1. Introduction
Plasma cell leukemia (PCL) is a rare and clinically aggressive form of plasma cell dyscrasia with a dismal prognosis and distinct presentation of multiple myeloma. PCL accounts for approximately 0.6-4% of numerous myeloma cases. PCL is characterized by a peripheral plasmacytosis (> 20% of plasma cells in differential white blood cell (WBC) count and absolute plasma cell count greater than 2.0 × 109/L) (1, 2). As PCL does not harbor a unifying genetic mutation and, consequently, specific therapeutic targeting of oncogenic mutations (1, 3), it is of a high clinical significance to shed light on the detailed molecular diagnostics early in the disease to find potentially targetable agents and design novel therapeutic approaches.
BRAF gene mutations are known as a targetable mutations in different malignancies. BRAF mutations have been frequently detected in melanoma and thyroid and colorectal cancers. BRAF V600E is a point mutation, which leads to activating the RAS-RAF-MEK-ERK signaling pathway in a constitutive manner and independent of extracellular signals (4).
This mutation is a key event in the molecular pathogenesis of hairy cell leukemia (HCL), and nearly > 97% of investigated HCL patients carry this mutation.
Despite its significant contribution to plasma cell neoplasms, BRAF mutation has been rarely considered in these cases. Since the frequency of BRAF mutation in these types of neoplasms is not high, and there is no remarkable indication for evaluation of this mutation in plasma cell neoplasms, finding evidence guiding us toward assessing the BRAF mutation could help make the suitable decision for targeted therapy (5).
