1. Background
Overactive bladder (OAB) syndrome, a condition with urgency (which could be together with urge incontinence), is mostly presented with increased daytime and nocturnal urine frequency (1). Overactive bladder is a highly prevalent condition that drastically impacts the quality of patients’ life. Overactive bladder prevalence in former studies was reported 7% to 27% in men and 9% to 43% in women. This prevalence increases with age and physical inactivity, and it is more common in females than males (2-5).
Urgency, as an essential symptom of OAB, has been reported to cause nocturia and incontinence (6). The International Continence Society (ICS) describes nocturia as an emergency need to urine once or more at night (in sleep time), which can negatively affect sleep quality, and consequently, the patients’ energy, health status, and quality of life (7-9).
We speculate that sleep disturbance and fatigue, which have a noticeably high prevalence in patients with OAB, adversely affect all aspects of health and can cause anxiety, depression, and mental disorders, and as a result, can deteriorate OAB symptoms (10-12).
2. Objectives
To the best of our knowledge, nocturia is a frequent complaint among OAB patients that can adversely affect their sleep quality. Hence, in this study, we compare sleep disturbance and fatigue in women with OAB (case group) and without OAB (control group) by using validated questionnaires (Pittsburgh sleep quality index [PSQI] and Fatigue Severity Scale [FSS]).
3. Methods
This case-control study was conducted among 140 patients including 70 women with OAB and 70 women in the control group, who visited the Gynecology and Urogynecology clinic at Yas Hospital affiliated to Tehran University of Medical Sciences (TUMS) from Aril 2019 to May 2020.
This research was performed in accordance with the Helsinki Declaration and was confirmed by Tehran University of Medical Sciences ethics committee (code: IR.TUMS.MEDICINE.REC.1398.025). All the patients signed an informed consent form.
Overactive bladder diagnosis was made by taking the subjects’ medical history, using other diagnostic tools (if needed), and administering the three incontinence questionnaires. The control group was selected from the women visiting gynecology clinics. The requirements for the inclusion of subjects in the control group included no former OAB diagnosis, no pelvic discomfort, no voiding dysfunction, and no evidence of active urinary infection.
Non-pregnant women with OAB were assigned to the case group, and women with stress urinary incontinence (SUI) or stress-predominant mixed urinary incontinence (MUI), neurologic disorders, such as multiple sclerosis, CVA, and spina bifida, symptoms of urinary tract infection, OAB treatment, and pregnancy were excluded.
Sleep disturbance and fatigue symptoms were evaluated by using proved questionnaires, including PSQI and FSS in both groups.
3.1. Pittsburgh Sleep Quality Index
The PSQI includes 19 items assessing sleep quality and disturbance during the previous month. All the items are divided into seven categories, including (1) sleep duration; (2) sleep disturbance; (3) sleep latency; (4) daytime dysfunction due to sleepiness; (5) sleep efficiency; (6) overall sleep quality; and (7) sleep medication use.
The value of each question is between 0 to 3; the total score is obtained with question value summation that is between 0 to 21, with higher total scores showing poor sleep quality in participants. A total PSQI score > 5 is considered a proper cutoff for poor sleep detection (13). The Persian version of this questionnaire has a validity of 0.86 and a reliability of 0.89 (14).
3.2. Fatigue Severity Scale
The FSS is a short questionnaire aimed to assess the fatigue effect. The FSS consists of nine components that measure the symptoms related to fatigue degree over the previous week. Lower scores (e.g., 1) yield an intense disagreement with the question, while higher scores (e.g., 7) show an intense agreement.
The total score of lower than 36 reveals the absence of fatigue and a total score of 36 or more indicates “Further evaluation by a physician may be needed” (15). The Persian version of this questionnaire has a validity of 0.96 and a reliability of 0.93 (16).
3.3. Statistical Analysis
All the statistical analyses were performed using SPSS version 24.0 (IBM, New York, USA). Independent t-test and non-parametric Mann-Whitney U-test were applied to test mean differences. The chi-square test was used to test for differences in proportion. A P-value of less than 0.05 was considered as the level of statistical significance.
