1. Background
Menopause is a natural phenomenon that results from loss of ovarian activity and permanent cessation of menstruation. The most common symptoms are hot flashes described as periodic feeling of heat and sweating associated with chills, palpitations, anxiety, pressure in the head and chest, a burning sensation, nausea, choking, and lack of focus (1), which normally last for three minutes (2).
Hot flashes usually occur around 50 - 52 years of age, along with a decline in estrogen production (3). About 80% of women experience hot flashes within the first three months after menopause, and women in industrialized countries spend about one third of their lives in menopause (4).
The pathophysiology of hot flashes is unknown. However, reduction and cessation of estrogen production plays an important role in changing brain neurotransmitters and instability in the hypothalamic thermoregulatory center. Although hot flashes and sweats do not jeopardize life (5), they result in anxiety, severe discomfort, and social dysfunction, ensure time and women’s careers, and eventually reduce their quality of life (6).
The treatment of choice for hot flashes is estrogen replacement therapy which reduces the symptoms up to 80 - 90%, but it also causes side effects like heart attack, cardiovascular diseases, infarction, thromboembolism, and breast cancer (7). Furthermore, 10% of women are banned from consuming estrogen. Therefore, hormone therapy is applied in less than 20% (8). Studies in Iran have shown that only 9.1% of women prefer to use hormones to treat hot flash (9).
Several other medications like progestin, antihypertensive medications, anti-dopaminergic medications, ergot alkaloids with mild painkillers, tranquilizers, antidepressants, alpha-adrenergic agonists (10), vitamins E have been recommended for treating hot flashes (11). Although these medications are effective and have some benefits, they have many adverse effects like irregular vaginal bleeding, constipation, breast tenderness and pain, mood swings (12), addiction (2), myocardial infarction (13), endometrial cancer, gall stones, hypertension, breast cancer thrombophlebitis, and glucose intolerance (14), which sometimes restrict hormone replacement therapy in older ages.
Alternative therapies like diet, sports, aromatherapy, homeopathy, meditation, and herbal medicine have increased in the past decade, all of which have been effective in alleviating menopause symptoms (15). In fact, using herbal medicines and phytoestrogens represent a diverse group of non-steroidal natural products, which seem to have some estrogenic effects and are often marketed as food supplements. The population being exposed to phytoestrogens is potentially increasing, in part because of an unfavorable risk-benefit profile of hormone replacement therapy (16). Furthermore, few studies have investigated the impacts of herbs containing phytoestrogen like soy (17), licorice (18, 19), and Pimpinella anisum (20). In this regard, P. anisum (aniseed) (21) has been used as antispasmodic, carminative, expectorant, and galactagogue for centuries (22).
Pimpinella anisum L. is an annual herb indigenous to Iran, India, Turkey, and many other warm regions in the world. Chemical studies have demonstrated the presence of eugenol, anethole, methylchavicol, anisaldehyde, and estragole as the major compounds of the fruit essential oil of P. anisum. Eugenol and estragole have been reported to show anesthetic, hypothermic, muscle relaxant, and anticonvulsant activities. Furthermore, anethole possesses muscle relaxant effect. Pimpinella anisum has estrogenic effects and is nearly free from adverse effects, and its simple use has attracted the attention of researchers and postmenopausal women (23). This medicine is available in different forms such as pills, syrups, drops, and oil (22).
2. Objectives
Considering the high prevalence of hot flashes, its adverse effects and treatment challenges, as well as people’s increased tendency to complementary medicine and herbs, the present study aimed at determining the effect of P. anisum extract on treatment and recurrence of hot flashes of postmenopausal women in Tehran, Iran in 2019.
3. Methods
3.1. Study Design
The present double-blind, randomized controlled parallel-group clinical trial was registered at www.irct.ir (code: IRCT201103284317N4). The patients were randomly assigned into two groups of experimental and control. Considering the type I error probability of 5%, power function of 80%, and effect size of 6%, the sample size was determined as 72 individuals using the following formula:
Es (Effect size) = 0.6
Zβ = 0.85
Zα = 1.96
3.2. Sampling
Using a purposeful sampling method, the researcher attended the selected health centers and invited patients by reviewing their files. The aims of the study were explained to all participants, and a written informed consent was obtained from them prior to the study. Then, according to inclusion and exclusion criteria, the participants were randomly assigned into two groups of experimental and control (table of random numbers based on computer random sequence).
