1. Context
Pandemics are among the severe challenges faced by public health. About nine major pandemics have occurred in the recent century, with at least 59 million deaths (1). The latest occurrence announced by World Health Organization (WHO) in 2019 is the COVID-19 pandemic, which, apart from its physiological impacts on general health similar to other pandemics, has had massive psycho-socio-economic implications for societies. Studies have shown that anxiety and depression have increased by 32 and 33% in the general population during this outbreak (2). Changing the psychological level of different communities arises from some components, such as quarantine, physical distancing, fear of stigmatization, heavy workload in medical settings, etc. (3, 4). The COVID-19 pandemic has also been associated with some other adverse consequences, including the escalation of violence, especially domestic violence targeting women (5), and deterioration of the psychological situation of people with pre-existing mental health conditions (6).
Economic indicators show the extent of pandemic effects. For example, evidence indicates that it affects gross domestic product (GDP), given the critical conditions prevailing in many countries. Several studies and involved organizations have reported a decline in GDP from 2 to 7.2%. Developing countries suffer from a more server GDP decline (7), while the global economy has experienced an average decline of 6.7% in per capita terms in 2020 (8).
The unemployment rate is another indicator that has been affected by drastic changes during the pandemic. Despite the reports of work improvement in many countries in 2019, the stoppage of this trend occurred in 2020 (9). Europe's unemployed youth population has been estimated to increase from 2.8 to 4.8 million in 2020 displaying a general 26% unemployment rate (10). Likewise, according to the International Labour Organization (ILO) report, in 2020, 8.8% of working hours worldwide were lost compared to the winter of 2019, equivalent to 255 million full-time jobs (11).
This significance of the statistics becomes more prominent considering the COVID-19 cases and their related mortality rates. The mortality rate due to COVID-19 has a positive correlation with the unemployment rate while displaying a negative correlation with GDP (12, 13). The association between the COVID-19 situation and socioeconomic indicators resembles a vicious circle.
Another aspect of COVID-19 is the social effects among different communities. This pandemic involves everyone, even though some groups or communities are more vulnerable than others. Generally, people who suffer from inequality and poor access to social resources are more susceptible to health hazards. Current evidence confirms that people with low socioeconomic status have a poor situation about the COVID-19 outbreak. For example, one study from Massachusetts demonstrated that cities with more poverty, lower-income, and the high unemployment rates had a higher rate of COVID-19 (14). Race and ethnicity indicate households' socioeconomic status; according to the UK Biobank data, minorities, such as black and Asian participants were affected by the COVID-19 almost twofold (15). Evidence shows that the black population in the U.S. makes 33% of COVID-19 cases while they are just 18% of the U.S. population (16).
These broad consequences of the COVID-19 pandemic in different aspects of human life escalate inequality. Thus, essential measures and interventions should be designed by health policymakers to manage these effects.
2. Objectives
This study was done to review the main interventions against psychosocial and economic outcomes of the COVID-19 pandemic.
3. Method
3.1. Study Type and Design
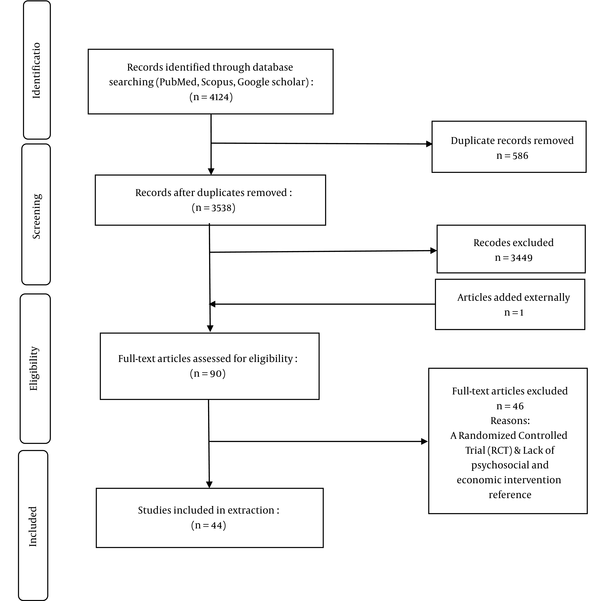
This scoping review aimed to determine the measures taken by governments against different non-medical (economic, social, and psychological) implications of the COVID-19 pandemic. All English papers published between December 2019 and December 2020 were eligible to be included in the study. The inclusion criteria included an intervention that has been taken and not merely a recommendation or suggestion, an intervention by governments or at least with governmental support, economic, social, or psychological interventions, and an intervention exerted in response to the COVID-19 pandemic. All letters to the editor, unofficial reports, or presented abstracts in the conferences, and seminars were excluded. The fellow diagram of the search strategy and screening of the documents is illustrated in Figure 1.
