1. Background
Healthcare-associated infection is one of the most common unwanted side effects of health care services in hospitalized patients, which can increase mortality and impose many costs on society. These infections do not occur during hospitalization or the incubation phase but occur 48 hours after hospitalization or 7 to 30 days after discharge (1). On average, 7% of patients in developed countries and 10% in developing countries suffer from at least one type of nosocomial infection at admission, and about 10% of patients die from these infections (2).
Catheter-associated (CA) bacteriuria is one of the most common healthcare-associated infections resulting from the extensive use of urinary catheters. As known, 15 to 25% of hospitalized adults are catheterized due to urinary retention and urine output examination following surgery or as a result of severe disease, and for therapeutic and diagnostic purposes (3). Each day of Foley catheterization increases the risk of bacteriuria by 3 to 7% (4). Meanwhile, a significant amount of workforce and money is used by medical centers to reduce catheter-associated bacteriuria, especially when bacteriuria shows the signs and symptoms of Catheter-associated urinary tract infection (5).
Commonly, and especially in females, by inserting the catheter into the urinary tract, the microbes surrounding the urethra and perineal area stick to the catheter surface and enter the bladder, creating a potential for bacterial colonization in the urine (6). Catheter-associated bacteriuria can cause significant complications such as antibiotic-resistant organisms, lower and upper urinary tract infections, bacteremia, recurrent fevers, kidney and bladder stones, and increased length of stay and hospitalization costs (7). It is estimated that 65 to 70% of catheter-associated urinary tract infections can be prevented by taking infection control measures (8). Patients would be prone to urinary tract infections when healthcare providers do not follow the infection-control instructions such as hand washing, urethral cleaning before catheterization, performing sterile techniques when inserting the catheter, and pulling it out as soon as possible (9).
In recent years, many studies have been conducted on reducing the chances of urinary tract infections, such as using antimicrobial agents, disinfecting the catheter site, and washing the bladder after catheterization. On the other hand, some evidence shows that periurethral cleaning with antiseptics before catheterization reduces the risk of urinary tract infections (10). According to the study by Clayton on urinary catheters and ways to prevent hospital-acquired infection, it is recommended to use an antiseptic for cleaning before catheterization (11). According to the Centers for Disease Control and Prevention guidelines, a sterile or antiseptic solution is needed to clean the periurethral area, but the type of the antiseptic solution is not yet known (4).
Povidone-Iodine is the most commonly used antiseptic in skin disinfection and pre-catheterization cleansing. However, research is ongoing on other compounds to detect a more proper solution with fewer clinical complications, faster act, and more cost-effectiveness. As an antiseptic, chlorhexidine has antimicrobial effects similar to povidone-iodine. However, unlike povidone-iodine, it does not lose its properties while exposed to blood and serum proteins and creates a more prolonged disinfection effect on the skin. According to various studies, chlorhexidine performs better in disinfecting hands and surgical sites than iodine (12). However, the results are contradictory regarding pre-catheterization cleansing, which raises the need for further research. Nasiriani et al. (13) compared water and povidone-iodine for cleaning in female patients before catheterization, concluding that water is more cost-effective than iodine concerning the bacteriuria rate. In the study by Duzkaya et al. (9) and Cheung et al. (14), chlorhexidine was found to be more effective than iodine and normal saline in reducing bacteriuria, whereas Fasugba et al. (10) reported no statistically significant difference between the impacts of antiseptics, water, and normal saline after catheterization on urinary tract infection rates.
2. Objectives
The present study compares the impacts of povidone-iodine and chlorhexidine to introduce a more suitable antiseptic for reducing bacteriuria in female patients undergoing catheterization.
3. Methods
Study participants were 110 female patients above 18, meeting the inclusion criteria, hospitalized in the Emergency Department of Al-Zahra Hospital affiliated with Isfahan University of Medical Sciences. This study was a single-blind clinical trial in which the sample was unaware of group assignment. The sample was selected by convenience sampling. We provided adequate explanations about the study, obtained written informed consent, and explained the study's objectives to the patients.
Due to the high probability of sample loss, 220 female patients over 18 years admitted to the Emergency Department of Al-Zahra Hospital of Isfahan University of Medical Sciences who met the inclusion criteria were selected as the sample. Demographic and clinical questionnaires were completed, and the patients were randomly divided into two groups of povidone-iodine and chlorhexidine using Minimization Software, based on confounding variables including age, consciousness level, triage level, nutritional status, and underlying diseases. According to the following formula, the sample size was estimated at least 32 people in each group. Concerning a 10% sample loss, 36 people were enrolled in each group.
