1. Background
According to the World Health Organization (WHO), sexual health is the interaction between the mind, body, and emotions that improve personal desires, communication, and love (1). Sexual function is a process that involves various organs of the body, such as the neurological, vascular, and endocrine systems. Women's sexual function refers to a woman's ability to achieve sexual arousal, lubrication, orgasm, and finally, a sense of satisfaction (2). Comprehensively, sexual function is one of the most important areas of health, quality of life, and general health that affects humans from birth to death (3). Various hormonal changes, including menstruation, pregnancy, childbirth, breastfeeding, and menopause, can affect people's sexual function (4). Pregnancy and childbirth are challenging periods for a couple that can affect sexual health (5, 6). Although there may be a wide range of individual changes and swing patterns, sexual activity decreases during pregnancy (7). In addition, the postpartum period is associated with urinary incontinence, depression, fatigue, perineal pain, and changes in sexual activity (8). Childbirth results in anatomical and functional changes in the pelvic floor muscles, which leads to sexual problems in many women in the postpartum period (9). Other changes, such as decreased libido, vaginal dryness, dyspareunia, and anorgasmia, can also affect the sexual cycle (10). A common sexual disorder is dyspareunia during the first year after delivery, and its amount increases significantly after delivery (11, 12). Dyspareunia is persistent or recurrent pain in the genital system before, during, or after sexual intercourse (13). This affects not only physiological health but also has many mental and physical consequences, of which undesirable emotional influence between couples and psychological and association distress are significant (14). Many factors, like the type of delivery, lactation, dyspareunia before pregnancy and during it, and resumption of sexual activity in the postpartum affect postpartum dyspareunia (15).
The prevalence of dyspareunia and other postpartum sexual problems is more true in women who have had a vaginal delivery (16). Several studies have shown that dyspareunia during 3 - 6 months after vaginal delivery is more common than cesarean delivery because of trauma to the pelvis after vaginal delivery (12). Descending fetal head and perineal stretching can cause direct neuromuscular and tissue injury in vaginal delivery (17). Numerous factors, such as grade 3 and 4 perineal ruptures, episiotomy, instrumental deliveries, for example, forceps and vacuum, and infant weight over 4 kg lead to dyspareunia after vaginal delivery (12, 18).
Therefore, one of the reasons for choosing cesarean delivery by women and specialists can be perineal injury and subsequent dyspareunia (19).
2. Objectives
According to the importance of postpartum sexual dysfunctions and their many effects on the quality of life of couples, this study aimed to determine vaginal postpartum sexual function and dyspareunia.
3. Methods
3.1. Participants, Recruitment Setting, and Sampling Procedure
This descriptive-analytical study was performed using a cross-sectional approach on 400 women with a history of natural childbirth from August 2020 to February 2021 in Hormozgan Province, Iran. The sample size was obtained with a 95% confidence interval, 5% error, 36% P (20), and 10% drop. The Ethics Committee approved this study of Hormozgan University of Medical Sciences, and sampling began after getting the necessary permissions from the university authorities. The random multi-stage sampling method was done. Firstly, to select the sampling site, the health centers of Hormozgan Province were divided into four regions of north, south, east, west, and three health centers were randomly selected from each region. Then, the sample size inside each health center was determined by structural equation modeling and the population covered. Finally, sampling was done in available health centers.
Inclusion criteria were Iranian women aged 18 to 45 years who were literate, passing of three months after vaginal delivery, beginning intercourse in the postpartum period and also, receiving prenatal care, no stressful event during pregnancy (leaving a spouse or divorce, the death or ailment of a relative, an accident, and home burglary), and no complications, such as difficult delivery (dystocia), postpartum hemorrhage, and postpartum depression during recent pregnancy. According to their report, the samples had no history of chronic disease and known mental illness and a history of taking drugs that affect sexual function, such as antidepressants, such as SSRIs. They did not use hormonal contraceptives, and their spouses were able to have normal sex (for example, they did not have erectile dysfunction or premature ejaculation). Exclusion criteria included women who did not consent to complete the questionnaire. All eligible participants signed a written consent form approved by the Hormozgan University of Medical Sciences Ethics Committee without any compulsion.