3.2. Search Strategy
To identify the relevant papers, three databases, including PubMed/MEDLINE, Scopus, and Google Scholar, were searched based on the following keywords: Coronavirus OR COVID-19, AND [("economic" OR "economic intervention") OR ("social" OR "social intervention") OR (“Psychological Intervention” OR “mental health intervention” OR “Psychological Support” OR “psychological distress” OR “psychological care” OR “psychological stress” OR “psychological impact.]. Some article references were used to search the grey literature after searching the databases.
Two authors, SA and MF, reviewed the literature from January 2021 to April 2021 independently, according to the above criteria, and selected the related citations. Then, they reviewed the final articles and extracted several components, including the exerted interventions, the intervention area (economic, social, or psychological), the geography of intervention, and the target population. Conflicts between two reviewers were resolved by the third author (HJ). Finally, the results were categorized and presented descriptively.
4. Results
Initially, 4124 citations were searched and inserted into the EndNote. Duplicates were removed, and a total of 3538 titles and abstracts were reviewed. After the completion of the title and abstract screening, 90 full texts were considered potentially relevant and reviewed. Subsequently, 44 citations fulfilled the eligibility criteria and were included (Figure 1).
Regarding the negative psychosocial and economic effects of the COVID-19 pandemic, governments have established measures in these areas to manage some of its burdens. Apart from interventions related to the general population, at-risk and vulnerable groups, such as those with low socioeconomic status, are specific targets of the interventions. According to our findings, three types of the taken supportive-economic measures involve providing compensation for income and revenue losses, reducing payments, and guaranteed measures.
Quarantine and shutting down businesses damage businesses and household income; hence, governments have taken significant measures to compensate for these damages. Some measures include offering cash payments to vulnerable groups, such as workers, financial and nutrition grants, lending, subsidizing and capital injection, and similar aids. Also, other economic actions focus on reducing the amounts that business owners and individuals should pay, such as deferring or suspending taxes and reducing the rate of social security contributions. The third type of action involves quarantine measures to support economically vulnerable groups and individuals by guaranteeing the reimbursement of loans or buying the products. Table 1 shows a more detailed description of these measures.