The inclusion criteria were the need for Foley catheterization, no experience of urinary tract infection within two weeks before admission, no fever above 38°C at the time of inclusion, no history of allergy to the antiseptics used in the study, no apparent periurethral injuries, and no Foley catheterization at the time of admission. The exclusion criteria were the unwillingness of the patients and their families to participate, the removal of Foley catheter earlier than five days, discharge, transfer to another ward, and patient’s death earlier than five days.
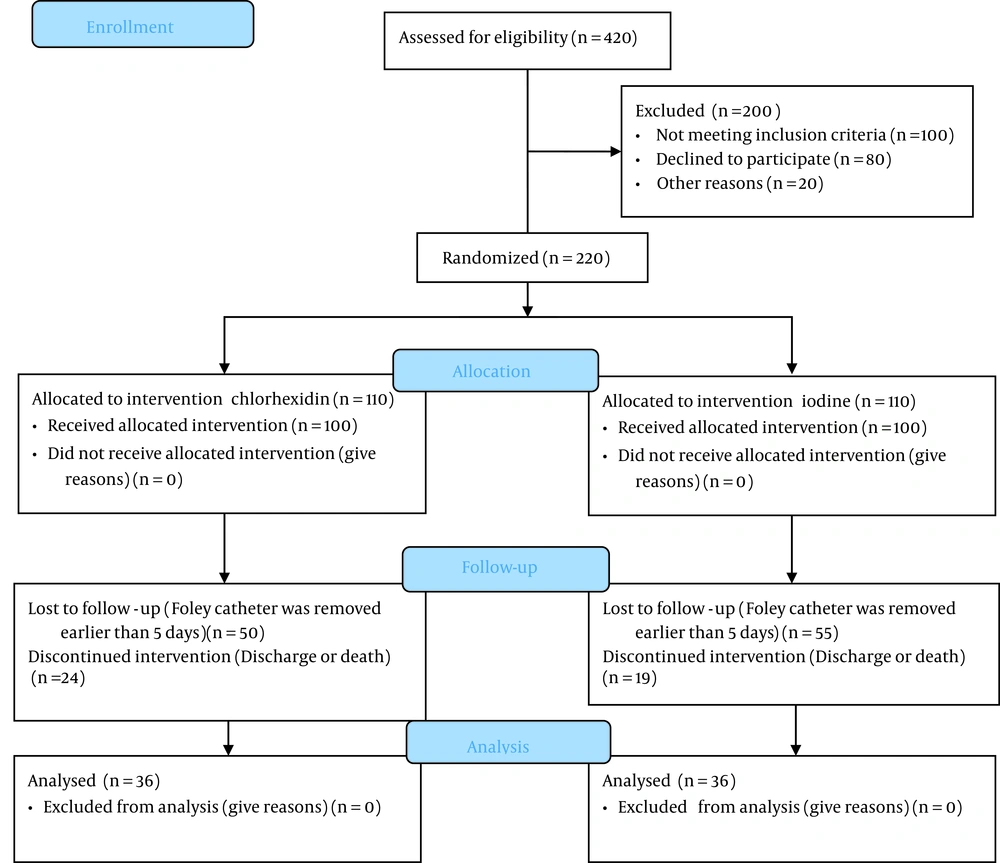
In this study, bacteriuria and pyuria-positive specimens were not excluded to prevent excessive sample dropout. Then, the bacteriuria and pyuria rates were compared in three sessions after the intervention. The nature of the study was explained to each patient, and informed consent was obtained. The study protocol was approved by the Ethics Committee of Isfahan University of Medical Sciences with the ethics code IR.MUI.RESEARCH.REC.1397.378. The patient enrollment algorithm is illustrated in Figure 1. Also, we registered the study in the clinical trial registry with the RCT code IRCT20170712035044N2.
The patients admitted to the emergency department who met the inclusion criteria were divided into two groups using Minimization Software. The periurethral and perineal areas were cleaned using povidone-iodine solution 10% in group 1 and chlorhexidine solution 2% in group 2. The researcher and a trained colleague did the cleansing procedure by their dominant hands from the top of labia majora to the rectal area (downwards) using a sterile technique with an antiseptic gauze and then dried the area (15). After the standard sterile catheterization, a 10 cc urine specimen was collected in a sterile urine container for urinalysis and urine culture examination using a syringe needle (no. 25) after disinfecting the elastic part of the catheter with alcohol. The specimens were submitted to the lab in less than two hours and were cultured in blood agar, which the technician approved at the hospital laboratory.