3.2. Measure
In the present study, demographic and obstetric checklist measuring sexual function and the postpartum dyspareunia questionnaires (Carol Scale) were used.
3.3. Demographic and Sexual Variables
Demographic Information Questionnaire was a researcher-made questionnaire that includes items, such as age, age of spouse, duration of marriage, level of education, number of pregnancies (gravida), the average number of intercourse (per month), and marital satisfaction. Marital satisfaction is the mediator variable measured by the researcher-made questionnaire. This questionnaire had four questions answered on a 3-point Likert scale (1 = low to 3 = high), and the minimum and maximum scores were 4 and 12, respectively. The face validity of marital satisfaction was done using the opinions of 15 women who were referred to the health clinics and were asked to comment on appropriateness, clarity, and potential ambiguity of the items explored, and logical sequence of items to achieve the qualitative face validity assessment and regarding face validity, the results showed that all items of the scale were appropriate, clear, and straightforward to use. The content validity of the marital satisfaction questionnaire was performed using the opinions of ten experts in the area of sexual and reproductive health. The CVI results of all items were above 0.79, which were considered appropriate and did not need to be reconsidered in the final version (CVI-1 = 0.85, CVI-2 = 1, CVI-3 = 0.95, and CVI-4 = 0. 95). Also, the CVR of marital satisfaction questionnaire’s items was higher than the minimum value of 0.62 (according to the assessment of 10 experts) in Lawshe's table. In the present study, to evaluate the reliability, Cronbach's alpha coefficient was 0.861.
3.4. The Carol Postpartum Sexual Function and Dyspareunia Assessment Scale
In 2017, Lopez-Lapeyrere et al. designed a new tool for measuring postpartum sexual function and dyspareunia among Spanish women. This tool has 11 questions, including four factors about pain and discomfort related to vaginal penetration, vaginal stimulation, after vaginal intercourse, and preparation for sexual activity. Two sections assess the frequency of sexual problems and the severity of pain or inconvenience. A 5-point Likert scale was used to answer questions to assess the frequency of sexual problems from "never = 0" to "always = 4," and the scale for assessing the severity of pain or discomfort was based on the pain ruler between 0 (no pain) and 10 (maximum pain intensity) (21). The validity and reliability of the Persian version of this instrument were confirmed by Banaei et al. in 2020. The structural factor analysis was performed using confirmatory factor analysis. The Persian version of the carol postpartum sexual function and dyspareunia assessment scale has four factors of the original tool were confirmed. The fit of the four-factor model was confirmed ideal based on goodness of fit indices. The average variance extracted (AVE) value of all factors was 0.772, 0.660, 0.552, and 0.664, respectively, which is higher than 0.5 and indicates acceptable convergent validity. The overall Cronbach's alpha coefficient of the instrument to show internal stability and the total ICC to indicate the stability or repeatability of the scale throughout the time were 0.892 and 0.793, respectively, and also the reliability was considered acceptable (22). In the present study, to evaluate the reliability, Cronbach's alpha coefficient of factors one to four was 0.823, 0.830, 0.852, and 0.786, respectively.
3.5. Statistical Analysis
This research was done using the correlation method and structural equation modeling method. Sexual function and dyspareunia after vaginal delivery as response variables, age, spouse's age, length of the marriage, education level, number of pregnancies (gravida), and average number of intercourses (per month) as independent variables, and marital satisfaction as a mediator variable were considered.
For preliminary data analysis, SPSS 18.0 Software and for PLS modeling, Smart PLS Software was used. To analyze the data, descriptive and inferential statistical methods were used. Descriptive statistics, including mean and standard deviation were determined. In the inferential statistic part, the structural equation modeling (PLS method) was used to estimate the coefficients of the β path and also to test the research hypotheses. To evaluate the normality of research data, the Kolmogorov-Smirnov test was used. Because the data of the present study had no normal distribution, the PLS partial least squares method was used to examine the research model. To anticipate sexual satisfaction, the proposed conceptual model was examined through the structural equation modeling method, and the partial least squares method was used to estimate the model. Figure 1 of the tested model shows the association between the research variables (23) (Figure 1).
