1. Background
There have been several emerging viral diseases since 1980s. Currently, coronavirus disease 2019 (COVID-19) caused by SARS‐CoV‐2 has spread throughout the world (1).
In December 2019, a new coronavirus appeared in Wuhan, China. Then, the number of patients increased, and it spread rapidly in almost all countries in the world (2, 3). SARS-CoV-2 is the cause of the severe acute respiratory syndrome epidemic known as COVID 2019 (4). On March 11, 2020, the World Health Organization (WHO) announced the disease as a ‘global pandemic’ (5).
COVID-19 pandemic has had a great impact on reducing organ donation and transplantation activities (6). The risk of transmission of COVID-19 from a donor is unknown (7). Recent guidelines recommend that all potential donors be tested for SARS-CoV-2, and positive donors must be suspended. Asymptomatic individuals who are in contact with COVID-19 patients are removed from the donation list (2).
The incidence rate and impact of COVID-19 have been reported to be very different. Some countries have reported the rate of donation to be reduced to less than 50% during the pandemic (8).
In the UK, compared with 2019, the number of brain death donors decreased by 66% and the number of transplants decreased by 68% (6). However, COVID-19 has had no significant effect on the number of deceased organ donors in Hong Kong (9), Slovenia, and Germany (10).
On February 19, Iran confirmed two cases of death due to COVID-19, which rapidly spread throughout the entire country (6). According to the Iranian Ministry of Health and Medical Education (MOHME), all activities related to donation and transplantation were halted in March 2020 and then resumed again.
2. Objectives
The aim of this study was to determine the donation and transplantation activities before and after COVID pandemic in Iran.
3. Methods
This retrospective study used the questionnaire designed by Ahmed et al. (11) to compare the deceased organ donation and transplant activities between two specific 9-month periods, March to December 2020 and the same length of time of the last 2 years (2018 - 2019). The survey assessed rates of donation after brain death before and after COVID-19 in a 9-month period. Organ donation system in Iran is donation after brain death.
Questionnaires were sent by email to chief executives of organ procurement units (OPU). From all OPUs in Iran, 15 OPUs chose to participate in western, northern, southern, eastern, middle, southeastern, northwestern, northeastern, southeastern regions of Iran. The questionnaire included the numbers of brain death confirmations, family consents for donation, organ recoveries, solid organs transplanted, cause of brain death, and the new experience of remote working of organ procurement staff after COVID-19.
We also compared the rate of potential donor (a patient whose clinical condition is suspected to fulfill brain death criteria (12)) and eligible donor (the diagnosis of brain death is confirmed, and there are no previously known contraindications to donation (12)) during the two time intervals.
The summary of results for the continuous variables is presented as numbers and percentages for variables. The median (± IQR) changes in continuous outcome variables between two interval times were assessed with Wilcoxon non-parametric test. A P-value less than 0.05 was considered as statistically significant. All data were analyzed using SPSS16 software.
4. Results
The median numbers of organ donations, potential donors, family consents, and marginal donors were dramatically decreased after COVID-19 pandemic. These variables between the two time intervals are compared in Table 1.
| Variables | December 2018 - March 2019 (Number) | March - December 2020 (Number) |
|---|---|---|
| Brain death confirmations | 409 | 332 |
| Number of organ donations | 343 | 84 |
| Number of potential donors | 361 | 192 |
| Family consents | 214 | 133 |
| Number of marginal donors | 112 | 85 |
Additionally, the medians of organ donations, potential donors, family consents, and marginal donors during the two time intervals were investigated. The Wilcoxon test revealed significant changes between the medians of organ donations (5.6 ± 0.95 vs. 11.86 ± 2.15, P = 0.0187), potential donors (12.8 ± 2.43 vs. 24.06 ± 4.19, P = 0.005), and family consents (8.86 ± 1.93 vs. 14.12 ± 2.52, P = 0.002) during 2020 and average of 2018-2019 years. In addition, there was a significant change between median of eligible donors during the two time periods (2.5 ± 0.53 vs. 3.98 ± 0.63, P = 0.009).
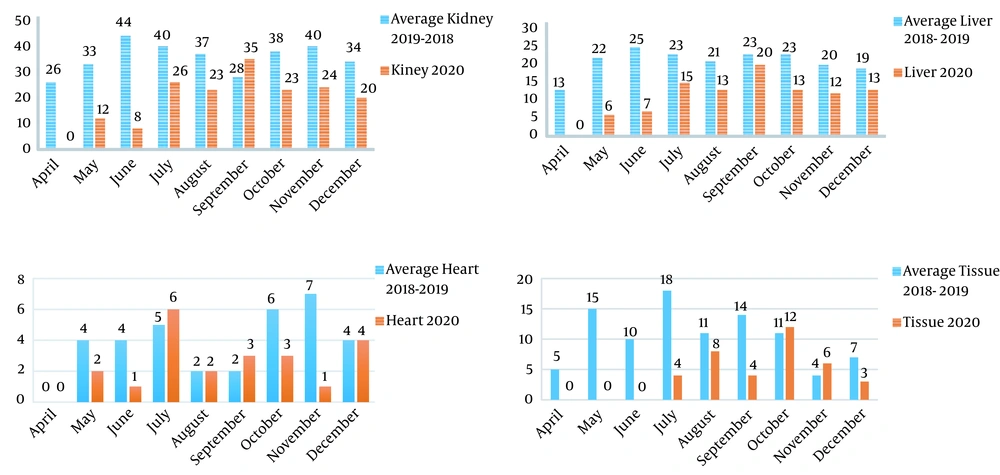
The largest reduction was seen in tissue transplants (62%) during two time intervals. Similar decreases of various magnitudes were seen in liver (48%), kidney (48%), and heart (36%) transplants in two time intervals without a significant impact on new waitlist additions. Non-urgent organ transplantations such as pancreas, small bowel, and lung were suspended in these centers. Guidelines were designed in an organ‐specific manner.