The inclusion criteria were being literate or having a literate person at home, aged 45 - 60 years old, body mass index (BMI) < 29, amenorrhea for one to three years, experiencing hot flashes and not taking any medications or hormones to alleviate them, no history of known diseases, not taking antidepressants and tranquilizers, being married or passage of at least one year of their husband’s death, not having experienced major stressors (death of first-degree relatives, divorce, etc.) during the last six months, not being vegetarian, not having history of allergy to herbal medications, and no history of estrogen-receptor positive cancers in participants or their first-degree relatives.
The exclusion criteria included consuming phytoestrogen foods for three consecutive days, unwillingness to continue cooperation and any unknown side effects during the study.
3.3. Setting and Data Collection
We included patients referred to the health centers of medical sciences universities in Tehran, Iran, from 2 May 2018 to 1 February 2019. Questionnaires and information forms were used, and the validity of the research tool was confirmed using content validity and test-retest reliability with a correlation coefficient of 94%. The first questionnaire included demographic data, menstrual history, pregnancy history, physical activity, frequency and severity of hot flashes, and methods used to treat hot flashes; this questionnaire was completed before beginning the treatment. The second questionnaire included the patients’ activities during the previous week, including sports, unpleasant life events, and the methods used to treat hot flashes; this questionnaire was completed by the researchers at the end of each week. The third questionnaire assessed the severity of hot flashes experienced by participants using the Visual Analog Scale (VAS) at the end of each week. The first information form was filled out by the participants and included such information as daily food consumption from two weeks before starting the treatment until the end of the study. The participants were asked to avoid foods containing phytoestrogens during the study days. The second information form contained frequency and severity of hot flashes on a daily basis, and was filled out by the participants from two weeks before starting the treatment until the end of the study. Forms were collected at the end of each week. A Weighting Scale (Seca, Iran) and metal tape (made in Italy) were used to measure weight and height, respectively. The rigid metal tape was used so that climatic conditions would not affect it. The reliability of the scale was initially measured using a two-kg weight and was calibrated using the same weight after every ten measurements.
3.4. Intervention
The aniseeds (seeds of P. anisum) were purchased from herb shops in Tehran (herbarium code: SBMU-8207) and identified in our laboratory. The seeds were milled by electrical grinder and extracted by 96% ethanol (Maceration method × 3). The solvent was evaporated at 40°C, and the waxy extract was mixed by corn starch. The mixed powder was filled in capsules (size 000). The placebos were prepared by starch in same capsules.
After a two-week control, both groups were matched considering such variables as age, duration of amenorrhea, starting time of hot flashes, as well as frequency and severity of hot flashes. Since the study was double-blind, the medicines were coded by a fellow pharmacist such that neither the researcher nor the participants were aware of the capsule content. The group receiving P. anisum took capsules containing 330 mg P. anisum extract, and the placebo group took capsules containing 330 mg starch. All capsules looked similar. The participants took capsules for eight weeks, three times a day. To study the recurrence of hot flashes, the participants were followed up for four weeks after discontinuing the medication.
3.5. Statistical Analysis
The data were analyzed using SPSS version 21. The intra-group average of frequency and severity scores were compared for primary and secondary outcomes using repeated measures analysis of variance (ANOVA), and independent t-test was used to compare the scores between the two groups.
