1. Background
Cancer, as the second leading cause of mortality, is increasing around the world (1), especially in developing countries. It is predicated that the prevalence of cancer will increase from around 56% in 2008 to 60% by 2030 in less developed countries (2). In Iran, cancer, as the second largest group of chronic non-communicable diseases (3) and the third cause of mortality, has shown an increasing trend (3-5). Pregnancy and reproductive health are important issues in cancer survivors and patients undergoing cancer treatment; however, limited attention has been paid to these issues and the social and cultural factors.
Cancer treatment can negatively affect women’s reproductive power (5-8). Obviously, women are under major stress during treatment, and the occurrence of pregnancy can increase the severity of stress (7) and disrupt their treatment and recovery processes. These groups of women are more likely to terminate their pregnancy (9, 10), while some of these women, even those with life-threatening conditions, may refuse treatment due to their fear of harm to the fetus (11). It is documented that radiotherapy and chemotherapy during the first trimester of pregnancy can increase the rate of congenital malformations and spontaneous abortion (9, 12), and some methods of cancer treatment can increase the risk of pregnancy loss, preterm birth, low birth weight, and birth of children with special needs (10-12).
Accordingly, it is recommended that women avoid pregnancy during cancer treatment. Also, women with hormone-sensitive cancers are advised to avoid pregnancy three years after treatment, that is, the period of peak recurrence (5, 13). However, it is observed that unintended pregnancy occurs more frequently among women who have chronic medical conditions (14). On the one hand, women under cancer treatment or cancer survivors may assume that they become infertile during or after treatment (15, 16), and on the other hand, physicians, as care providers, only focus on cancer treatment plans and outcomes (17) and may assume that women of this group are not sexually active due to their disease (15).
As a result, identifying factors influencing pregnancy among cancer patients is of great importance. Although there are many studies on unintended pregnancy and contraceptive use, few studies have examined pregnancy, abortion, and contraceptive use among women with cancer (18, 19). All previous researches, reviewed in the present study, found pregnancies during cancer treatment to be unintended. Here, the question arises as to whether all pregnancy is unintended in all groups of women. To the best of our knowledge, there is no study about pregnancy in women undergoing cancer treatment or cancer survivors in Iran. Therefore, the present study aimed to identify influential factors, particularly demographic and sociocultural factors affecting pregnancy in women of reproductive ages in Zahedan City, Iran who were undergoing chemotherapy or radiotherapy, in addition to women who had undergone their last chemotherapy or radiotherapy up to one year ago.
Zahedan is the capital of Sistan and Baluchestan Province which is the second largest province in Iran, which has a border with Afghanistan and Pakistan and has special socioeconomic, cultural, and political circumstances. Among all provinces of Iran, Sistan and Baluchestan has the lowest rank in human development indices (20), and 25% of women, aged 14 - 44 years, are illiterate (21). The last census in Iran demonstrated that this province has the highest rate of total fertility (3.96%) (22), which indicates the lower prevalence of contraceptive use, compared to other regions of Iran. Also, this province is among provinces of Iran with the highest prevalence of unwanted pregnancy (20.7%) (23).
Although the incidence of cancer is lower in Sistan and Baluchestan, the cancer trends are increasing in this region (24).
2. Objectives
Therefore, the findings of the present study can be useful for physicians and family planning service providers to obtain more information about high-risk groups. Our findings may also be considered by health planners to decrease the rate of pregnancy during cancer treatment and to curb its consequences in Iran, particularly in Sistan and Baluchestan Province.
3. Methods
This cross-sectional study was carried out between September 2019 and August 2020 on 133 women of reproductive age (15 - 49 years) with cancer, who were referred to Khatam Hospital, Imam Ali Hospital, and Dr. Hashemi's office (an oncologist) for chemotherapy or radiotherapy, in addition to women who had undergone treatment at least one year ago in Zahedan. Regards to sample size, it should be explained that due to uncertain number of women under cancer treatment, census method was employed to find the samples. The subjects were selected by purposive sampling. The inclusion criteria were as follows: absence of infertility; absence of cancers associated with the removal of important reproductive organs; lack of menopause; and living with the spouse even periodically. On the other hand, infertility, the presence of cancers associated with the removal of important reproductive organs, reluctance to interview, and lack of favorable conditions to continue the interview were the exclusion criteria.