| Countries | Group | Intervention |
|---|---|---|
| Ireland, New Zealand, Australia, USA, South Korea, Sweden, Japan, UK, Italy, Spain (17); South Africa (18, 19); China (17, 20) Eswatini, Zimbabwe (21) Peru, Kyrgyzstan (22); Portugal (23) Nigeria (24) | General population | Income support measures for household |
| UK, Germany, Italy, China, Hong Kong, Ireland, Australia, Spain, France, Japan (17) South Africa (19) Egypt (25) | General population | Loan and product guarantees |
| South Korea, USA, Australia, Hong Kong, New Zealand, China, Italy, Germany, UK, Japan, France, Sweden, Spain (17); Italy (23) | General population | Adjusting tax policies by deferring or suspending |
| Japan, France, USA, , Ireland, Spain, New Zealand (17); South Africa (19) Spain, Greece, Portugal (23) Nigeria (24); Egypt (25) | General population | Supporting industries and businesses by loans, subsidies, and capital injections |
| Sweden, South Korea (17) Spain, Portugal (23) | General population | Reducing the rate of social security contributions |
| UK, Japan, South Korea, Spain, Sweden (17) | General population | Increasing the loans and capital injection |
| France, Germany, Hong Kong (17) | General population | Employment protection |
| Italy, Germany, Sweden, UK (17) Ghana (26) | General population | Different interventions (subsidies welfare support, covering the rental reduction, Direct grants, deferral of debt payments, and paying electricity bills) |
| Italy, Germany (17), Nigeria, Kenya (18), China (40), Greece, Portugal (23), Egypt (25), Bangladesh (27) | Low socioeconomic people | Supporting workers (covering the lost hours of short-time workers, cash payment to workers, and supporting workers by loans or guaranteeing loans) |
| African countries (28) | General population | Interventions in the energy sector (free electricity provision, reduction of electricity costs, suspension of bill payments, support for oil and gas, tax exemption on energy bills, incentives for renewable, etc.) |
| China (20) | General population | Supporting different insurances and special unemployment insurance |
| Sweden (18) | General population | Supporting students |
Economic Interventions During COVID-19 All Around the World
Rather than the economic interventions, some literature mentioned social support by governments for different groups. Generally, at-risk and vulnerable groups are the target population in governments' social support measures and some not-for-profit and non-governmental organizations (NGO). The following measures can be mentioned in the social area: (1) supporting domestic violence victims; (2) providing shelters and nutrition for refugees and the homeless; and (3) supporting workers, especially migrant workers, and providing the necessary arrangements for the elderly.
Psychological effects are some of the most pervasive undesirable consequences of the COVID-19 epidemic; thus, governments and some NGOs intervene in this area to manage and mitigate these effects. Establishing virtual ways and telecommunication is the main approach in confronting to psychological effects of the epidemic condition. Virtual platforms have been used to educate the general population and high-risk groups to confront stress and anxiety resulting from corona conditions. Video conferences, individual interviews by virtual networking platforms, and exchanging text and video messages are some examples of psychological interventions for increasing social connections against physical distancing. COVID-19 cases, patients with a history of psychological disorders, and older adults as high-risk groups have received special attention through the interventions and actions. Details about social and psychological interventions are illustrated in Table 2.
| Country | Group | Intervention |
|---|---|---|
| UK (18); France (29); U.S. (30) | At-risk population (domestic violence Victims, HIV+ patients, Children, Patients with chronic diseases, Elderly, pregnant women, and prisoners) | Supporting domestic violence victims (providing guidelines, determining the place and phone number for referral, granting funds to organizations for preventing, and responding to domestic violence victims) |
| Ghana (26) | At-risk population | Supporting elderly (provision of foodstuffs and meals, educating about COVID-19 and its preventive measures, learning how to use social media, supporting by insurance, allocating special funds by the government, and providing social support by NGOs) |
| Sweden, Lebanon (18) | People with Low socioeconomic status | Supporting refugees (Providing shelters and Providing foods and personal protection equipment) |
| IRAN (31); U.S. (32) | At-risk population | Supporting prisoners (releasing 70000 prisoners to reduce in-custody transmission and intersectional efforts to reduce prisoner’s population in COVID-19era) |
