1. Background
In December 2019, a cluster of severe respiratory infections was reported in China. This disease was the third coronavirus that emerged in the last two decades (1, 2). Previous experiences with major epidemics such as influenza and SARS show that monitoring infectious disease behavior and reporting the disease cases are essential factors for early detection and rapid public health response. Disease early detection can reduce mortality, complications, and costs associated with the disease (3, 4).
The effectiveness of disease reports depends on the timeliness and accuracy of medical record documentation (3). There are comprehensive health information systems (HISs) for reporting infectious diseases in United States, Netherlands, United Kingdom, and Canada (5-9). These HISs contain complete information about different variables of the diseases (3, 10, 11). Figar et al. reported that data in the hospital information system showed an outbreak of flu two weeks before the Ministry of Health national alert in Buenos Aires, Argentina, in 2009. As well, he showed that HIS plays an important role in assessing the morbidity and mortality due to the outbreak (8).
HISs have played a vital role in responding to the COVID-19 pandemic and fundamentally changed the type of consumers-healthcare interactions and the way in which healthcare services are delivered (12). Their critical functions, such as sustained data sharing, patients’ monitoring, and their contacts tracing, community risk sensitization and engagement, public education, and timely preparedness and response activities, could improve the pandemic management (13).
2. Objectives
Health information systems have major impacts on improving decision-making process about procedures, programs, and health policies during the outbreak. The current study explored health information systems (HISs) challenges based on HIS’s manager viewpoint in the teaching hospitals in one of the largest states of Iran during the COVID-19 pandemic.
3. Methods
3.1. Research Setting
This qualitative study was conducted in referral teaching hospitals for patients with COVID-19 at Mashhad University of Medical Sciences.
3.2. Research Design
The study was conducted using content analysis and started one month after the Iranian officials announced the COVID-19 outbreak, from April 2020 to May 2020.
3.3. Participants
All HIS’s managers who were working in referral teaching hospitals of Mashhad University of Medical Sciences for COVID-19 and had long experience in health information management (HIM), were invited to participate.
3.4. Data Collection Methods
In the present study, data were collected in two phases: In the first phase, all HIMs who were invited, reported their challenges about HISs via official letters. Due to the lack of sufficient information about some of the extracted codes from mentioned letters, semi-structured interviews were conducted with the same participants in phase two (among managers who consented to participate, using purposeful sampling). The interview questions were determined and confirmed during an expert panel. Because of the high risk of COVID-19 transmission, participants refused to conduct face-to-face interviews, so semi-structured interviews were performed by telephone.
3.5. Data Analysis
In the first phase, each of the challenges was carefully evaluated by two researchers, separately. For each letter, all semantic units were extracted, collected, and coded in an Excel worksheet. Then, these initial codes were analyzed and grouped using the constant comparison method and inductive content analysis to discover the main themes. In the next step, the researchers compared the extracted codes to identify existing similarities and differences. Similar codes were combined in this step. In case of disagreement, a decision was made based on the majority vote of the researchers.
In the second phase, the interviewees’ contents were recorded and analyzed in full detail in Microsoft word document, after each interview was completed. If new data acted as a response to the ambiguities in the first phase, the data were analyzed according to previous codes. But, if new semantic units were found in the interviews, the data were considered a new code.
3.6. Ethical Considerations
This study was approved by the Ethics Committee of Mashhad University of Medical Sciences in April 2020 (Ethical code: IR.MUMS.REC.1399.108). Moreover, the participants were ensured of data confidentiality and autonomy. They were informed of the purpose of the study and the voluntary nature of their participation. Written informed consent was obtained from all participants before recording the interviews.
4. Results
4.1. The Characteristics of the Hospitals and Participants
health information systems managers in 18 hospitals participated in the study. The characteristics of the hospitals and participants are shown in Tables 1 and 2.