A researcher-made questionnaire was used for data collection. The content validity of the questionnaire was examined in this study. The questionnaire was revised, based on the feedback and recommendations of five experts in the fields of family planning and cancer. As the main items of this instrument were gathered from previous studies (25, 26), its face validity was confirmed. A pilot study was performed a month before the main part of the research in order to evaluate the reliability of the questionnaire.
The collected data were analyzed in SPSS-18. For categorical variables, Pearson’s chi-square test was used to find differences between women with and without experience of pregnancy, based on the demographic, sociocultural, and accessibility factors. Fisher’s exact test was also run to see whether the number of observations was below five in any of the nominal variables. Finally, we used multinomial logistic regression to discover the main predictors of pregnancy. The odds ratio (OR) was measured at a 95% confidence interval (CI). The maximum likelihood method was used to estimate the coefficients of logistic regression models. All variables with a P-value less than 0.05 were considered statistically significant. Also, the fitness of the proposed models was assessed using different goodness-of-fit indices, including the Hosmer-Lemeshow (H-L) test and goodness-of-fit measures such as Cox-Snell, R2 and Nagelkerke R2.
4. Results
Table 1 presents the participants’ socioeconomic and demographic characteristics. Overall, 46 (34.6%) of women were 40 - 44 years old, and 52 (39.0%) of women were 30 - 39 years old. Also, 66 (46.6%) of respondents had less three years of age difference with their husbands. In terms of ethnicity, 72 (54.1%) and 55 (41.4%) of respondents were Fars and Baluch, respectively. Regarding education level, 41 (30.8%) and 39 (29.3%) of women had secondary and tertiary education, respectively. In addition, 43 (32.3%) and 36 (27.0%) of respondents respectively said that their husband have tertiary and secondary education. The results showed that 102 (77.0%) of women lived in urban areas, and 96 (72%) were housewives. Also, 22 (16.5%) of respondents mentioned that their husbands had another wife or wives. In terms of power structure in the family 75 (56.4%) and 49 (36.8%) of women mentioned that decisions about major issues and health/medical issues in the family were made jointly and only by their husbands, respectively.
| Variables | No. (%) |
|---|---|
| Age group, y | |
| 15 - 19 | 2 (1.5) |
| 20 - 24 | 9 (6.8) |
| 25 - 29 | 24 (18.0) |
| 30 - 34 | 26 (19.5) |
| 35 - 39 | 26 (19.5) |
| 40 - 44 | 46 (34.6) |
| 45 - 49 | 2 (1.5) |
| Spousal age difference, y | |
| < 3 | 31 (23.3) |
| 3 - 6 | 62 (46.6) |
| 7 - 10 | 29 (21.8) |
| > 10 | 11 (8.3) |
| Ethnicity | |
| Fars | 72 (54.1) |
| Baluch | 55 (41.4) |
| Others | 6 (4.5) |
| Education level | |
| Illiterate | 16 (12.0) |
| Elementary school | 37 (27.8) |
| Secondary school | 41 (30.8) |
| Tertiary school | 39 (29.3) |
| Husband’s education | |
| Illiterate | 19 (14.3) |
| Elementary school | 35 (26.3) |
| Secondary school | 36 (27.1) |
| Tertiary school | 43 (32.3) |
| Occupational status | |
| Housewife | 96 (72.2) |
| Employee | 37 (27.8) |
| Polygamy | |
| Yes | 22 (16.5) |
| No | 111 (83.5) |
| Place of residence | |
| Urban | 102 (76.7) |
| Rural | 31 (23.3) |
| Decisions about important issues are made by | |
| Respondent | 5 (3.8) |
| Husband | 56 (42.1) |
| Jointly | 72 (54.1) |
| Decisions about health/medical issues are made by | |
| Respondent | 9 (6.8) |
| Husband | 49 (36.8) |
| Jointly | 75 (56.4) |
Demographic Background of the Participants (N = 133)
Table 2 shows that the desired number of children was 3 - 4 in 58 (43.6%) of respondents, and 58 (43.6%) of women desired more than four children. Also, 47 (35.3%) of couples did not agree on the number of children, and 22 (16.5%) couples did not agree on the contraceptive method. Almost half of women claimed that they were going to become pregnant in the future. In terms of gender preference, 61 (45.9%) of women preferred to have a boy than a girl. The results also showed that 49 (37.0%) of women did not have any knowledge about the emergency contraceptive methods. Regarding the accessibility factors, 130 (97.7%) of women were less than 30 minutes away from both health centers and pharmacies. Also, 61 (46.6%) of women claimed that the physician responsible for their cancer treatment never discussed contraceptives.
