1. Background
The coronavirus disease 2019 (COVID-19), which begun on December 19 in Wuhan, China spread rapidly around the world (1, 2). The widespread transmission of this disease in the world caused the World Health Organization (WHO) to introduce it as a pandemic and an emergency situation for countries (3, 4). The pandemic not only created fear of disease and death among different people in the society, but also brought double and unbearable psychological pressure to people worldwide. The widespread prevalence of the disease, launching quarantine programs, and delay in reopening of schools and universities negatively affected the mental health of students (5, 6). Since the COVID-19 pandemic has led to fear in different social groups, timely understanding of the mental state of the people is essential (7, 8). Previous studies have shown that the prevalence of COVID-19 has had devastating psychological effects on individuals due to fear of getting sick, fear of dying, and loneliness (9). According to the evidence, similar pandemics have negatively affected the community mental health. Meanwhile, medical students and clinicians, who are directly involved in caring for patients with COVID-19, are at high risk for developing mental disorders (10, 11). Due to the large number of patients with COVID-19 around the world, many countries have asked interns, and even professors and residents, to join the workforce and treat the patients. However, the lack of sufficient experience and knowledge in medical students in such critical situations can be very stressful (12, 13). A study in China found that 27% of medical students who lacked sufficient experience in dealing with such crises and entered the medical environment as workforce experienced psychological distress, and 11% suffered from mental disorders such as post-traumatic stress disorder (PTSD) (14). So far, several studies have been conducted on the effect of COVID-19 on the mental health of medical staff, children, adults, and the general population (14-16), but few studies have been conducted on medical students and professors, especially in Iran.
2. Objectives
Hence, this study aimed to investigate the extent of psychological distress and coping strategies among clinicians and medical students during the COVID-19 pandemic in Rasht, Iran.
3. Methods
3.1. Participants and Study Plan
Using the Kessler psychological distress scale (K10), this cross-sectional analytical study evaluated psychological distress and coping strategies among 109 clinicians and medical students working in Razi Hospital of Rasht, Iran during the COVID-19 pandemic from May to June, 2020.
The statistical population of this study included all clinicians working in COVID-19 departments of Razi Hospital. The selected samples were interns (n = 34), residents (n = 42: internal residents = 32, surgery residents = 5, urology residents = 5), and professors (n = 33: internal professor = 5, emergency medicine professor = 3, surgery professor = 5, urology professor = 7, oncologist = 5, infection disease specialist = 5, rheumatologist = 3). All participants answered the distributed data collection tools (response rate = 100%).
Guilan was one of the first major provinces involved in the COVID-19 crisis in Iran and Razi Hospital in Rasht was the main referral center for COVID-19 patients, which had the highest number of admitted patients. In Rasht, there were only three hospitals admitting COVID-19 patients, including Razi Hospital, Ghaem Private Hospital, and Rasoul-Akram Hospital. Two of these hospitals were non-educational and did not have professors, interns, or residents. Hence, we only included samples working in Razi Hospital.
Inclusion criteria were professors, residents, and interns who had active participation in the visit and management of COVID-19 patients.
3.2. Sampling
Participants were selected by convenience sampling. To decrease the risk of infection during the pandemic, we distributed the checklists and questionnaires by email and obtained an informed consent from all participants. The samples were also assured that their information would be kept strictly confidential.
In order to evaluate the degree of psychological distress and coping strategies among clinicians and medical students, three scales were used including: a demographic information questionnaire, the K10 scale, and a self-made checklist based on a review of texts to evaluate the coping strategies in pandemic situations. Demographic variables including age, sex, marital status, residential status, and level of education were also recorded.
3.3. Ethical Considerations
This research was approved by the Ethics Committee of Guilan University of Medical Sciences, Iran (code: IR.GUMS.REC.1399.134). The objectives of the research were explained to all participants and they were assured of the confidentiality of the information. Also, written informed consent was received from all participants before completing the questionnaires and checklist.