| Characteristic | Values |
|---|---|
| General/ surgical beds | |
| 10 - 24 | 0 |
| 25 - 49 | 2 |
| 50 - 99 | 3 |
| 100 - 199 | 5 |
| 200 - 299 | 2 |
| 300+ | 2 |
| Geography | |
| Large urban | 6 |
| Suburban | 8 |
| Variables | Values |
|---|---|
| Gender | |
| Male | 3 |
| Female | 5 |
| Age (y) | 33.5 ± 5.6 |
| Education level | |
| Bachelor degree | 8 |
| Master degree | 1 |
| Years of experience in using HIS | 8.6 ± 5.6 |
4.2. The Challenges of HISs
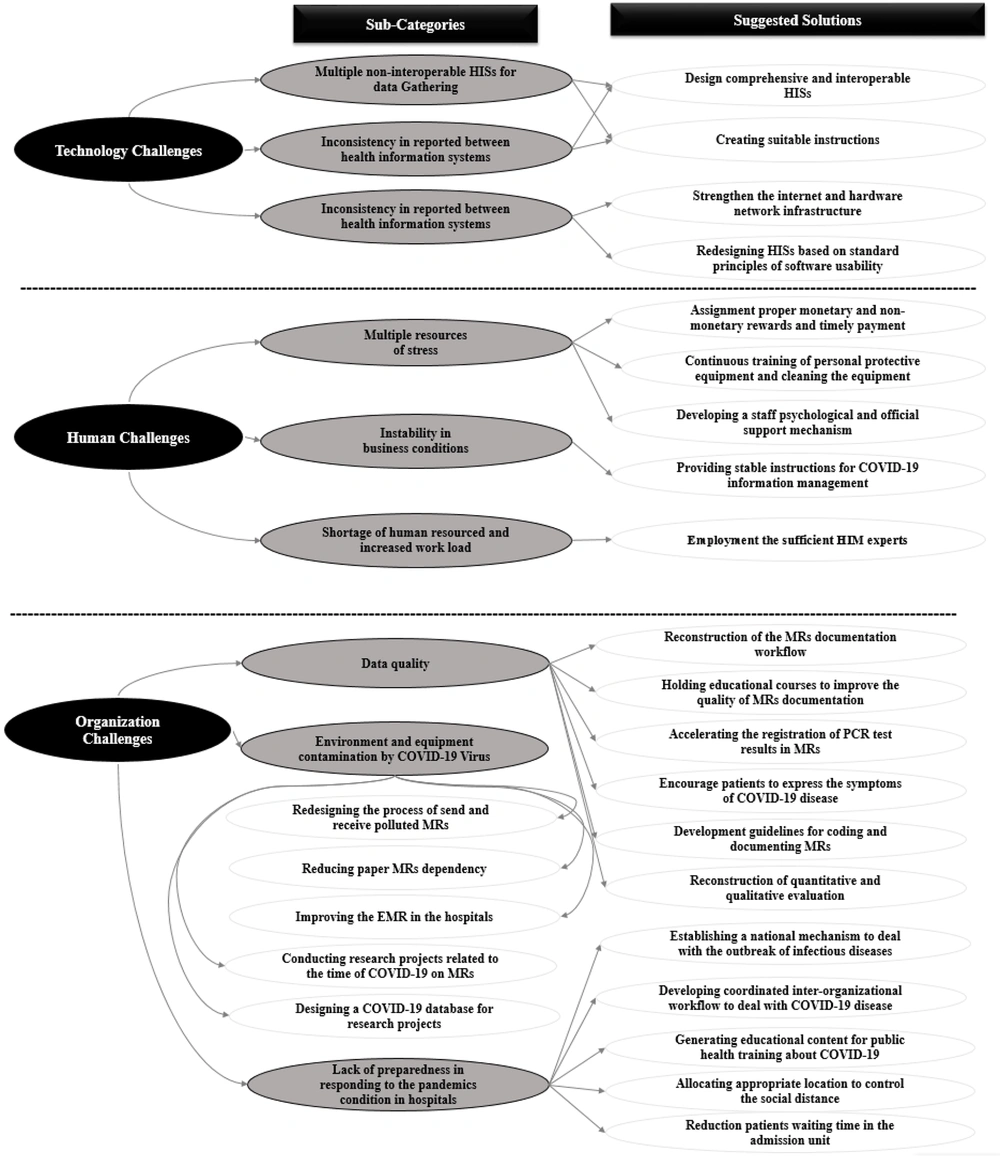
The 46 challenges and 24 solutions by HIS managers were classified into three categories: technology, organization, and human (Figure 1).
4.2.1. The Technology Category
The first category was technology category, which included three sub-categories: Multiple non-interoperable HISs, inconsistencies between reports of HISs, and lack of suitable hardware equipment.