| Variables | No. (%) |
|---|---|
| Desired number of children | |
| 0 | 0 (0) |
| 1 - 2 | 17 (12.8) |
| 3 - 4 | 58 (43.6) |
| > 4 | 58 (43.6) |
| Couple’s agreement on the number of children | |
| Yes | 70 (52.6) |
| No (husband wants more children) | 45 (33.8) |
| No (respondent wants more children) | 2 (1.5) |
| Do not know | 16 (12.0) |
| Do you want to become pregnant in the future? | |
| Yes | 66 (49.6) |
| No | 67 (50.4) |
| Couple’s agreement on the contraceptive method | |
| Yes | 111 (83.5) |
| No | 22 (16.5) |
| Son preference | |
| Yes | 61 (45.9) |
| No | 72 (54.1) |
| Contraceptive method | |
| Withdrawal | 31 (23.3) |
| Condoms | 43 (32.3) |
| Pills | 42 (31.6) |
| No method | 15 (11.3) |
| Other methods | 2 (1.5) |
| Knowledge about the emergency method | |
| Yes | 84 (63.2) |
| No | 49 (36.8) |
| Distance from health centers, min | |
| < 30 | 123 (92.5) |
| 30 - 60 | 10 (7.5) |
| > 60 | 0 (0) |
| Distance from pharmacies, min | |
| < 30 | 130 (97.7) |
| 30 - 60 | 130 (2.3) |
| Did your doctor discuss contraception? | |
| Yes | 71 (53.4) |
| No | 62 (46.6) |
Distribution of Participants Based on Some Fertility and Contraception Indicators (N = 133)
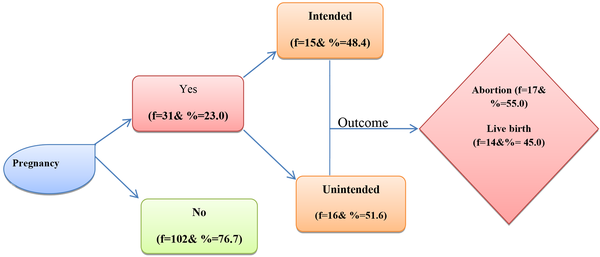
Furthermore, Figure 1 shows that 31 (23.0%) of respondents had the experience of pregnancy during cancer treatment or up to one year after the last chemotherapy or radiotherapy session. In more detail, 15 (48.0%) of pregnancies were unintended, and 16 (51.0%) were intended. In terms of pregnancy outcomes, 17 (55.0%) of women had abortions, and 14 (45.0%) had livebirths.