4. Results
In this study, 72 postmenopausal women were randomly assigned into two equal groups of experimental and control (n = 36 each) (Table 1). To remove the effect of confounding variables, both groups were matched in terms of duration of amenorrhea and frequency and severity of hot flashes. As Table 1 shows, the demographic characteristics were similar in both groups.
| Variables | Pimpinella anisum (n = 36) | Control (n = 36) | P-Value |
|---|---|---|---|
| Age (y) | 52.93 ± 3.38 | 52.56 ± 3.39 | 0.29 |
| BMI | 23.31 ± 3.66 | 22.22 ± 2.82 | 0.44 |
| Spouse’s career | 0.33 | ||
| Businessman | 20 (55.5) | 29 (72.7) | |
| Employee | 7 (19.4) | 4 (11.2) | |
| Worker | 9 (25.1) | 6 (16.6) | |
| Level of education | 0.09 | ||
| Illiterate | 11 (30.5) | 12 (23.3) | |
| Primary | 16 (44.4) | 17 (47.2) | |
| Secondary | 5 (14.1) | 3 (8.3) | |
| High school or higher | 4 (11.0) | 4 (11.2) | |
| Residence | 0.19 | ||
| Private | 18 (50) | 18 (50) | |
| Rental | 16 (44.4) | 14 (38.8) | |
| Relatives | 2 (5.6) | 4 (11.2) | |
| Parity | 3.3 ± 0.4 | 3.8 ± 0.9 | 0.09 |
| Age at menarche | 12.8 ± 0.3 | 13.2 ± 0.5 | 0.33 |
| Time from last menstrual period (y) | 1.2 ± 0.3 | 1.7 ± 0.7 | 0.24 |
| Living child | 3.2 ± 1.2 | 3.5 ± 0.9 | 0.61 |
The Distribution of Research Samples in Terms of Demographic-Obstetric Characteristics in Pimpinella anisum and Control Groups a
The frequencies of hot flashes during the study are presented in Table 2. The t-test showed that the mean frequency of hot flashes was similar in both groups before the treatment, but there were significant differences in anisum groups from the first week of treatment (7.89) to the eight week (1.04) and the follow-up period (4.21) (P = 0.001). There was no significant reduction in the control group (P = 0.75). According to the results of the repeated measure ANOVA, while there was a significant difference between the mean frequency of hot flashes during the treatment and follow-up period in the experimental group (P < 0.001), the difference was not significant in the control group.
| Time of Treatment | Groups | P-Value | |
|---|---|---|---|
| Pimpinella anisum (n = 36) | Control (n = 36) | ||
| Before the therapy | 7.89 ± 5.67 | 6.86 ± 3.15 | NS |
| 1st week | 4.70 ± 3.61 | 6.89 ± 3.31 | 0.002 |
| 2nd week | 4.17 ± 4.51 | 6.85 ± 3.28 | 0.001 |
| 3nd week | 4.16 ± 2.42 | 6.82 ± 3.26 | 0.001 |
| 4nd week | 2.82 ± 2.30 | 6.81 ± 3.25 | 0.001 |
| 5nd week | 2.33 ± 2.10 | 6.77 ± 3.28 | 0.001 |
| 6nd week | 1.92 ± 1.80 | 6.79 ± 3.24 | 0.001 |
| 7nd week | 1.48 ± 1.60 | 6.91 ± 3.30 | 0.002 |
| 8nd week | 1.04 ± 1.24 | 6.73 ± 3.22 | 0.001 |