The first challenge was the presence of multiple non-interoperable HISs for data gathering. The COVID-19 data are registered in multiple information systems including the paper-based medical records, hospital information system (as the main source of electronic data collection tool), MCMC (a web-based system to collect clinical data), COVID-19 registry (a standalone system to gather data for research purposes), SINA system and National Health Portal (NHP) (web-based systems to collect data for health home purposes), FARABAR and AVAB system (the web-based systems to collect data for statistical purposes). These systems have considerable overlaps and do not have interoperability with each other. These HISs were developed due to the lack of coordination between different organizations such as governmental departments, insurance companies, academic units, and medical research departments.
Our results showed that there were no uniform standards and transparent instructions for designing, recording, and managing health information in HISs. Therefore, the systems produced inconsistent statistical reports. This problem led to a mass problem for the end-users. The end-users had to enter patients’ data into these systems in parallel, compare the syntaxes and reports, and found out why these reports were inconsistent. After the users explore the reason for inconsistent in the reports, all systems should be corrected by users that were a very time-consuming process. For example, the request for the PCR test (the main diagnosis laboratory test for COVID-19) was recorded in the hospital information systems, but the test results were reported in the NHP, without any data exchange. So, the users must fulfill the related fields of hospital information systems, based on the PCR test results in the NHP. Due to possible end-users’ mistakes or losing the test results, the late test results preparation process was not equal to the number of requests and results of the PCR test between NHP and HISs.
Lack of suitable hardware and communication equipment was another important challenge (including insufficient computer hardware like mouse or keyboard for data entry, frequent interruption of the internet or HISs). Figure 1 shows the themes, sub-themes, and suggested solutions-technology challenges.
4.2.2. The Organization Category
The second category of HIS challenges was the organization category that included three sub-categories: data quality, environment, and equipment contamination, and lack of sufficient preparedness in responding to the pandemics in hospitals.
The participants reported a number of reasons for low data quality, such as registration of primary diagnosis by admission staff in the patient medical records. As well, participants believed that the contamination of paper medical records by COVID-19 virus led to a delay in assigning the ICD-10 code and quantitative and qualitative evaluation process.
The necessity of documenting patients’ signatures and fingerprints in consent forms, preparing copies or scans of paper medical records for legal and insurance issues, as well as the lack of scientific evidence for effective methods of disinfecting polluted equipment were the most important challenges of the second category of organization.
Another challenge declared by the participants was the lack of sufficient preparedness in responding to the pandemics condition in hospitals. Participants believed that the issuance of contradictory instructions by the Ministry of Health, weak cross-sectoral cooperation between different levels of health service delivery (first, second, and third levels), and lack of sufficient information about the behavior of the COVID-19 virus were considerable organizational challenges in the third category. Figure 1 shows all HIS challenges and participants’ solutions in the organization category.
4.2.3. The Human Category
The third category was the human category, which had three subsets: multiple resources of stress, instability in business conditions, shortage of human resources, and increased workload. Many resources exacerbated stress in HISs end-users. For example, “uncertainty about the proper monetary and non-monetary reward for working in referral hospitals” was an important reason. Particularly, when the participants compared their monetary with other health care professionals in the hospital. They declare that HISs users were exposing to COVID-19 virus, similar to other healthcare professionals in the hospitals, because of infected medical records and environment. But, they do not receive proper monetary.
Another important source of stress in the staff was daily negative feedback about inconstancy in statistic reports and low data quality in HISs by the senior management. Since the existing multiple non-interoperable was the main reason for these issues and end-users could not improve data quality or inconstancy in statistic reports. Figure 1 shows themes, sub-themes, and suggested solutions.
5. Discussion
In the current study, the challenges of HISs in COVID-19 were investigated qualitatively. The results of the present study showed that some challenges refer to the structure of HISs, and some of them occurred due to the lack of experience in the face of the outbreak of COVID-19. The most important results of the current study will be discussed in the following.