3.4. Questionnaires
3.4.1. Demographic Characteristics
Demographic variables in this study included age (year), gender (male, female), marital status (single, family), residential status (yes, no), and educational status (faculty member, residents, intern).
3.4.2. The 10-Item Kessler Psychological Distress Scale
The 10-Item Kessler Psychological Distress scale (K10) was developed by Kessler in 1992 to measure mental distress in the general population. The scale includes 10 items with a 5-point Likert scale ranging from 0 (never) to 5 (always). The range of scores obtained is 0-50, and higher scores indicate more psychological distress (17). The Persian version of this scale showed acceptable validity and reliability in Iranian society (18). In this study, Cronbach’s alpha coefficient of K10 scale was equal to 0.771.
3.4.3. The Researcher-Made Checklist of Coping Strategies
In order to examine the coping strategies, we designed a researcher-made checklist, which included 10 items (options such as talking to someone at home, calling and talking online, watching movies, in networks I used social media, I search the web, I exercise, non-academic study, I listen to music…). In order to measure validity of the checklist, we used face validity and content validity. In this regrades, an expert panel (10 medical faculty members) were formed and we calculated CVR and CVI (CVI = 0.79; CVR = 0.82). To measure reliability, we used test-retest method and distributed the checklist to 10 clinicians and medical students with one week interval and calculated the correlation (r = 0.9).
3.5. Statistical Analysis
In this study, continuous variables were expressed as mean (SD) and categorical variables as frequency (percentage). The relationship between demographic variables and total K10 score was assessed using independent t-test, one-way analysis of variance and Pearson’s correlation coefficient. Data were analyzed by SPSS software version 16 and the significance level was considered as 0.05.
4. Results
4.1. Characteristics of Participants
The demographic characteristics of the responders are presented in Table 1. The mean age of the responders was 36.14 (SD = 10.68) years. Out of 109 responders, 51.4% were male, 48.6% were female, 56.9% were married, 76.1% were native, and 38.5% were in residency training (Table 1).
| Demographic Characteristics, Mean ± SD or No. (%) | Psychological Distress, Mean (95% CI) or ra | P | |
|---|---|---|---|
| Age, y | 36.14 ± 10.68 | -0.397 | < 0.001 |
| Sex | 0.067 | ||
| Male | 56 (51.4) | 11.71 (9.67 - 13.76) | |
| Female | 53 (48.6) | 14.40 (12.32 - 16.47) | |
| Marital status | 0.003 | ||
| Single | 47 (43.1) | 15.47 (13.14 - 17.80) | |
| Married | 62 (56.9) | 11.16 (9.40 - 12.92) | |
| Native | 0.033 | ||
| No | 26 (43.1) | 15.81 (12.27 - 19.34) | |
| Yes | 62 (56.9) | 12.14 (10.59 - 13.70) | |
| Academic status | < 0.001 | ||
| Faculty member | 33 (30.3) | 9.39 (7.38 - 11.41) | |
| Resident | 42 (38.5) | 12.48 (10.09 - 14.87) | |
| Intern | 34 (31.2) | 17.21 (14.60 - 19.82) |
Abbreviations: COVID-19: coronavirus disease 2019; CI, confidence interval; SD, standard deviation.
ar, Pearson correlation coefficient.
4.2. Distribution of K10 Scores
The mean K10 total scores was 12.94 (SD = 7.64). Sixty-seven participants (61.5%) reported a K10 total score of 10 or higher, indicating probable psychological distress.
4.3. Relationship of K10 Scores with Demographic Variables
Table 1 presents the relationship between the psychological distress and demographics variables of participants. Based on the Pearson’s correlation coefficients, a significant negative correlation was obtained between age and K10 total scores (r = -0.397, P < 0.001). The mean of K10 total score in females was higher than males, although this difference was not statistically significant (P = 0.067). Single participants had a higher K10 total score compared with married ones (P = 0.003). Furthermore, interns had a higher K10 total score compared with residents (P = 0.012) and faculty members (P < 0.001). Also, residents had a higher mean score of K10 than faculty members (Table 1).