| Bangladesh (27); Kuwait (33) | People with Low socioeconomic status | Supporting migrant workers (free access to testing and treatment for COVID-19, providing information on COVID-19, covering basic necessities by community volunteers, charity organizations, donors, and non-profit organizations, mutual agreement between the government and employers to continue paying, Increasing diplomatic activity to support migrant workers) |
| U.S. (34) | People with low socioeconomic status (Hispanic) | Providing digital content to guide Latino about COVID-19 and decrease inequalities |
| U.S. (35) | People with Low socioeconomic status | supporting COVID-19 positive cases in low-income families through the "Test-to-Care" project (remote clinical care, providing essential information, and provision of food and sanitation items) |
| U.S. (36-38) | General population | Organized Telepsychology support through social media platforms (texting and video calls) to Engage the patients in self-care behaviors, such as getting recommended sleep and exercise |
| At-risk population | Virtual communication platforms to engage women in self-care behaviors (e.g., adequate sleep, physical activity, and healthy eating), and their partners to have emotional support, being outdoors, gratitude, and adhering to structures and routines. | |
| India (39) | People with Low socioeconomic status | Provision of foods for vulnerable groups (poor households, migrants, homeless, etc.) |
| Spain (23) | People with Low socioeconomic status | ban on cutting water, energy, or gas supplies to vulnerable consumers |
| Canada (40) | People with low socioeconomic status | converting local schools or community centers into temporary shelters and providing hotels for homeless people |
| Canada (41, 42) | General population | text messaging service to encourage people for self-reported stress, anxiety, depression, and contamination/hand hygiene obsessive-compulsive symptoms & Use of Asynchronous Virtual Mental Health (AVMH) Resources |
| At-risk population | Intervention Network COVID-19 Home-isolation Activities Together (SPIN-CHAT) text messaging (Text4Hope-Cancer Care) as a convenient, cost-effective, and accessible population-level mental health intervention; A virtual neurologic examination (VNE) for Mental Status Examination and Cognitive Testing | |
| Pakistan (43) | General population | Providing various activities that people can undertake for a healthy lifestyle, like sports, yoga, music, arts, and mindfulness through the mental health telemedicine helpline & social media platforms, such as Facebook and YouTube; Establishment Tele-clinics called the mental health telemedicine helpline to deliver mental health service |
| Tunisia (44); India (45); Australia (46, 47) | General population | Online Mental Health Services, helpline, Text messaging, chat, telephone, and videoconferencing |
| Spain (48) | At-risk population | Using the city’s municipal shelter, covering lodging and maintenance necessities as a consequence of the reduction in the capacity of the pre-existing resources |
| China (49-54) | General population | Using social media platforms, such as Facebook or Snap-chat to reduce stress and anxiety; Psychological assistance hotline team to offer guidance and supervision to callers to help |
| At-risk population | Encouraging patients to express feelings; Expressing patients’ understanding and comfort; Giving knowledge and information about COVID; Providing some simple relaxation techniques, and offering the self-emotional management skills (such as listening to music as a way of distraction when in a bad mood) | |
| Ireland (55) | At-risk population | Holding online therapeutic triad CBT sessions amongst children with mental disorders and their parents |
| Italy (56, 57) | General population | Virtual acceptance and commitment-based therapy (ACT) to promote psychological flexibility and mental health |
| At-risk population | Access to personal health records from the hospital in a remote fashion (smart-working) | |
| Germany (58, 59) | General population | Coping with Corona: Extended Psychosomatic care in Essen' (CoPE) is. an online training program using psychotherapeutic techniques of mindfulness and CBT |
| Portuguese (60); South Korea (61); Hungary (62) | General population | A telephone-based intervention to promote cognitive-emotional regulation and emotional stabilization, allowing a better acceptance of the experience and more efficient use of personal resources |
| Malaysia (63) | General population | An online Ultra Brief Psychological Interventions (UBPI), including empathy, mindfulness, emotional regulation, and problem-solving skills |
Psychosocial Interventions During COVID-19 All Around the World
5. Discussion
The literature review involved interventions exerted in non-medical consequences of the COVID-19 pandemic. Since the effects of this pandemic are not limited to the medical sector, governments have taken different measures to manage other effects. These interventions, in this review, are discussed into three categories, including economic, social, and psychological measures.