The results of our study showed that “multiple non-interoperable HISs for data gathering” challenge refers to the HISs architecture in Iran. Our results showed that the lack of coverage of clinical function in the HISs has led to develop and use of multiple HISs for gathering clinical information. Multiple HISs were designed to cover this shortcoming. For example, MCMC has an important role in COVID-19 for gathering clinical data. Parts of patients’ clinical data were gathered by HIS, while other parts were registered in the MCMC, SINA system, etc. In COVID-19, this problem shows itself more than before. Managing and incorporating the health information and statistical reports in multiple HISs became an important issue. Moghaddasi et al. showed that more than 80% of Iranian hospitals now use HISs, which creates an opportunity to develop a nationwide real-time data collection infrastructure. But, existing HISs encompasses functions including administrative, financial, admissions, discharge, transfers, para clinical data, and very limited clinical function such as a summary of record (14). Jahanbakhsh et al. believed that already there are no proper long-term strategic plans for HIS design, development, and improvement in Iranian hospitals (15). As well, in line with our results, the results of the study by Barzekar et al. showed that one of the main challenges for HIS’s users was lack of adequate education and inadequate allocation of budget to them (16).
Our results showed that many legal, financial, and social barriers must be overcome before Iran as a developing country can realize the full potential of the electronic health information in the HISs. For example, the participants in the current study believed that paper medical records were unclean and could disseminate the severe acute respiratory syndrome coronoavirsu-2 (SARS-CoV-2) in the hospital. Already, the medical record summary sheet exists in most Iranian HISs. But the courts and insurance organizations need to review a paper copy of medical records for responding to legal and financial issues. Sittig reported the same results in the US as a developed country. He said that although the robust and rapid infrastructure for health information collection and exchange is available in the US, many legal and social barriers must be solved before fully use the full potential of this infrastructure. The legal system lags behind adoption of new technologies, including HISs, and offers little guidance to navigate the transition from paper-based to electronic medical records. For example, many health information exchanges depended on patients’ consent model. Therefore, healthcare organizations resist participating entirely in these exchanges due to concerns about losing patience and the revenue stream to their care (17). In addition, Fahey and Hino demonstrated that the lack of a consensus on privacy protection in the digital data gathering, especially contact tracing for COVID-19, creates risks for privacy implementation and for reassuring citizens (18).
Lack of sufficient preparedness to respond to the pandemics in the hospitals was one of the challenges of HISs in the current study, which included the challenges such as inconsistency in university management units against COVID-19, contradictory instructions, weak inter-sectoral cooperation, lack of sufficient information about COVID-19, and lack of sufficient space to separate patients. These results tie well with previous studies. Peiffer-Smadja et al. reported a number of challenges that a hospital in French to respond to the COVID-19 outbreak, such as anticipating the increase of cases, managing healthcare workers’ anxiety, increased need for healthcare workers, many research and teaching activities, maintaining teaching activities, and real-time information of the healthcare workforce (19). Singer believed that there are serious gaps in responding to the COVID-19 pandemic even in developed countries. Reduced availability for health professionals, a long period of time needs to provide adequate supplies of effective vaccines for the Europe region alone, unreliability many of diagnostic tests and digital health solutions were a number of serious gaps (20). Shrestha et al. investigated nationwide preparedness for COVID-19 in Nepal’s hospitals. They found out 39.7% of the hospitals in the country admit patients with COVID-19. But, most of them are not well prepared for the management of these patients. For example, supply of personal protective equipment was inadequate in the hospitals (21). Patan hospitals (a city in Nepal) faced resource constraints during the COVID pandemic (22).
The low data quality of the MRs, such as incomplete primary diagnosis field and lack of clear instructions for assigning ICD-10 coding was another important challenge in our study. In line with our results, Pan American health organization (PAHO) reported that many organizations have swiftly adopted remote working arrangements (23). Meanwhile, the continuity and quality of statistical information reporting may be faced with exceptional conditions of controlling the performance of day-to-day operations underlying statistical reporting (24). In line with the previous studies, the participants in our study reported that rapid changes in governmental instructions for data management, including ICD 10 coding. Anderson et al. said that certifying deaths due to COVID-19 guidance might be updated, if necessary when clinical guidance on COVID-19 evolves (25). Kazemi-Arpanahi et al. believed that providing the data quality criteria in COVID-19 registry data elements and their values should be determined for reporting COVID-19. They developed a comprehensive COVID-19 registry that can provide an in-depth description of specific patient cohorts rather than delivering epidemiological data (26).
5.1. Conclusions
The findings of the current study, provide valuable scientific evidence for health information system challenge during the COVID-19 pandemic in Mashhad, which is the second-largest city of Iran as a developing country. It seems that reconstruction of health information systems, revision of medical record documentation processes, and holding training courses for users, and planning to deal with pandemics, human resource support programs are very necessary.