4.1. Outcome
Table 3 presents a comparison of women with and without experience of pregnancy regarding the demographic, sociocultural, and accessibility factors. The results showed a significant relationship between age and pregnancy (P = 0.001), and the highest pregnancy rate was reported in women aged 20 - 24 years. Also, there was a significant relationship between pregnancy and ethnicity, and the highest pregnancy rate was seen in Baluch women (P = 0.024). The husband’s education level also had a significant relationship with pregnancy (P = 0.014), with the highest rate of pregnancy among women whose husbands were illiterate.
| Variables | Pregnancy | χ2 | P-Value | |
|---|---|---|---|---|
| Yes, No. (%) | No, No. (%) | |||
| Age group | 19.62 | 0.001 | ||
| 15 - 19 | 1 (50.0) | 1 (50.0) | ||
| 20 - 24 | 6 (66.7) | 3 (33.3) | ||
| 25 - 29 | 8 (33.3) | 16 (66.7) | ||
| 30 - 34 | 8 (30.8) | 18 (69.2) | ||
| 35 - 39 | 1 (3.8) | 25 (96.2) | ||
| 40 - 44 | 3 (13.0) | 20 (87.0) | ||
| 45 - 49 | 4 (17.4) | 19 (82.6) | ||
| Spousal age difference, mean | 0.757 | 0.860 | ||
| < 3 | 8 (25.8) | 23 (74.2) | ||
| 3 - 6 | 13 (21.0) | 49 (79.0) | ||
| 7 - 10 | 8 (27.6) | 21 (72.4) | ||
| > 10 | 2 (18.2) | 9 (81.8) | ||
| Ethnicity | 4.77 | 0.024 | ||
| Fars | 12 (16.7) | 60 (83.3) | ||
| Baluch | 15 (27.3) | 40 (72.7) | ||
| Non-Fars | 2 (17.7) | 4 (81.3) | ||
| Respondent’s education level | 3.67 | 0.299 | ||
| Illiterate | 3 (18.8) | 13 (81.0) | ||
| Primary school | 5 (13.5) | 32 (86.5) | ||
| Secondary school | 11 (26.8) | 30 (73.2) | ||
| Tertiary school | 12 (30.8) | 27 (69.2) | ||
| Husband’s education level | 9.41 | 0.014 | ||
| Illiterate | 15 (34.9) | 28 (65.1) | ||
| Primary school | 9 (25.7) | 26 (74.3) | ||
| Secondary school | 7 (19.4) | 29 (80.6) | ||
| Tertiary school | 0.0 | 100.0 | ||
| Employment status | 6.05 | 0.021 | ||
| Employee | 14 (17.7 | 23 (82.3) | ||
| Housewife | 17 (37.8) | 79 (62.2) | ||
| Polygamy | 1.07 | 0.220 | ||
| Yes | 7 (31.8) | 15 (68.2) | ||
| No | 24 (21.6) | 87 (78.4) | ||
| Place of residence | 2.44 | 0.089 | ||
| Urban | 27 (26.5) | 75 (73.5) | ||
| Rural | 4 (12.9) | 27 (87.1) | ||
| Desired number of children | 2.36 | 0.307 | ||
| 1 - 2 | 4 (23.5) | 13 (76.5) | ||
| 3 - 4 | 10 (17.2) | 48 (82.8) | ||
| > 4 | 17 (29.3) | 41 (70.7) | ||
| Couple’s agreement on the number of children | 4.77 | 0.024 | ||
| Yes | 11 (15.7) | 59 (84.3) | ||
| No | 20 (31.7) | 43 (68.3) | ||
| Couple’s agreement on the contraceptive method | 1.20 | 0.188 | ||
| Yes | 27 (24.3) | 84 (75.7) | ||
| No | 4 (18.2) | 18 (81.8) | ||
| Son preference | 1.31 | 0.174 | ||
| Yes | 17 (27.9) | 44 (72.1) | ||
| No | 14 (19.4) | 58 (80.6) | ||
| Did your doctor discuss contraception? | ||||
| Yes | 12 (16.9) | 59 (83.1) | 3.50 | .048 |
| No | 19 (30.6) | 43 (69.4) | ||
| Distance from health centers, min | ||||
| < 30 | 31 (25.2) | 92 (74.8) | 3.28 | 0.063 |
| 30 - 60 | 0 (0.0) | 10 (100.0) | ||
| > 60 | 00 | 0.00 | ||
| Distance from pharmacies, min | 0.173 | 0.552 | ||
| < 30 | 30 (23.1) | 100 (76.9) | ||
| 30 - 60 | 1 (33.3) | 2 (66.7) | ||
| > 60 | 00 | 00 | ||
Comparison of Women with and Without Experience of Pregnancy in Terms of Socioeconomic, Cultural, and Accessibility Factors
In terms of occupation, the results showed that pregnancy had a significant relationship with occupation (P = 0.021), and the highest rate of pregnancy was reported in housewives. Couple’s agreement on the contraceptive method was also another variable with a significant relationship with pregnancy (P = 0.024). The highest rate of pregnancy was found in women who did not agree with their husband about the contraceptive method. Moreover, there was a significant relationship between pregnancy and physician consultation about the contraceptive method (P = 0.048), and the highest rate of pregnancy was obsereved in women, who claimed that their physician did not discuss the contraceptive use.