5.1. Economic Interventions
Economic interventions mainly focus on the general population, targeting the impoverished households by cash payment, loan guarantee, deferring and suspending taxes, increasing loan injection, covering the rental reduction, and suspension of bill payment. Also, many interventions intend to support industries and businesses, including product guarantees, adjusting tax policies, loans, subsidies, and capital injection, reducing the rate of social security contribution, and employment protections. Among countries that have addressed the economic interventions are 19 high-income countries, six upper-middle-income countries, and eleven lower-middle-income countries (64). Therefore, more financial resources provide a better ground for implementing economic measures in wealthier countries.
5.2. Social Supports
Unlike economic interventions, social supports are mostly allocated to vulnerable, low-income, and at-risk groups. In this review, in the social areas, governments try to protect vulnerable groups against infection by preparing appropriate shelters or providing personal protective equipment and hygiene supplies. In addition, measures also target people affected by the negative consequences of the pandemic are supported, including victims of domestic violence, elderlies, refugees, prisoners, migrants, low-income households, and other susceptible minorities.
Although the COVID-19 epidemic affects all people and their lives, some groups are at greater risk, such as low socioeconomic groups, workers, refugees, migrants, homeless, minorities. In fact, COVID-19 cases and their mortality rates are higher in socially vulnerable groups than in the general population (65, 66). Therefore, social support is necessary to control the epidemic and protect these groups from the undesirable effects of the disease. Considering the limited capacity of health care systems in low- and middle-income countries compared to high incomes, their governments should pay more attention to social interventions (67).
5.3. Psychological Interventions
Unlike previous pandemics of other coronaviruses, improving E-health infrastructure, virtual platforms, and telemedicine have resulted in on-time and effective psychological interventions amongst the affected populations (68). For instance, in Essen, Germany, using the "CoPE" program mental health services were delivered to people affected by COVID-19 via telephone, video conferencing calls with the experts, or online interventions. This program consists of several modules: psycho-education, mindfulness, and cognitive behavioral skills training (58). Thus, in most countries, psychological interventions, including cognitive behavioral therapy (CBT), acceptance and commitment-based therapy (ACT), and mindfulness-based stress reduction interventions have been delivered remotely (online) through various electronic media, such as Wechat, telephone, and Internet, or psychological and educational videos (55-57).
Evidence indicates that in countries, such as China, United Kingdom, and South Korea, psychological interventions for the general public are based on resilience, flexibility, and emotional regulation in epidemic situations (69-71). Some artificial intelligence (AI) technologies have also been used in the form of face-to-face psychological interventions. In Canada, for example, SPIN-CHAT is a group videoconference intervention program based on anxiety management principles for maintaining the mental health of scleroderma patients and cancer patients in the COVID-19 era (41).
Although developed and developing countries have been similarly affected by mental health outcomes of COVID-19, the highest number and the most pervasive non-medical interventions have been conducted in high-income countries (72). For example, in countries, such as the United Kingdom (55), United States (73, 74), and Australia (46, 47, 75), the telemedicine revolution and telepsychology have been used during the psychological crisis for public health emergencies (74). Evidently, limited financial resources, low access to comprehensive health care, especially in rural areas, and socio-cultural factors are the main obstacles in LMICs to act on psychosocial and economic interventions (76).
This scoping review collected practical information about the implemented interventions to reduce the burden of COVID-19 psychosocial and economic consequences. However, only English documents were reviewed, and only three scientific search engines were used. Thus, many implemented interventions may not have been published yet to be included in the present paper.
5.4. Conclusions
The future of the COVID-19 pandemic is vague and unpredictable. Governments and their decisions will determine the trend the pandemic will take. Therefore, governments, especially in LMICs, are responsible for supporting vulnerable people and protecting them against the devastating socioeconomic and psychological implications using their capacities and resources.
In addition, psychosocial risk assessment and a comprehensive risk management plan are required to combat short- and long-term outcomes of the COVID-19 pandemic on public health to assist in ensuring general mental health and timely psychosocial response.