Kidney, liver, and heart donor transplant volumes underwent a noticeable decrease after COVID 19 pandemic (Figure 1).
In spite of head trauma rate changing significantly in two time intervals (median 10.06 ± 2.41 vs. 6.2 ± 2.15, P = 0.05), the other cause of brain death did not change significantly during the two time intervals. Brain death by suicide was increased by 14.44% during the COVID-19 pandemic compared to 2018 - 2019 period (Table 2).
| Cause of Brain Death | Average Period of March - December 2019 | March - December 2020 |
|---|---|---|
| Trauma | 178 | 95 |
| Heart attack | 81 | 59 |
| Suicide | 9 | 13 |
| Drug abuse | 29 | 25 |
| Anoxia | 13 | 6 |
| Tumor | 15 | 17 |
| Other | 15 | 7 |
5. Discussion
The impact of the SARS-CoV-2 pandemic on donation and transplantation system was unprecedented. Since the number of COVID‐19 patients is dramatically increasing, all transplantation strategies adapt their protocols in relation to the risk of viral transmission (13). Similar to other countries, in Iran, deceased donation and transplantation programs significantly changed their routine protocols and halted performing all types of transplantations, and all OPUs’ activities were suspended in March 2020.
In updated guidelines after COVID-19 in Iran, epidemiological, clinical, and laboratory assessment of all potential deceased donors and testing all recipients and donors for COVID-19 were recommended. All donor and recipient candidates in the COVID‐19 period were referred for SARS-CoV-2 reverse transcription polymerase chain reaction (RT-PCR) testing or computed tomography (CT) imaging of the chest without evidence of COVID‐19, and all transplantations with a positive RT‐PCR were canceled. Provinces with high burden of COVID-19 infection had reductions in donation and transplantation volume compared to the same period in 2018 - 2019. OPU directors reported an increase in remote referral responses; this was consistent with the study by Ahmed et al. (11) reporting that most programs in some OPUs had changed to telephone consultation for follow-up.
In our study, family consent decreased by 32% in 2020 compared to the same period in 2018 - 2019. Also, four OPU centers had increased telephonic approaches for family consent. According to pervious studies, the first step for family consent is eye contact and face-to-face interactions (14). Phone interview with families and not having face-to-face consultations might negatively affect the results of family consent. Similarly, Ahmed et al. (11) reported that organ authorization in the USA decreased by 11% after COVID-19 pandemic due to telephonic approaches with donor families for both initial contact and follow-up correspondence. Gain et al. (15) showed that the acceptance rates on the telephone were lower than face-to-face interviews during COVID-19 period.
According to this study, there was a remarkable decline (75.52%) in deceased donation during the two time intervals. Due to COVID-19, the rate of eligible donors significantly decreased. These changes reveal that COVID-19 pandemic has had a strong impact, reducing organ donation and transplantation.
In our study, the number of marginal donors and rate of actual and potential donors decreased. One of the reasons for this issue might be the restrictions on the age of donors. Hence, the criteria for marginal donors changed, and the maximum age for kidney donation was reduced to 60 years without having any risk factors. Liver transplants were received only from brain death cases, and donation from alive individuals was cancelled. Similarly, in the UK, the maximum age for deceased organ donor was reduced to 60 years at first and then increased to 75 years following reduced rate of COVID-19 infection (8).
In this study, the largest reduction was seen in tissue transplantation, and all types of deceased donor transplantation volumes dramatically decreased after COVID-19.
In the COVID-19 period in Canada, heart transplants were only performed in patients with critical conditions, although small bowel transplants were suspended (16).
Our results showed that the number of organ donations due to head trauma significantly decreased in 2020 compared to the average period of 2018 - 2019. According to our results, the suicide rate increased in 2020 compared to the average period of 2018 - 2019.
One of the reasons for the decreased brain death rate seems to be the decreased number of intercity travels and remote working due to pandemic restrictions. On the other hand, the increase in suicide events in the mentioned period is probably due to the negative psychological effects of COVID-19.
There was a decrease in transplantation events during the COVID-19 pandemic worldwide (8, 11, 13, 17). As COVID-19 is still a serious public health risk, OPUs need to develop strategies to address challenges in various sectors to improve outcomes of donation, particularly among those requiring urgent life-saving intervention (18).
The impact of COVID-19 pandemic on donation and transplantation is unprecedented, with our results showing a significant reduction in donation and transplantation. Accordingly, it is necessary to develop appropriate protocols and establish new strategies to evaluate organ donation so as to ensure the safety of recipients and medical staff.