1. Context
Climate change refers to any lasting change in the Earth's climate over a period of time (1, 2). Global warming is a type of climate change in which the average temperature in the lower layers of the Earth's atmosphere is increased due to factors such as greenhouse gas emissions and air pollution (3-6). Estimates indicate that the annual average temperature and frequency of the heat wave are increasing. Climate change and increased global warming, in addition to economic and social impacts, have become a potential threat to human health (1, 7-11). According to a report by the center for research on the epidemiology of disasters (CRED), 44% of the 147 events recorded in the first quarter of 2017 were due to climate change. Environmental and climate changes have direct and indirect effects on health, human well-being, and the mortality pattern of infectious and noncommunicable diseases (NCDs) (12-15).
Climate change has caused an increasing number of people with health problems, such as the elderly, children, and patients, to be at risk (16-19). Climate change has contributed to death due to heat-stroke, non-infectious diseases such as cardiovascular, pulmonary, malnutrition, and contagious diseases (4, 11, 20, 21). However, the slowing down of cold winters, hence fewer cold season illnesses such as respiratory diseases, and the increase in agricultural production are among the positive effects of climate change (22). On the other hand, the increase in air temperature during the recent years has predisposed some patients with non-respiratory diseases such as cardiovascular disease to temperature change complications more than other people in the community (23, 24). Various studies have reported a correlation between air temperature changes (decrease or increase) and compromising heart health (11, 14, 17, 19, 21, 25-27).
For example, in patients with heart failure, the increase in temperature increases the incidence of disabling complications (25, 28). To achieve full health in these individuals, at least some basic needs must be provided; needs that are undergoing changes as a result of climate change. Among these changes is a reduction in healthy and adequate food and water resources in societies. On the other hand, following the increase in sweating in the rising temperature, the chance of drug poisoning increases and can be a factor of referral and re-admitting individuals to treatment centers (23, 29, 30). The World Health Organization (WHO) has declared climate change and NCDs, including cardiovascular disease, in 2019 as two main health threats (11, 17). Despite all the scientific advances in the prevention and treatment of diseases, cardiovascular disease is still considered the first cause of death worldwide (31-33). Prevention of these diseases, as well as the reduction of complications, disability, and death in various age and sex groups, are among the most important goals of the health system in the world (34). Considering the widespread occurrence of cardiovascular diseases, conducting a comprehensive study on the factors affecting the patients and those who are predisposed to these diseases is an important issue in reducing their tangible and intangible complications. Therefore, this study aimed to identify the role of climate change factors on cardiovascular diseases.
2. Evidence Acquisition
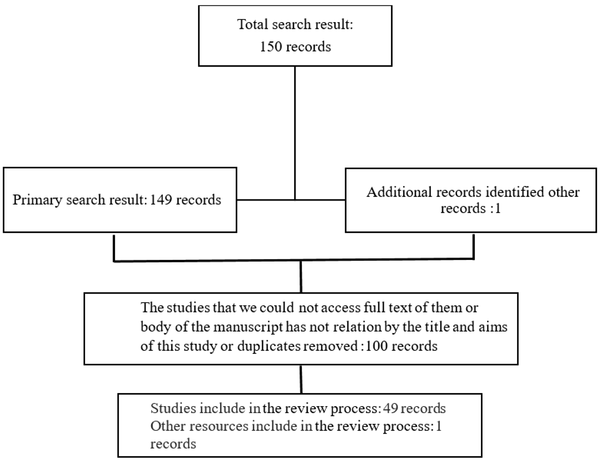
The current narrative review study searched the databases including EMBASE, PubMed, Science Direct, Ovid, Cochrane Library, Magiran, and SID using Persian and English keywords such as ‘climate change’, ‘cold wave’, ‘heat wave’, ‘temperature decrease’, ‘temperature rise’, ‘heart disease’, ‘heart attack’, and ‘heart failure’ from the beginning of 2000 to the end of 2019. A total of 150 articles were retrieved from these databases, and their abstracts were evaluated by the research team. According to the availability of full-text of the articles and their relationship with the subject of the study, 50 papers were finally included in the study (Figure 1).
3. Results
Climate change affects the heart health through air pollution, increase in air temperature, and dietary changes (35). Following the increase in air temperature, the contractility of the heart decreases. On the other hand, temperature increase leads to an increase in the central body temperature, which in turn causes the body's compensating mechanism to increase the heart rate and direct blood flow to the skin through central organs, such as the heart and kidneys. The body increases sweating to adjust its temperature. In a patient with heart disease, the heart's reduced ability to circulate blood to vital organs can contribute to worsening of the symptoms and threatening the life of the individual (16, 34, 36). Studies from around the world have shown that climate change has increased the deaths of people with heart disease (37).
