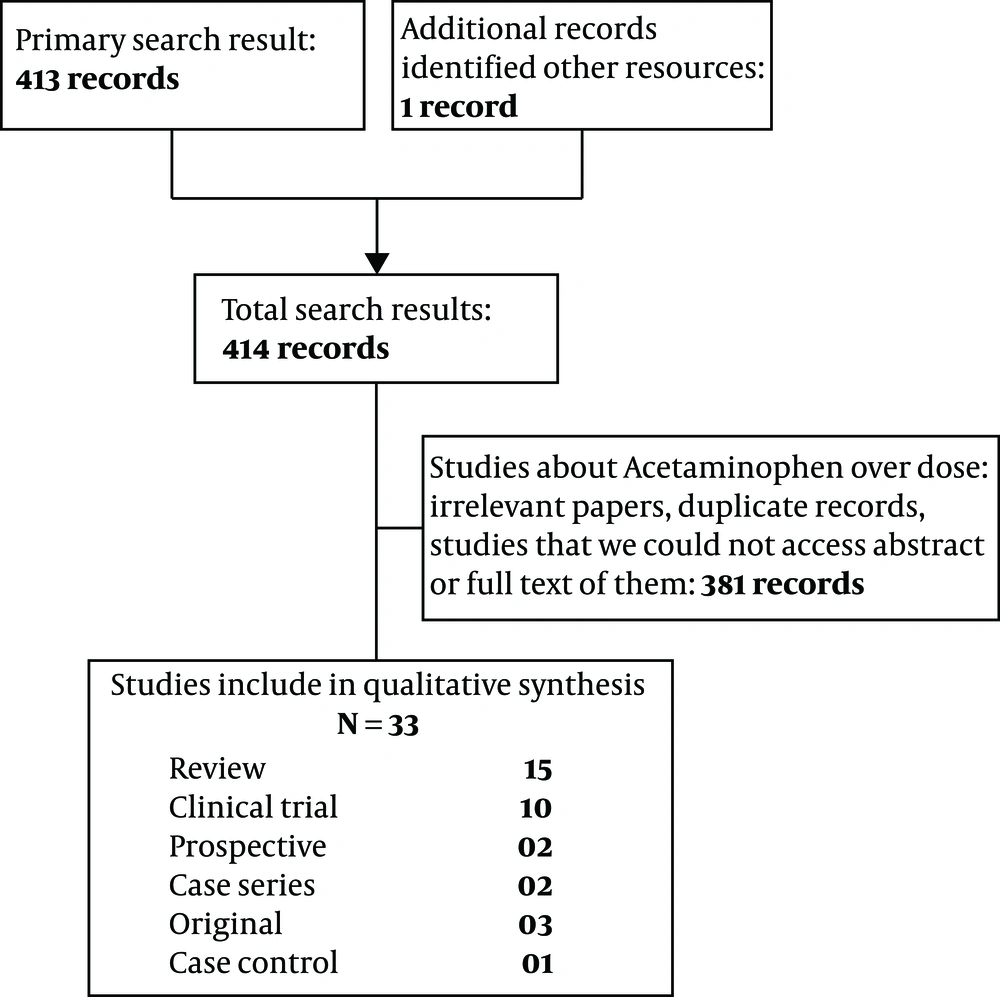
Data were gathered from investigating 33 papers. All articles were published until July 2020. The search was done using the following keywords: acetaminophen, paracetamol, cirrhosis, liver disease, chronic hepatitis, and safety in reliable databases, including PubMed, Embase, Ovid, and Scopus. A total of 414 articles were found, some of which were excluded owing to irrelevance, studies on animals, and the lack of access o the full text. Finally, 15 review articles, 10 clinical trials, one case-control and two prospective studies, two case series, and three original articles were used for the present study (Figure 1).