4. Results
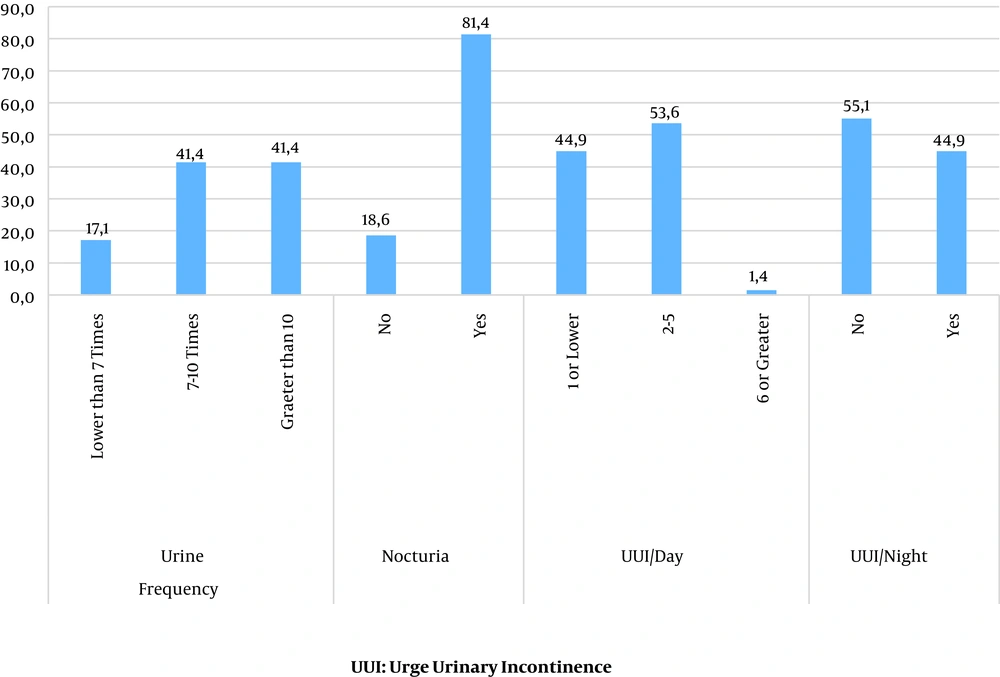
The mean age of the 140 participants was 44.50 ± 12.64 years old. The majority of the participants were married (78.6%), and nulli parity was reported in 9.7%, menopause in 39.3%, hysterectomy in 11%, and smoking in 7.9% of the cases. In OAB patients, different symptoms, including urine frequency per day, having nocturia, urgency, and urinary incontinence in the day and in night are evaluated (Figure 1).
The mean PSQI score was 13.24 ± 3.67 (range: 6 to 22). All the participants experienced different degrees of poor sleep quality (PSQI > 5); however, there was a significant difference (P < 0.001) between the case and control groups in terms of global PSQI score. The PSQI subscales scores for each group are presented in Table 1.
| PSQI Subscale Score | Women with OAB | Control Women | P-Value |
|---|---|---|---|
| Sleep duration | 0.89 ± 0.12 | 1.40 ± 0.10 | 0.002 |
| Sleep disturbance | 1.25 ± 0.06 | 1.10 ± 0.04 | 0.050 |
| Sleep latency | 1.64 ± 0.12 | 1.13 ± 0.11 | 0.004 |
| Daytime dysfunction due to sleepiness | 0.98 ± 0.12 | 0.91 ± 0.11 | 0.671 |
| Sleep efficiency | 1.56 ± 0.16 | 0.95 ± 0.14 | 0.007 |
| Overall sleep quality | 1.46 ± 0.13 | 0.97 ± 0.09 | 0.004 |
| Sleep medication use | 0.76 ± 0.14 | 0.33 ± 0.10 | 0.014 |
| Global PSQI score | 14.73 ± 0.45 | 11.82 ± 0.37 | < 0.001 |
Pittsburgh Sleep Quality Index Among the Participantsa
The mean FSS score was 39.05 ± 15.12 (range: 9 to 63), and the questionnaire showed that 58.6% of the participants were suffering from fatigue (FFS ≥ 36). Additionally, there was a significant FFS score difference (P-value < 0.001) between the case and control groups. The FSS subscale mean scores are shown in Table 2.