Table 4 presents the prediction of pregnancy, based on the logistic regression analysis. Also, we calculated the fitness of proposed model using the Hosmer-Lemeshow (H-L) test and goodness-of-fit measures, including Cox, Snell R2, and Nagelkerke R2. The results showed that the main predictors of pregnancy were woman’s age (OR = 0.927, 95% CI: 0.446 - 0.899, P = 0.011), ethnicity (OR = 2.49, 95% CI: 1.02 - 7.719, P = 0.045), and occupational status (OR = 0.358, 95% CI: 0.118 - 0.979, P = 0.46).
| Variables | B | P-Value | OR | 95% CI |
|---|---|---|---|---|
| Woman’s age | -0.457 | 0.011 | 0.927 | 0.446 - 0.899 |
| Husband’s education level | 0.089 | 0.205 | 1.06 | 0.952 - 1.255 |
| Physician consultation with the patient about contraception | 0.506 | 1.69 | 0.533 - 3.580 | |
| Yes | 0.323 | |||
| No | 1 | |||
| Couple’s agreement on the number of children | 0.056 | 0.669 | 975 - 7.033 | |
| Yes | -0.963 | |||
| No | 1 | |||
| Ethnicity | 0.045 | 2.49 | 1.02 - 7.719 | |
| Baluch | 1.033 | |||
| Non-Baluch | 1 | |||
| Occupation | 0.046 | 0.358 | 0.118 - 0.979 | |
| Employee | -1.080 | |||
| Housewife | 1 | |||
| Constant value | -1.864 | 0.344 | 1.96 | - |
Prediction of Pregnancy During the Treatment Period
5. Discussion
The results of the present study showed that 23.0% of women had a pregnancy or pregnancies during chemotherapy or radiotherapy and up to one year after the last session of treatment. In terms of the pregnancy outcomes, 55.0% of pregnancies ended in abortion, and about 45% were live birth. However, Shabazin and Gholamy (27) believed that the actual prevalence of unwanted pregnancy in Iran may be higher than the reported rates, because in the Iranian society, some women tend to hide their unwanted pregnancy from others, which makes it difficult to collect accurate information.
Moreover, the rate of pregnancy in the current study was considerably higher than previous studies. A study by Mody et al. (28) in the US showed that 71% of women did not report pregnancy during their primary cancer treatment, while they were sexually active. Another study based on data from the Basel Breast Cancer Database showed that the rate of unintended pregnancy was only 3.5% (8). Moreover, a study by Kopeika et al. (29) on young female breast cancer survivors (with the median time of six years from the time of diagnosis) in the UK found unintended pregnancies in only 7.0% of women, 58% of which were terminated, and around 2.0% were live births.