3. Results
3.1. Cirrhosis
Cirrhosis is one of the most common problems of public health, causing lots of deaths, according to the autopsies. Alcohol use, viral and autoimmune hepatitis, and fatty liver diseases cause cirrhosis (10). The perception that acetaminophen is toxic in cirrhotic patients arises from the hepatotoxicity ensued due to acetaminophen overdose, although glutathione supply is sufficient in these patients and cytochrome P-450 activity is not increased (which would cause decreased NAPQ1) while taking a therapeutic dose of acetaminophen. This suggests the safe use of acetaminophen in patients with cirrhosis (11). Patients with chronic liver diseases can safely receive 4 g/day of acetaminophen as its glucuronidation and sulfation to nontoxic metabolites are not affected unless there is a risk factor for glutathione deficiency. An increase in the half-life of acetaminophen in patients with cirrhosis is not associated with hepatotoxicity or hepatic decompensation (8). In patients with cirrhosis, the half-life of oral acetaminophen is doubled, but it rarely causes renal or hepatic injury while taking in doses lower than 4 g/d (12). Glutation supply is variable in individuals encompassing patients with liver diseases. Malnutrition and alcohol consumption are the causes of glutathione depletion. Cirrhosis does not affect the level of glutathione. In patients with cirrhosis (not actively drinking alcohol), acetaminophen can safely be prescribed even for periods more than 14 days at doses of 2 to 3 g/day, and 3 to 4 g as a short-term or one-time dose (13). The metabolism of analgesics in patients with chronic liver diseases without cirrhosis is similar to the normal population. Some studies concluded that therapeutic doses of acetaminophen can be safely administered in patients with cirrhosis (11). A literature review about the therapeutic use of analgesics in patients with cirrhosis concluded that 2 to 3 g/d of acetaminophen was safe even for long periods. It concluded that as acetaminophen lacked sedative effect and nephrotoxicity and was safe in liver diseases encompassing cirrhosis, it could be the first choice for pain management in this group (9). A double-blind, two-period crossover study showed that 4g/d of acetaminophen for 13 days was safe for patients with chronic stable liver diseases, including cirrhosis (14). A study about the pharmacokinetics of acetaminophen in patients with cirrhosis, which studied 11 patients with pathologically confirmed cirrhosis and 12 controls, showed that plasma concentration of acetaminophen in patients with cirrhosis was higher than healthy individuals (P < 0.05) in 30, 60, 120, 180, 240, 300, and 360 minutes after drug administration. Biological half-life of acetaminophen in cirrhotic patients was 1.6 hours longer than healthy individuals (3.7 h. compared to 2.1 h.) when 1 g acetaminophen was orally taken. Average plasma clearance was decreased to less than half of the control group but did not have a toxic effect on the liver regardless of its effect on prothrombin time, galactose elimination capacity, plasma albumin and plasma clearance of phenazone. Moreover, when 1 g acetaminophen was administered subchronically (5 days), its half-life did not differ in patients with (4 cases) and without (9 cases) liver cirrhosis according to paired t-test. Any individual’s plasma concentration in days 2 and 5 did not vary (15). Zapater et al. (16) administered 1 g of acetaminophen to patients with cirrhosis and plasma levels of acetaminophen and its glucuronide, sulfate, cysteine and mercapturate conjugates were repeatedly measured (11 times after administering acetaminophen and once just before receiving acetaminophen) in blood samples and 24 h urine and were compared with healthy individuals. Reduced acetaminophen clearance in cirrhotic patients, which culminated in increased mean area under the curve concentration (AUC), were found in comparison to patients without underlying liver diseases. The mean systolic blood pressure in cirrhotic patients had a notable direct relationship with AUC 0 - 6 of acetaminophen regardless of the severity of underlying liver diseases. In patients with esophageal varices, the plasma concentration of acetaminophen raised faster to therapeutic levels (16). In another study in which six patients with chronic liver diseases received 4 g/d of acetaminophen for more than five days, no toxic effect was found (12). As mild to moderate hepatic failure does not affect the pharmacokinetics of acetaminophen, it can be safely administered in such patients (17). Riley and Smith (18) mentioned that acetaminophen at a dose of 2 g/d can be administered in cirrhosis patients. A case-control study on 170 patients concluded that acetaminophen in adjusted doses of 2 - 3 g/d did not correlate with hepatic decompensation (19). Even in alcoholic cirrhosis, 3 g/d of acetaminophen can be safely used (20). Acetaminophen is not considered toxic at a dose of 2 g/d in cirrhotic patients as mentioned in a review article about medication prescription in patients who suffer from decompensated liver cirrhosis (21). Glutathione shortage does not seem a problem in patients with severe liver diseases and therapeutic dose of acetaminophen does not aggravate treatment-emergent adverse effect, so patients with liver diseases can safely receive acetaminophen in therapeutic doses (11, 22).