| Fatigue Severity Scale | Women with OAB | Control Women | P-Value |
|---|---|---|---|
| My motivation is lower when I am tired. | 5.34 ± 0.26 | 4.31 ± 0.23 | 0.005 |
| Exercise make me tired. | 5.19 ± 0.25 | 3.59 ± 0.21 | < 0.001 |
| I am easily fatigued. | 4.59 ± 0.26 | 3.56 ± 0.22 | 0.004 |
| Fatigue interferes with my physical functioning. | 5.40 ± 0.23 | 4.33 ± 0.20 | 0.001 |
| Fatigue causes frequent problems for me. | 4.91 ± 0.24 | 3.44 ± 0.20 | < 0.001 |
| My fatigue prevents sustained physical functioning. | 5.27 ± 0.24 | 3.59 ± 0.20 | < 0.001 |
| Fatigue interferes with carrying out certain duties and responsibilities. | 5.04 ± 0.26 | 3.64 ± 0.21 | < 0.001 |
| Fatigue is among my three most disabling symptoms. | 4.76 ± 0.27 | 3.43 ± 0.20 | < 0.001 |
| Fatigue interferes with my work, family, or social life. | 4.57 ± 0.27 | 3.14 ± 0.22 | < 0.001 |
| Total score | 45.07 ± 1.90 | 33.02 ± 1.38 | < 0.001 |
Fatigue Severity Scale Among the Participantsa
In women with OAB, there was a positive significant correlation (P = 0.007) between PSQI and FSS scores. This correlation was also observed between urgency urinary incontinence at night and PSQI (P = 0.047) and between nocturia and FSS score (P = 0.032).
5. Discussion
The study showed that compared to the control group, sleep quality was significantly poorer in OAB patients. In fact, in these patients, nocturia, and urgency urinary incontinence at night have an adverse impact on their sleep efficiency and could deteriorate sleep disturbance. Furthermore, in OAB patients, urgency and urinary incontinence during the day negatively affect their daytime functions.
The cause of OAB has not been vividly identified in the literature. However, changes in autonomic functions might be the underlying cause of OAB. In particular, OAB symptoms, including nocturia and urgency, are significant factors affecting sleep disruption. In fact, nocturia is probably a main reason for awakenings in patients with OAB (17, 18). On the other hand, frequent awakening at night results in severe fatigue for doing daytime activities (19). Given this, OAB symptoms adversely influence patients’ quality of life.
It is worth mentioning that poor sleep quality has been considered as an important risk factor for some diseases. Former studies have shown that sleep disorder is associated with depression, dementia, cardiovascular disease, and autonomic dysfunction (20-24). Similar to our study, women with urgency urinary incontinence suffer from poor sleep quality. It seems that omen with urgency urinary incontinence diagnosis should be assessed for sleep disorders so that they can be treated with proper medical agents (18).
Several studies have suggested that multicomponent treatment should be considered as the first-line therapy for OAB patients. It seems that using OAB treatment methods may increase bladder stability and improve sleep quality (17, 25).
Overactive bladder treatment includes pharmacologic agents such as anti-muscarinic drugs and non-pharmacologic treatments such as guided slow-paced respiration, sleep restriction, and stimulus control. Although many patients who had used these treatments reported improvement in their sleep quality, considerable controversies concerning the outcome of clinical trial studies in post-OAB treatment period exist (17, 26, 27).
Small sample size was one of the limitations of our study. Another limitation was related to the short period of the study that did not permit evaluating the effect of OAB treatment on the patients’ sleep quality. Therefore, future studies are suggested to address the impact of assessing OAB treatment on PSQI score.
Finally, it is recommended that in patients with the chief complaint of sleep disorder, the physician ask about urinary problems before prescribing sleep medications. Because the patient may not talk about urinary issues due to shyness, nocturia and urge incontinence could be considered as the main causes of their sleep disorders.
The study illuminated that sleep disorders are common in patients with OAB, and it seems urinary problems assessment is a prerequisite for any sleep medication prescription.