The patient's demographic information, including the cause of hospitalization, underlying diseases, the level of triage, age, and other characteristics, as well as the document number, was recorded in the questionnaire for future follow-ups. The Foley catheter was monitored as per hospital routines by an assistant nurse. During the second and third sessions, urinalysis and urine culture specimens were submitted respectively 72 hours and five days after catheterization, following the above instructions. Notably, 74 samples were excluded from the study due to unwillingness, Foley catheter removal earlier than five days, discharge, transfer to another ward, or the patient’s death earlier than five days, and finally, 36 individuals were studied in each group.
Data collection was done using a demographic questionnaire, urinalysis, and urine culture test. The more than 103/mL urine colony count was considered positive bacteriuria and WBC ≥ 10/HPF positive pyuria (16).
4. Results
A chi-square test was used to determine and compare the frequency distribution of pyuria between the povidone-iodine and chlorhexidine groups. The McNemar test was used to determine and compare the frequency distribution of pyuria in each group. The chi-square test and Fisher's exact test were used to determine and compare the bacteriuria frequency distribution after catheterization between the povidone-iodine and chlorhexidine groups. The Mann-Whitney (non-parametric) test was used to determine and compare the mean number of microorganisms after catheterization. The Friedman test was used to determine and compare the mean number of microorganisms after catheterization in each group.
Statistical analysis showed no significant difference in the independent variables between the two groups (P > 0.05). The three parameters of the number of microorganisms, bacteriuria rate, and pyuria rate were compared immediately, 72 hours, and five days after catheterization. According to the chi-square test, no significant difference was observed in the number of bacteriuria-positive cases between the two groups, immediately (P = 0.76), 72 hours (P = 0.22), and five days (P = 0.50) after catheterization (Table 1).
| Time | Chlorhexidine Group, No. (%) | Povidone-iodine Group, No. (%) | Chi-square Test | |
|---|---|---|---|---|
| χ2 | P-Value | |||
| Immediately after catheterization | 6 (16.7) | 7 (19.4) | 0.09 | 0.76 |
| 72 hours after catheterization | 21 (58.3) | 26 (72.2) | 1.53 | 0.22 |
| 5 days after catheterization | 35 (97.2) | 34 (94.4) | - | 0.50 |
There was no significant difference in the number of pyuria-positive cases between the two groups immediately after catheterization (P = 0.80). However, 72 hours (P = 0.03) and five days (P = 0.004) after catheterization, this rate was significantly higher in the povidone-iodine group than in the chlorhexidine group (Table 2).
| Time | Chlorhexidine Group | Povidone-iodine Group | Chi-square Test | |
|---|---|---|---|---|
| χ2 | P-Value | |||
| Immediately after catheterization | 12 (33.3) | 13 (36.1) | 0.06 | 0.80 |
| 72 hours after catheterization | 23 (63.9) | 30 (80.3) | 4.15 | 0.03 |
| 5 days after catheterization | 20 (55.6) | 31 (86.1) | 8.13 | 0.004 |
The number of microorganisms in the three sessions did not follow the normal distribution, so the Mann-Whitney test was used to compare the mean number of microorganisms between the two groups at different times. The results showed no significant difference in the number of microorganisms between the two groups immediately (P = 0.93), 72 hours (P = 0.43), and five days (P = 0.61) after catheterization (Table 3).
| Time | Chlorhexidine Group (Mean ± SD) | Povidone-Iodine Group (Mean ± SD) | Mann–Whitney Test | |
|---|---|---|---|---|
| P-Value | Z | |||
| Immediately after catheterization | 6972.29 ± 20419.51 | 3125.22 ± 10019.53 | 0.93 | 0.08 |
| 72 hours after catheterization | 20180.56 ± 34123.97 | 17527.78 ± 30538.25 | 0.43 | 0.80 |
| 5 days after catheterization | 40430.56 ± 38814.05 | 46277.78 ± 41688.20 | 0.61 | 0.51 |
In the first urine culture (immediately after catheterization), 16.7% of the patients in the chlorhexidine group and 19.4% in the povidone-iodine group were bacteriuria-positive. According to the results, there was a 41.6% increase in the bacteriuria rate within 72 hours of catheterization in the chlorhexidine group. This rate increased by 58.2% in the povidone-iodine group. Within five days after catheterization, 80.5% of the patients in the chlorhexidine group and 75% in the povidone-iodine group were bacteriuria-positive.