3.2. Alcoholic Liver Disease
A systematic review concluded that alcoholic patients can safely receive acetaminophen in therapeutic doses (23). A randomized double-blinded placebo-controlled study aimed to assess if a maximal therapeutic dose of acetaminophen was associated with hepatic injury in patients with chronic alcohol abuse immediately following the cessation of alcohol intake. They received 4 g of acetaminophen (1,000 mg QID) or a placebo for two days. The results showed that the levels of aminotransferases and international normalized ratio (INR) did not differ significantly among these two groups (using 2-way analysis of variance) in 2 days following acetaminophen ingestion, thereby suggesting no increase in liver toxicity of therapeutic doses of acetaminophen in alcoholic patients (24). Based on two Randomized Controlled trials (RCTs) and other studies, patients with stable chronic alcoholic disease can receive acetaminophen up to 4 g for 48 to 72 hours (25). Liver toxicity was reported in 76 patients who had received acetaminophen in nontoxic doses (< 6 g/d), all of whom regularly used alcohol. More than half of the patients took alcohol more than 80 g in a day. More than half of the patients with developed liver injury due to acetaminophen had taken more than 4 g every day, which was the recommended dose (26). Hepatotoxicity (significant increase in the levels of aminotransferases and following acute liver failure) in patients receiving acetaminophen in the range of 2.6 to 10 g or higher was reported in 13 alcoholic patients (27). Fifty-three alcoholic patients suffered from acetaminophen-induced hepatotoxicity (average dose and duration of acetaminophen use were 6.62 g and 4.6 days, respectively) (28). A randomized controlled trial showed that acetaminophen at a dose of 4 g for 10 days in patients consuming 1 to 3 drinks of alcohol per day did not have any toxic effect other than a non-significant rise in the liver enzymes (8 IU/mL). Even patients with cirrhosis who regularly drink alcohol can take acetaminophen 4 g/d for a short period or single-dose (29). Acetaminophen causes little elevation of serum alanine aminotransferase (ALT) when used for 10 days in therapeutic doses in some of the individuals who moderately drink alcohol (30). In patients who are not heavy drinkers, acetaminophen is safe up to 4 g per day for short-term (13). Acetaminophen half-life was 50% higher in patients with cirrhosis compared to in healthy individuals. There was not a significant difference between those who had ascites and those who had not. Similarly, the presence of a portacaval shunt did not alter acetaminophen’s half-life in patients with cirrhosis (31).
According to a systematic review about the administration of acetaminophen in alcohol consumers, no adverse effect of acetaminophen was found at therapeutic doses for 48 hours in class 1 studies, and for 14 days in class 2 studies, and a single dose of acetaminophen at a dose of 1 - 2 g was safe. However, class 3 studies reported hepatotoxicity of acetaminophen in alcohol drinkers. Additionally, there is no effect on hepatic aminotransferase enzymes, prothrombin time, or other biochemical parameters in well-designed trials (23). A multicenter randomized study in which alcoholic patients took 4 g/d for 3 consecutive days and glutathione, aspartate aminotransferase (AST), ALT, and INR levels were compared with placebo-receiving group until 2 days following acetaminophen ingestion. No statistical difference was found between the case and control groups, suggesting the safe usage of acetaminophen in alcoholic persons (24). A study that surveyed the risk of drug-induced liver injury in patients with pre-existing liver diseases concluded that acetaminophen could increase the risk of liver damage in patients with alcohol-induced liver diseases (32).
3.3. Chronic Hepatitis
There are some pieces of evidence regarding an increased risk of acetaminophen-related hepatotoxicity in patients with chronic hepatitis C infection. Progression to severe hepatic failure after acetaminophen usage was higher in patients with chronic hepatitis infection compared to those without infection (33, 34). A study that assessed healthcare providers’ opinion and their recommendations on NSAIDs and paracetamol usage in patients with cirrhosis and chronic hepatitis showed that their recommendations against the use of acetaminophen were significantly more common than recommendations against the use of paracetamol (35).
3.4. Non-Alcoholic Fatty Liver Disease
Michaut et al. (36) showed that non-alcoholic fatty liver disease (NAFLD) can predispose patients to acetaminophen toxicity. In patients with NAFLD and obesity, some of the drugs such as acetaminophen, methotrexate, haloten, carbon tetrachloride, and ethanol can cause greater toxicity (37). A study that evaluated the danger of drug-induced liver injury in patients with pre-existing liver diseases concluded that acetaminophen consumption was related to improved risk of liver injury in patients with NAFLD (32). In these patients, therapeutic dosages of acetaminophen aggravate fat accumulation and impair hepatic autophagy. As activation of autophagy protects against acetaminophen-induced liver injury, patients with NAFLD are more susceptible to acetaminophen-induced liver injury due to impaired autophagy. Therefore, a lower dose of acetaminophen should be used in these patients (38, 39).
Although the predisposing role of hepatic steatosis to acetaminophen intoxication has been assessed in several animal studies, the exact mechanism is not clear yet. A recent study has assessed the association between NAFLD and acetaminophen toxicity by examining the role of nuclear receptor peroxisome proliferator-activated receptor α (PPARα) and coactivator peroxisome proliferator-activated receptor gamma coactivator 1-β (PGC-1β) in driving inflammation, mitochondria redox balance and fatty acid metabolism. Awareness of this mechanism can be a rational approach to reduce the maximum dose of acetaminophen for patients with liver steatosis (40).
4. Conclusions
Patients with cirrhosis can safely take acetaminophen in adjusted doses. Although acetaminophen has been safely administered in therapeutic doses in alcoholic patients, there are reports of hepatotoxicity even in therapeutic doses. Recommendation against acetaminophen is higher than NSAIDs in patients with chronic hepatitis. Patients with NAFLD are susceptible to acetaminophen toxicity. Generally, it can be recommended to assess liver function and consider the severity of liver diseases before the administration of acetaminophen.