An initial conceptual model based on Alidost et al. (23)
To show the validity of the research model findings, the structural equation model fit indices using the partial least squares method were used. In addition to the mentioned indicators, the overall pattern fit index in PLS was considered as GOF index, which can be used to check the validity or quality of the PLS pattern in total. This index also acts like the fit indices of the LISREL model and is between zero and one, and mounts are values close to one, indicate the appropriate quality of the model. This index ponders the overall predictive power of the model and if the tested model was successful in predicting latent variables or not.
4. Results
The present study was carried out on 400 women with a history of vaginal delivery. Findings related to demographic and sexual variables are depicted in Table 1. The mean age of the women was 26.74 ± 6.12 years, and on average, they had intercourse eight times a month. The average overall sexual function and postpartum dyspareunia score were 27.18 ± 8.62. The sub-domain scores of preparation for the sexual activity, pain or discomfort on caressing the vulval area, pain or discomfort related to vaginal intercourse, and pain or discomfort after vaginal delivery were 6.97 ± 2.10, 4.10 ± 2.69, 11.87 ± 5.40, and 4.15 ± 2.50, respectively.
| Variables | Mean ± SD / No. (%) |
|---|---|
| Age (y) | |
| 15 - 30 | 296 (74) |
| 31 - 40 | 99 (24.75) |
| 41 and more | 5 (1.25) |
| Spouse age (y) | |
| 15 - 30 | 189 (47.3) |
| 31 - 40 | 184 (46) |
| 41 and more | 27 (6.8) |
| Level of education | |
| Elementary-illiteracy | 29 (7.3) |
| Middle school | 119 (29.7) |
| High school-diploma | 140 (35) |
| College education | 254 (63.5) |
| Duration of marriage (y) | |
| 1 - 5 | 254 (63.5) |
| 5 - 10 | 89 (22.2) |
| 11 - 15 | 48 (12) |
| Up to 16 | 9 (2.3) |
| Gravida | |
| 2 and less | 324 (81) |
| 3 - 5 times | 73 (18.3) |
| Up to 5 | 3 (0.7) |
| Sexual function & dyspareunia | |
| Preparation for the sexual activity | 0.9 ± 4.3 |
| Pain or discomfort on caressing the vulval area | 5.2 ± 2.1 |
| Pain or discomfort related to vaginal intercourse | 4.1 ± 2.2 |
| pain or discomfort after vaginal | 2.1 ± 3.1 |
| Number of sexual intercourse (per month) | 8 (3.4) |
| Marital satisfaction | 6.68 ± 1.97 |
To determine the association between the variables in the model, the correlation coefficient was used (Table 2). The results showed that the association between age, spouse age, the average number of intercourse, and marital satisfaction with sexual function and dyspareunia after vaginal delivery was significant (P = 0.01). While according to the research findings, the variables the duration of marriage and number of pregnancies had no significant association with sexual function and dyspareunia after vaginal delivery (Table 2).