In terms of the contraceptive use, although nearly 90.0% of women reported using a contraceptive method, only 67.0% used safe methods (condoms and pills), and 23.0% used the withdrawal method, which is not a safe method; also, about 11.0% of women did not use any methods. The withdrawal method, if used carefully, can be as effective as most non-hormonal barrier methods. Only 4% of women using this method are expected to experience an unintended pregnancy within the first year of use; however, due to the high user error, the rate of unintended pregnancy among users is 27% in the first year (30). Moreover, the withdrawal method, as shown by Bommaraju (31), is not effective, because it is prone to user error and does not allow for female reproductive control. Therefore, it can be said that a considerable percentage of women are at risk of unintended pregnancy.
Moreover, a significant proportion of women (37%) were not familiar with emergency contraception. Similarly, Mody et al. (28) in the US reported that 90% of women with cancer used a form of contraceptive in, and the most common method was condom (52%). However, study by Guth et al. (8) also reported that 58% of women with breast cancer used ineffective contraceptive method.
Regarding the determinants of pregnancy among women, the results showed a significant relationship between age and the incidence of pregnancy, and the highest pregnancy rate was reported in women aged 15 - 24 years. It is clear that younger women have not reached their ideal number of children, compared to older women; therefore, the rate of precedency is higher among younger women, which is consistent with another study in Sistan and Baluchestan (32). The current findings also revealed that occupational status is one of the predictors of pregnancy. In other words, the proportion of housewives who became pregnant during treatment was significantly higher than employed women. This may be due to the fact that the desired number of children is lower in employed women; their authority in the family is higher; and they have more exposure to information about contraceptives and complications of pregnancy during treatment (26, 32).
Ethnicity is a cultural variable, which has a significant relationship with fertility. In this study, most pregnancies were reported in Baluch women. This finding is consistent with the study in Sistan and Baluchestan, which found a significant relationship between ethnicity and fertility behavior (32). On the other hand, Asadisarvestani (32) found no significant relationship between ethnicity and fertility behavior in Shiraz County. It was concluded that other social, economic, and cultural factors can undermine the role of ethnicity (26). It seems that the higher fertility rate in Baluch women versus Persian women is due to the impact of variables, such as higher childbearing value, less education, and lower employment rates, affecting fertility behavior and ideals in a certain way.
Physician consultation was one of the predictors of pregnancy. A significantly lower rate of pregnancy was found in women who received advice from their physician about contraception. Moreover, the results showed that half of the respondents claimed that their doctor did not discuss contraception. It is believed that contraceptive counseling by physicians made the patients more likely to use contraception, compared to patients who received no counseling (18). Previous studies have also revealed that 10% - 65% of reproductive-age survivors received contraceptive counseling after their cancer diagnosis (16, 18, 19). Some women might have forgotten the received advice about contraception but it should be accepted that a set of complex variables can affect the quality of counseling. More explanation, the limited number of medical centers and specialists in Zahedan has led to overcrowding; therefore, doctors may pay less attention to consultation about reproductive health issues.
Cultural factors also play an important role. Contraception conversations may be unlikely in clinic rooms, as providers focus on cancer treatment plans and outcomes, and patients may be uncomfortable initiating questions or may be unaware of the need to discuss their concerns with the doctors. Physicians may not clearly explain the issue to patients due to cultural restrictions. The discomfort surrounding contraception is exacerbated if family members are present and the provider is of the opposite gender (18, 33, 34). In addition, since a considerable number of women have low levels of education, they may not accurately understand their physician’s advice regarding pregnancy and contraception.
A study by Crafton (35) showed that only 57% of gynecologic oncologists believed that their patients understood the possibility of unplanned pregnancy during treatment. Research to date suggests that cancer survivors do not receive adequate counseling about safe and effective contraceptives during or after cancer treatment (16, 31, 36). Oncologists should advise patients on the contraceptive methods and the risk of pregnancy before starting treatment until they have achieved good health. The contraceptive efficacy and the adverse effects of each method should be discussed in relation to cancer diagnosis and treatment, as some drug interactions may lower the contraceptive efficacy (36, 37). It is suggested that oncologists refer patients of reproductive age to gynecologists to ensure proper contraceptive counseling (8, 16).