| 1st week of follow-up | 1.23 ± 1.31 | 6.83 ± 2.98 | 0.001 |
| 2nd week of follow-up | 1.44 ± 1.18 | 6.71 ± 3.32 | 0.001 |
| 3nd week of follow-up | 3.76 ± 1.75 | 6.85 ± 3.26 | 0.001 |
| 4nd week of follow-up | 4.21 ± 2.03 | 6.78 ± 3.22 | 0.001 |
| Test result over time | P = 0.001 | P = 0.75 | |
Comparing the Frequency of Hot Flashes Before, During, and After the Treatment in the Pimpinella anisum and Control Groups a
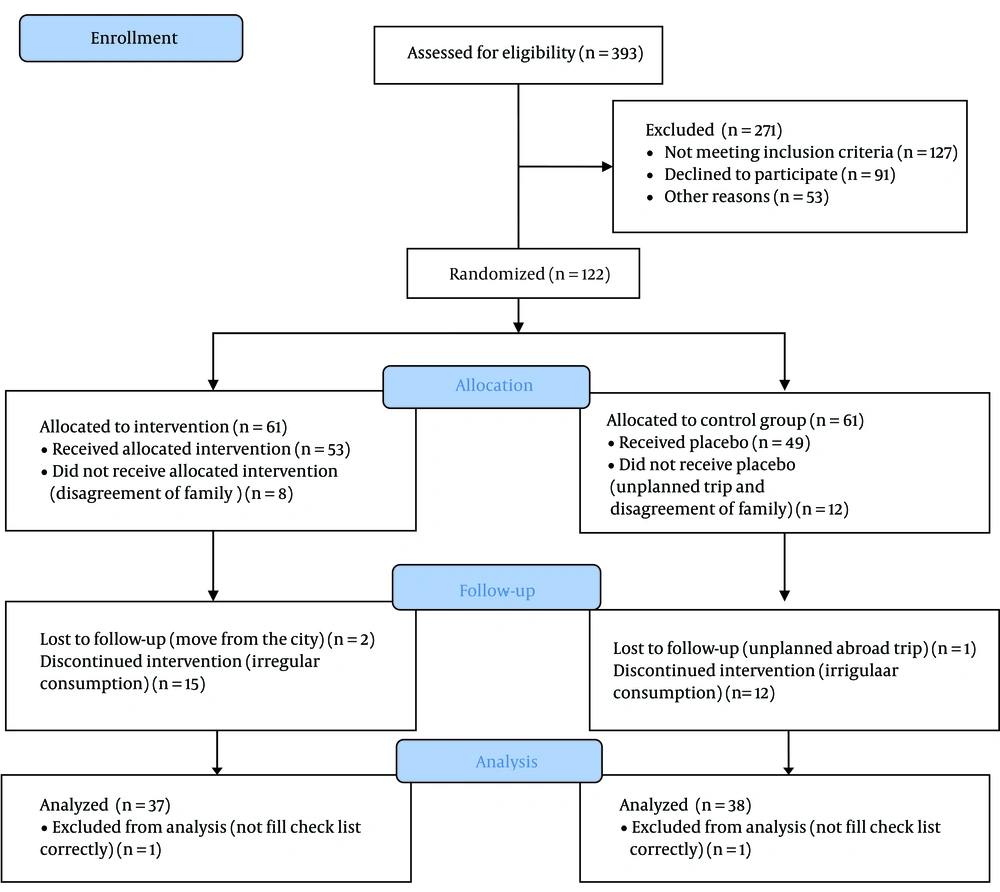
Table 3 shows the severity of hot flashes in both groups. The results of Mann-Whitney U test showed that these differences were significant in the P. anisum group (P = 0.001). Also, during the eight weeks of treatment, four patients in the P. anisum group experienced spotting. There is no harm or unintended effects in any of the groups. The consort chart and diagram are shown Figure 1.
| Groups and Hot Flash Severity | Before the Treatment | After the Treatment | After the Follow-Up Period | P-Value |
|---|---|---|---|---|
| Pimpinella anisum | 0.001 | |||
| Mild | 10 (27.8) | 32 (88.9) | 26 (72.2) | |
| Moderate | 20 (55.5) | 4 (11.1) | 10 (28.8) | |
| Severe | 6 (16.7) | 0 (0) | 0 (0) | |
| Total | 36 (100) | 36 (100) | 36 (100) | |
| Control | NS | |||
| Mild | 7 (19.4) | 8 (22.2) | 10 (27.8) | |
| Moderate | 25 (69.9) | 23 (63.9) | 21 (58.3) | |
| Severe | 4 (11) | 5 (13.9) | 5 (13.9) | |
| Total | 36 (100) | 36 (100) | 36 (100) |
Comparing the Severity of Hot Flashes in the Two Groups Before the Treatment, During the Treatment, and After the Follow-Up Period Based on the Pain Ruler Scale a
5. Discussion
According to the results of this study, P. anisum reduced the frequency and severity of hot flashes. Also, due to the effects of its phytoestrogens and the herbal medicine, it prevented the recurrence after four weeks of discontinuing the medication. Several studies on the effect of phytoestrogenic plants, like licorice have shown that these herbs had alleviating effects on heart diseases, breast and endometrial cancers, and osteoporosis, and they relieved menopausal symptoms, especially hot flashes (18-21), and improved memory and sleep patterns (24). Nahidi et al. reported the efficacy of P. anisum in reducing the frequency and severity of hot flashes among women in Ghazvin, Iran (20, 21). One of the strong points of the present study was the duration of treatment (eight weeks), which was twice the duration of the study by Nahidi et al. We also observed the frequency and severity of hot flashes declined until two weeks after discontinuing the medication, which indicates how long the medication can be effective. Nahidi et al. reported the same results (18, 20).