Cardiac attacks, as one of the most common cardiac disorders, account for more than one third of deaths in developing countries (10, 38). Studies have shown that cardiovascular disease is a result of environmental stressors, including air temperature; moreover, there is a relationship between the heart disease morbidity and mortality rates and the highest and lowest temperatures (20, 39-41). According to various studies, the association between the reduction of air temperature and the increase in the incidence and mortality from heart disease in different age groups has been confirmed, and cold weather is known as one of the most important environmental stressors in cardiac patients (39, 42, 43). However, in recent years, consistent with global warming and temperature increase across the world, several studies have been conducted to investigate the effect of this temperature change on the pattern of NCDs, including cardiovascular disease, whose findings have been contradictory (5, 9, 44).
The results of a study on the effect of rising air temperature on the death rate in a wave of heat in Adelaide, Australia, in 2009 showed that, unfortunately, mortality rates and hospitalization of people with chronic illnesses increased following a rise in air temperatures (40). Research conducted in Europe has shown that for every one-degree temperature increase, the mortality rate from cardiovascular diseases in the southern and northern regions increases by 3.12 and 1.84%, respectively (16). The results of a study conducted in Michigan showed that as a result of an increase in the air temperature, the rate of heart attack increases with changes in the ST segment in the electrocardiogram (1). In a study conducted in Beijing between 2000 and 2011, the results showed that with the increase in air temperature, mortality from heart diseases increased and needed to be addressed by health policy-makers (39). In another study in the Catalonia region of Spain during 2006 - 2013, it was found that the hospitalization rate of patients due to cardiovascular diseases increases as a result of a decrease in the air temperature (20). According to the results of a research in Japan, lower air temperatures contribute to a rise in the mortality rate from heart diseases (3, 45). In line with the Japanese findings, a study in England showed that death from heart diseases in people over 60 years old increased due to lower air temperatures (42, 43).
In recent studies in Iran, contradictory results have been reported. In some studies, findings have shown that deaths from cardiovascular diseases, pulmonary diseases and traumas have increased as a result of higher air temperatures (4, 7, 29, 35, 36, 46, 47). In a study conducted in Mashhad between 2004 and 2013, there was a direct correlation between the increase in air temperature and death from cardiovascular diseases. The study predicted that a rise in temperature in that city during the next decade would result in a 4.27% increase in deaths from cardiovascular diseases (4). However, in another study conducted in Shiraz from 2006 to 2012, there was no significant relationship between temperature changes and death from heart diseases (26).
The findings of most studies in Iran have shown that increased mortality from cardiovascular diseases is associated with lower air temperatures. The results of a study conducted in Kerman over a four-year period showed that there is a negative relationship between air temperature changes and death from heart diseases, i.e. an increase in death due to heart disease followed by a decrease in air temperature (35). The results of the study conducted by Farajzadeh and Darand during 2000 - 2005 in Tehran showed that with decreasing air temperature, the death rate due to heart diseases increased (31). Furthermore, the results of a study carried out by Fallah Ghalhari and Mayvaneh in Mashhad on the effect of air temperature on deaths from pulmonary diseases in a period of 10 years from 2004 to 2013 showed a negative and an inverse relationship (29). Several studies have been conducted over recent years on the effect of air temperature as an important environmental stressor on the pattern and burden of cardiovascular diseases (48-50). Finally, the results obtained in these studies vary in different parts of the world.
4. Conclusions
Considering the increasing climate change and global warming, recognizing climate change and its effects on human health is an important issue for the stake-holders. Heart diseases have a range of symptoms and disorders that affect different age, sex, and occupation groups. With regard to the impact of climate change and the increase in air temperature on the health of people, especially those with heart disease, various studies with contradictory results have been conducted worldwide. The results of some of these studies have shown a positive and direct effect of increasing air temperature on cardiovascular health complications, while some studies have considered this effect insignificant. Considering the world's most up-to-date policies for controlling the effects of greenhouse gas emissions, global warming, and climate change, it is necessary to pay more attention to the health of the population, especially cardiovascular health. Also, it is essential that further research be conducted on the effects of temperature changes on the health of the heart and, based on the results, mega planning and designing related guidelines be carried out by health policy-makers to prevent and reduce the complications of heart disease in at-risk groups.