Besides, E. coli was the most common bacterium cultured in the chlorhexidine group (55%) and povidone-iodine group (42%). According to the chi-square test, there was no significant difference in the frequency of microorganisms between the two groups (P > 0.05).
5. Discussion
The results showed no significant difference in the number of bacteriuria-positive cases and microorganisms between the povidone-iodine and chlorhexidine groups 72 hours and five days after catheterization. However, the pyuria rate was significantly higher in the povidone-iodine group than in the chlorhexidine group 72 hours and five days after catheterization. Little research has studied the bacteriuria rate in pre-catheterization cleansing with antiseptics, primarily focusing on the impact of antiseptics compared to sterile or tap water.
According to the results of the study by Cheung et al., to compare the impact of water and chlorhexidine on bacteriuria in pre-catheterization cleansing in patients with a fixed catheter, the bacteriuria rate was 60% in the chlorhexidine group and 75% in the sterile water group seven days after catheterization (17). In the present study, an 80% increase in the number of bacteriuria-positive cases was observed in the chlorhexidine group within five days, which is inconsistent with Cheung’s study. It seems to be due to different criteria in defining bacteriuria. In Cheung’s study, the bacteriuria threshold was considered higher than 105 CFU/ mL. However, in the present study, this rate was considered to be above 103 CFU/ mL (16).
In 2017, Kara and Özyürek conducted a study entitled “The effect of periuretral care and follow-up on bacteriuria in patients with urinary catheter: A comparison of three solutions” (14). This study showed no statistically significant difference in the bacteriuria rate between the groups. According to this study, no significant difference was observed between the impacts of chlorhexidine and povidone-iodine and the impacts of sterile water and normal saline on the bacteriuria rate. However, the present study aimed to compare the effects of chlorhexidine and povidone-iodine on the bacteriuria rate in catheterized patients.
Duzkaya et al. conducted the study “Povidone-iodine, 0.05% chlorhexidine gluconate, or water for periurethral cleaning before indwelling urinary catheterization in a pediatric intensive care: a randomized controlled trial” on 122 infants of one to 18-months-old (9). The patients were randomly divided into three groups of 40 individuals. Then, periurethral cleaning was done by povidone-iodine, chlorhexidine, or sterile water, depending on the group. A urine specimen was submitted every three days until the catheter removal, and the incidence of urinary tract infection was investigated along with the clinical symptoms. According to the results, 15% of the patients in the povidone-iodine group, 4.5% in the chlorhexidine group, and 7.5% in the sterile water group developed urinary tract infections. In this study, the bacteriuria incidence rate was not referred to, and the percentage of urinary tract infection in each group was expressed according to clinical symptoms. Although there was no statistically significant difference between the groups in this study, the incidence rate of urinary tract infection was clinically lower in the chlorhexidine group than in the other groups, consistent with the present study.
According to the definition of Foley catheter-associated urinary tract infection, both bacteriuria and pyuria indicators should be considered simultaneously (18). The most common microorganism cultured in urine tests was E. coli, which is consistent with the results of other studies. The mean age of women in this study was 68. According to the statistics, 20% of women above 65 have bacteriuria without catheterization (19), while 60% to 80% of the patients using fixed catheters develop bacteriuria, consistent with the present study (20). The study by Nasiriani et al., entitled “Comparison of the effect of water vs. povidone-iodine solution for periurethral cleaning in women requiring an indwelling catheter prior to gynecologic surgery" is consistent with the current study in terms of age and sex. That the urinary tract infection rate is different between males and females adds to the validity of the results (13).
To enroll patients without a previous history of catheterization, we conducted this study on patients hospitalized in the emergency department. Some of the study's limitations were the patients’ acute clinical condition, the commute of the clients and the staff in the department, and frequent relocations for paraclinical procedures such as CT scans and endoscopies that caused problems with catheter care. Therefore, it is recommended to conduct other studies on more clinically stable patients in other in-patient departments.
5.1. Conclusions
The study showed that the bacteriuria rate was lower in patients cleaned with chlorhexidine before catheterization than in those in the povidone-iodine group. Although this difference between the two groups was not statistically significant, the pyuria rate was significantly lower in the chlorhexidine group than in the povidone-iodine group, both 72 hours and five days after catheterization. Therefore, due to the fewer side effects of chlorhexidine, it is recommended to conduct further studies with chlorhexidine for periurethral cleaning before catheterization to reduce bacteriuria and pyuria, provided that its higher impact is confirmed. This method can lead to a decrease in urinary tract infections in patients with a urinary catheter.