2. Case Presentation
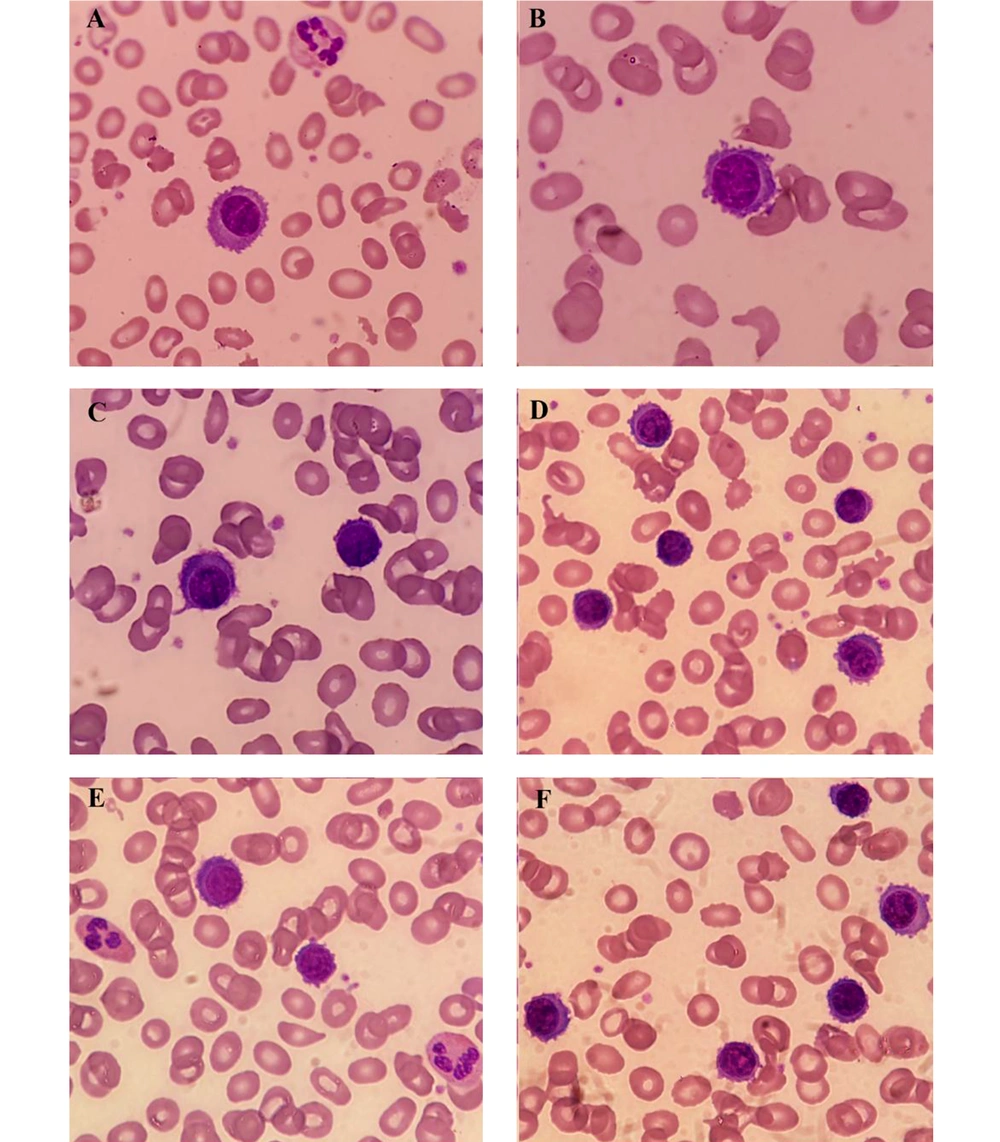
A 79-year-old man presented with fatigue, muscle weakness, and dizziness. Initial hematology evaluation revealed a moderate leukocytosis (WBC: 26.3 × 109/L), anemia (Hb: 8.1 g/dL), and platelet count of 225 × 109/L. Peripheral blood smear exhibited marked lymphocytosis (absolute lymphocyte count: 18.14 × 109/L) and infiltration of about 50% abnormal lymphoid cells with slender cell-surface projections and oval-shaped nucleus (Figure 1). These findings raised the provisional diagnosis of HCL or HCL variant (HCL-v). Additionally, since BRAF V600E mutation is known as the genetic hallmark of HCL, to provide a definitive diagnosis, the blood sample was sent for molecular analysis for this mutation as well as immunophenotyping.
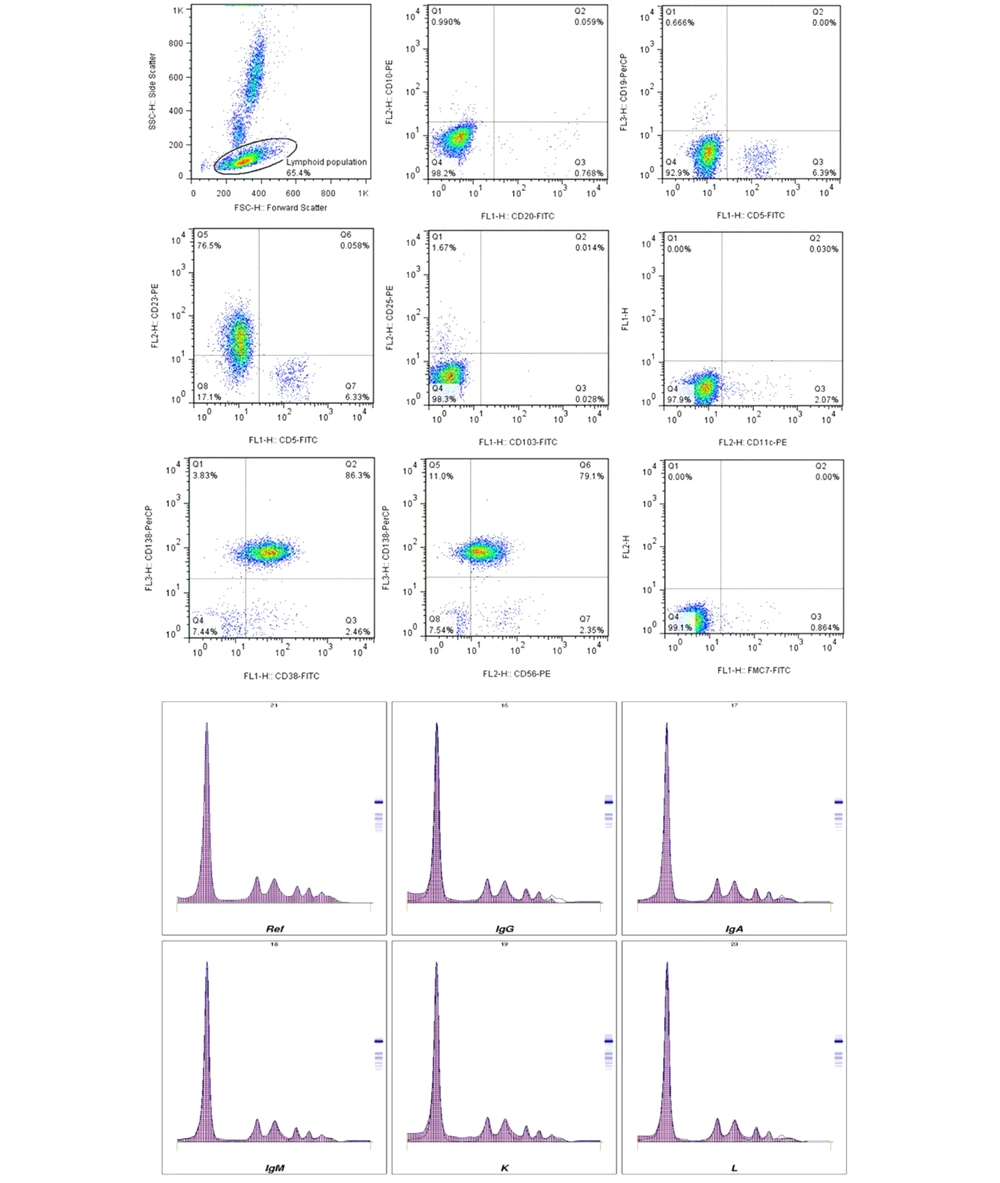
Molecular analysis confirmed the presence of BRAF V600E mutation, which was in agreement with HCL diagnosis, albeit the flow cytometric assessment of abnormal lymphocytes corroborated PCL (CD25-, CD103-, CD11c-, CD45-, CD19-, CD20-, CD56-, CD38+, and CD138+) (Figure 2).