4.4. Coping Strategies and Relationship of K10 Scores
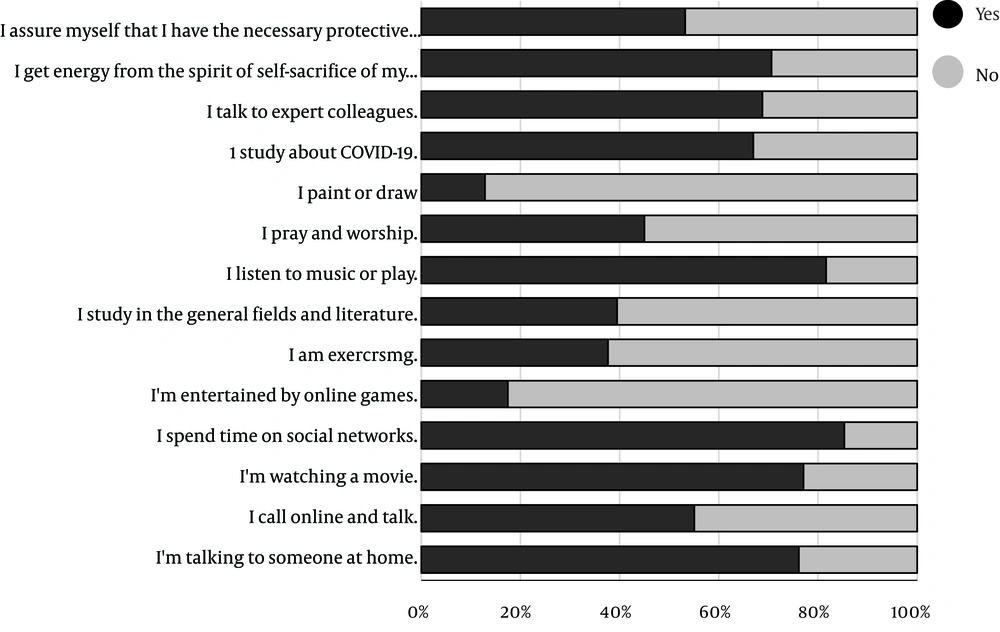
Our results showed that ‘spending time on social networks’ and ‘listening to music’ were among the most common coping strategies used by interns, residents, and faculty members (Figure 1).
There was also a significant relationship between the level of psychological distress of the participants and the use of coping strategies including ‘exercising’ (P = 0.002), ‘talking to expert colleagues’ (P = 0.004), and ‘gaining energy from the spirit of self-sacrifice in their colleagues’ (P < 0.001) (Table 2).
| Coping Strategies | No | Yes | P |
|---|---|---|---|
| I’m talking to someone at home. | 16.35 (8.96) | 11.98 (6.94) | 0.010 |
| I call online and talk. | 13.16 (7.17) | 12.90 (8.09) | 0.859 |
| I’m watching a movie. | 13.72 (7.33) | 12.81 (7.78) | 0.604 |
| I spend time on social networks. | 13.56 (10.06) | 12.92 (7.23) | 0.760 |
| I’m entertained by online games. | 12.91 (7.45) | 13.53 (8.77) | 0.752 |
| I am exercising. | 14.79 (6.76) | 10.07 (8.22) | 0.002 |
| I study in the general fields and literature. | 14.12 (7.23) | 11.33 (8.07) | 0.062 |
| I listen to music or play. | 14.90 (7.37) | 12.60 (7.70) | 0.226 |
| I pray and worship. | 13.93 (7.53) | 11.90 (7.75) | 0.169 |
| I paint or draw. | 12.77 (7.78) | 14.71 (6.75) | 0.377 |
| I read about COVID-19. | 15.53 (7.50) | 11.78 (7.48) | 0.016 |
| I talk to expert colleagues. | 16.09 (7.76) | 11.63 (7.24) | 0.004 |
| I get energy from the spirit of self-sacrifice of my colleagues. | 18.62 (7.67) | 10.69 (6.37) | < 0.001 |
| I assure myself that I have the necessary protective equipment to prevent it. | 14.92 (8.71) | 11.34 (6.20) | 0.014 |
aValues are expressed as mean (SD).