In another study, Nahidi et al. also reported the phytoestrogenic effect of licorice in reducing frequency and severity of hot flashes (18, 19). Mirabi and Mojab studied the effect of valerian on hot flashes, and the results showed a significant difference in the pre-and post-valerian treatment phases (24). In a study by Ye et al., a daily supplement of 84 or 126 mg soybean isoflavones improved menopausal symptoms (25). Heyerick et al. cited in Aghamiri et al. studied the effect of phytoestrogenic plant hop on hot flashes; their results were in line with ours (26). A relevant systematic review and meta-analysis on isoflavones clarified the effect of soybean isoflavones on the frequency and severity of hot flashes (27).
The results of the present study on reducing the frequency and severity of hot flashes were similar to the results of Farzaneh et al., who investigated the efficacy of evening primrose with placebo in improvement of menopausal hot flashes in 56 menopausal women. On the other hand, percentage of improvement in social activities, relations with others, and sexuality was significantly superior to placebo group (28). Also, Ahsan and Mallick showed the efficacy of soy isoflavones on reducing the frequency and severity of hot flashes, which was in line with the results of the present study (29). However, Van Patten et al. did not find phytoestrogen soy to be effective on reducing the daily frequency of hot flashes in Canadian menopausal women with breast cancer (30). The results can be explained by the fact that cancer is stressful and aggravates hot flashes, and breast cancer can affect mental health and cause anxiety.
Most participants of the present study were suffering from moderate hot flashes while after the treatment and during the follow-up period, most of them had light hot flashes, and no severe hot flashes were reported. The same results were reported by Nahidi et al. investigating the effectiveness of licorice and P. anisum (18-21). Meanwhile, in the study by Taku et al., most postmenopausal women suffered from severe hot flashes before the treatment, while most of them had mild hot flashes, and some experienced severe hot flashes after the treatment (27).
A strength of our study is that we investigated the possibility of side effects and the lasting effects of P. anisum after discontinuing the medication in the four-week follow-up period. The results showed that the reduction in frequency and severity of hot flashes was significantly different between four-week follow-up period and before starting the treatment, and that the medication remained stable over these four weeks.
It should be mentioned that four samples reported spotting, all in P. anisum group, which might be associated with phytoestrogenic effect of P. anisum on endometrial wall. So, the causes of spotting were evaluated, and since there was no structural disorder, the dosage of P. anisum was reduced.
In our study, no side effects were reported, and most of the participants expressed their satisfaction with reduction of pain and burning during intercourse, which might be due to P. anisum phytoestrogens. We precisely evaluated and closely controlled foods containing phytoestrogens that could affect P. anisum effectiveness during the treatment and in the follow-up weeks. We also excluded the patients who had consumed phytoestrogen-rich foods for three consecutive days. The main limitation of this study was that we did not assess sterogen serum level of participants at the beginning and end of the survey.
5.1. Conclusions
Pimpinella anisum is an effective herbal medicine on reducing the severity and frequency of hot flashes, and it is a simple, non-invasive, safe, and effective treatment for postmenopausal women. Hence, it is recommended to prescribe this medicine in different forms and inform postmenopausal women about different treatments and their advantages and side effects so that they can freely choose the type of therapy.