Furthermore, serum protein electrophoresis illustrated moderate hypogammaglobulinemia with a noticeable knob in the gamma zone. According to the immunofixation graphs, the peak was detected to be free lambda light chain (Figure 2). Serum-free light chain assay also revealed elevated levels of lambda-free light chains and a kappa/lambda ratio of approximately 0.036 (normal ratio: 0.26 - 1.65).
3. Discussion
So far, several studies have reported patients with plasma cell dyscrasia described by a hair-like structure; however, none of them evaluated the presence of BRAF mutation in these cases (6, 7). Specifically, there are some reports regarding BRAF V600E mutation in cases with plasma cell dyscrasia, which did not address the morphological changes in detail (4).
There is compelling evidence that cytoplasmic projections in some malignant cells, such as hair-like cells, contribute to BRAF V600E mutation. Under this condition, the constitutive activation of RAS/BRAF/MEK/ERK signaling and the subsequent stimulation of metabolic pathways, such as glycolysis and mitochondrial respiration, are considered to be responsible for particular cytoplasmic changes (8).
In the current entity, the hair-like morphology of abnormal cells prompted us to evaluate BRAF V600E mutation. Our findings were consistent with the previous comprehensive analysis conducted by Rossi et al. (8). This might provide a valuable insight to propose the cytoplasmic projections in plasma cells (PCs) as an indication for the assessment of BRAF V600E mutation in PC dyscrasias, thereby offering helpful targeted therapy through using selective BRAF inhibitors, such as vemurafenib (4).