5. Discussion
This is the first study to investigate the level of psychological distress and coping strategies among clinicians and medical students in Guilan Province, Iran. Our results showed that interns are more prone to psychological distress than professors and residents due to their less experience. This might be attributed to not having enough experience in controlling and managing infectious diseases such as COVID-19 pandemic and fear of medical errors in the face of new diseases. Other causes include physical and mental exhaustion due to high workload in the health care system, sudden and rapid changes in medical information, procedures and management of the emerging disease COVID-19, fear of working in high-risk conditions, and lack of equipment. Also, interns should use personal protection equipment, experience long working hours, change their lifestyle due to the pandemic, self-quarantine themselves, and cope with the risk of contracting the virus or transmitting the disease to family members. These findings reveal the importance of providing psychological support to this group in high-risk pandemic conditions, which is consistent with results of another study (11). Some previous studies found that there is a positive relationship between the occurrence of mental disorders and epidemics such as severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) (19, 20). In general, very few studies have been conducted to investigate the effect of the COVID-19 pandemic on the psychological distress of medical students and clinicians; however, previous studies have shown that the prevalence of psychological trauma caused by crises and pandemics in societies is very high (21). In fact, the COVID-19 pandemic has irreversible psychological effects on all individuals and social groups, including the general public, health professionals, and students due to quarantine, fear of disease, anxiety, worrying about attending work and hospitals, and closure of universities. In addition, this might lead to depression following the loss of family members or relatives who are afraid of death (22-24).
In the present study, the mean score of mental distress of female participants was higher than male ones, but no statistically significant relationship was reported. In this regard, a recent research conducted in China found that female medical staff suffer from higher levels of mental disorders, which can be attributed to high workload and child care due to school closures. The study also found that female medical staff suffered from depression and mental disorders due to loneliness and distance from family and children (7, 25). In the present study, it was found that the rate of psychological distress among single students was higher than married people, but there was no significant difference between men and women. Based on the study by Vahedian-Azimi et al. (11), it was found that the rate of mental disorders caused by COVID-19 pandemic is higher among single and male medical students than married and female ones. A review of coping strategies in the COVID-19 pandemic also found that ‘listening to music’ and ‘spending time on social media’ were the most common coping strategies for psychological distress among medical students and professors. It was also found that ‘doing exercise, ‘talking to colleagues’ and ‘being inspired by the spirit of self-sacrifice’ were more common in participants with lower scores of mental distress. Therefore, these coping strategies can be used to prevent or reduce psychological distress among interns, residents, and professors in a pandemic. Unfortunately, since there were no related studies on coping strategies, we could not compare the results.
5.1. Conclusions
Based on the findings of the present study, psychological distress was a common problem among clinicians and medical students during the COVID-19 pandemic in Guilan Province, Iran. According to studies, the existence of psychological distress can prevent proper functioning of clinicians and medical students in the care and treatment of patients with COVID-19. and also according to the available evidence and experiences from past epidemics such as SARS and that some students and medical staff are involved in care. Since COVID-19 interns have long-term mental disorders such as PTSD, it seems that the mental status of interns should be assessed periodically. Moreover, it seems that in order to reduce psychological distress among medical students, especially interns, it is necessary for medical policy makers and government officials to use appropriate approaches to increase their knowledge and readiness to attend hospitals and also to strengthen strategies to monitor the performance of these students.
In addition, we should use appropriate educational course for medical students, specially for interns in front of similar pandemics. There seems to be a need for more attention and support for female students and professors in the COVID-19 pandemic.
5.2. Limitations
The present study had some limitations. First, the sample size was small, which limited our statistical power. Second, since the study was conducted only in one hospital in Guilan Province, the results cannot be generalized to other clinicians and medical students in Iran.