While 90% of women in the present study were close to the health centers (< 30 minutes), the findings showed that a considerable percentage of women purchased contraceptives from pharmacies, while pharmacies, in most cases, did not provide enough information about the contraceptives; this could affect their knowledge of contraceptives, and consequently, lead to a higher rate of failure. Therefore, family planning service providers and physicians need to pay more attention to the delivery of adequate and accurate information about contraceptives to improve the rate of contraceptive use and reduce pregnancy in this group of women, particularly with attention to this fact that the desired number of children was above two in 86.0% of participants in this study, and nearly 50% of them planned on becoming pregnant in the future. The findings of a study by Kopeika et al. (29) in the UK also found that 41% of young breast cancer survivors showed tendency to have children. Similarly, a study by in Beirut, Lebanon, revealed that 30.76% of women wanted more children at the time of diagnosis (38).
It should be noted that contraceptive counseling is not only necessary for women, but is also essential for their husbands, as they play an important role in their partners’ reproductive choices and behaviors. This issue is especially important, as the present findings revealed that important decisions in the family are made by men and that their education level is one of the main predictors of pregnancy during treatment; nevertheless, the education level of 40.0% of men was low in this study, and a considerable number of them desired more children that their wives. In other words, 34% of husbands did not agree with their wives about the number of children, and 17% disagreed about contraception; couple’s agreement on the number of children was one of the main predictors of pregnancy.
Major efforts are needed to increase the spouses’ awareness of the risk of pregnancy during cancer treatment and the importance of contraception (32, 39), because if couples agree on the number of desired children, their agreement about other issues, such as the interval between childbirth and contraceptive use, is greater. These findings are consistent with the results of other studies, which found that men played an important role in women’s ability to make fertility-related decisions (32, 39-43).
In sum, contrary to the common belief that women with cancer are less likely to become pregnant, physicians and family planners should pay more attention to fertility preferences to provide the necessary information for their patients. According to Maslow et al., counseling recommendations for contraceptive use during treatment, besides addressing abstinence and safer sex practices, enable patients to feel more confident in their relationships, help them better express their sexual desires and preferences, and promote their awareness about the risks of unprotected sex (43).
Furthermore, considering the important role of demographic, cultural, and social variables in the incidence of pregnancy during treatment, physicians must pay more attention to the role of these factors to reduce the pregnancy rate and its consequences. Also, due to the widespread presence of health centers in different areas, it can be effective to refer patients along with their spouses to these centers to receive the services and information needed in the field of family planning. Since few studies have been conducted on reproductive health and family planning among women with cancer, it is recommended to conduct similar studies in other regions, especially in areas where the fertility and unintended pregnancy rates are higher.
5.1. Strengths and Limitations
The main strength of this study was its attention to socio-economic factors in addition to the role of accessibilities and structural factors. Furthermore, to the best of our knowledge, this study is the first study on this topic in Iran.
In terms of limitations, the main limitation of this study was its method. More explanation, the method of this study was quantitative, while the mixed method study can bring more depth knowledge. Moreover, the population of this study was limited to Sistan and Baluchestan Province.
5.2. Conclusions
Despite many advances in family planning in Iran, similar to many countries, the rate of unintended pregnancy is high in Iran, especially in areas with a lower socioeconomic status. Women with cancer are a vulnerable group in the community. Contrary to our expectations, not all pregnancies that occurred during the treatment period were unintended, which indicates the shortcomings of family planning programs, such as inadequate attention to vulnerable groups for family planning services and lack of proper communication between medical centers, family planning centers, and couples. Therefore, reducing the rate of pregnancy and its complications among women with cancer depends on multiple factors, such as improving the educational programs and enhancing the relationship between medical centers, family planning centers, and couples. However, this goal cannot be achieved without scientific and accurate knowledge of demographic, social, and cultural characteristics and other influential factors.