| Variables | Age | Husbands Age | Duration of Marriage | Gravida | number of Sexual Intercourse | Marital Satisfaction | Sexual Function & Dyspareunia |
|---|---|---|---|---|---|---|---|
| Age | 1 | ||||||
| Spouse age | 0.82** | 1 | |||||
| Duration of marriage | 0.67** | 0.62** | 1 | ||||
| Gravida | 0.47** | 0.48** | 0.58** | 1 | |||
| Number of sexual intercourse | 0.29** | 0.32** | 0.17** | 0.39** | 1 | ||
| Marital satisfaction | 0.11* | 0.11* | 0.34** | 0.06 | 0.28** | 1 | |
| Sexual function & dyspareunia | 0.39** | 0.28** | 0.01 | 0.04 | 0.39** | 0.31** | 1 |
ans: P ≥ 0.05; * P < 0.05, ** P < 0.01, two-tailed tests
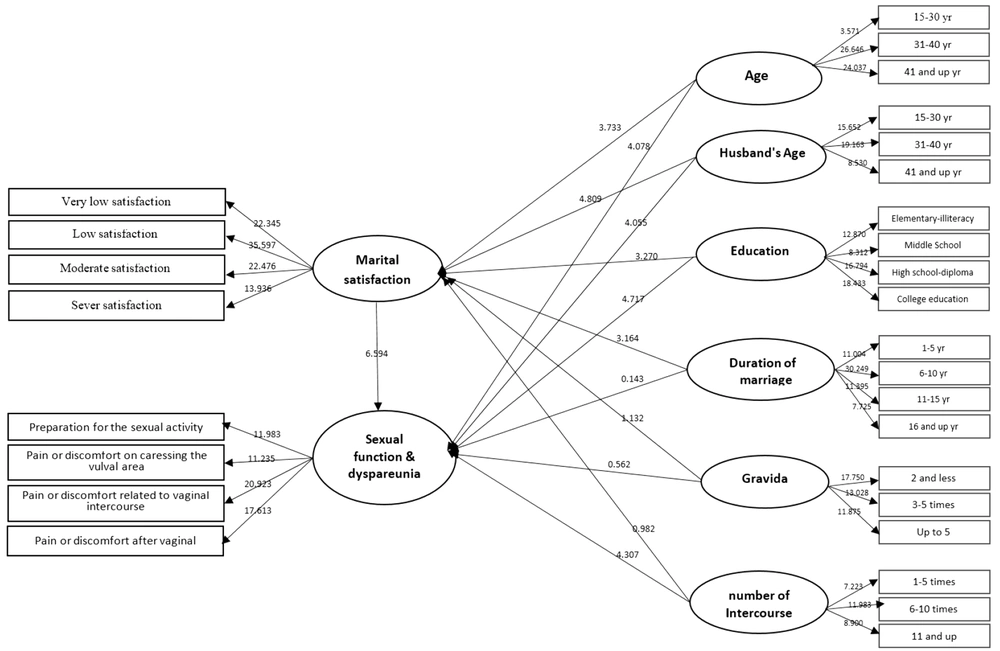
To predict sexual function, the partial least squares method was used to estimate the proposed conceptual model. In Figure 2, the t-statistic for the research paths is reported. The values above ± 1.96 to ± 2.58 are significant at the 0.05 level, and values above ± 2.58 are significant at the 0.01 level. Path coefficients, at the level of 0.01, are positive and significant.
The estimated coefficients and explained variance of variables are shown in Table 3. According to this table, age, spouse age, education, and duration of marriage significantly affected marital satisfaction. However, the impact of the number of pregnancies and intercourse on marital satisfaction was not significant. The findings also showed that the effect of age, spouse age, education, and the average number of coitus on sexual function and dyspareunia after vaginal delivery was significant (P = 0.01), while the variables of the duration of marriage and number of pregnancies had not a significant effect on sexual function and dyspareunia. The findings of structural equation modeling showed that the fitted model explains 0.19 of the variances of marital satisfaction and 0.58 of the variances of sexual function and dyspareunia after vaginal delivery (Table 3).
| Path | Direct Effects | Indirect Effects | Total Effects | Test Statistics | Explained Variance | P-Value |
|---|---|---|---|---|---|---|
| Age → marital satisfaction | 0.32 | - | 0.32 | 3.73 | 0.01 | 0.19 |
| Husbands age → marital satisfaction | 0.41 | - | 0.41 | 4.80 | 0.01 | |
| Education → marital satisfaction | 0.39 | - | 0.39 | 3.27 | 0.01 | |
| Duration of marriage → marital satisfaction | 0.32 | - | 0.32 | 3.16 | 0.01 | |
| Gravida → marital satisfaction | 0.15 | - | 0.15 | 1.13 | 0.192 | |
| Number of sexual intercourse → marital satisfaction | 0.36 | - | 0.36 | 0.98 | 0.109 | |
| Age → sexual function & dyspareunia | 0.54 | 0.17 | 0.71 | 4.07 | 0.01 | 0.58 |
| Husbands age → sexual function & dyspareunia | 0.45 | 0.22 | 0.67 | 4.05 | 0.01 | |
| Education → sexual function & dyspareunia | 0.41 | 0.21 | 0.62 | 4.71 | 0.01 | |
| Duration of marriage → sexual function & dyspareunia | 0.01 | 0.17 | 0.18 | 0.14 | 0.236 | |
| Gravida → sexual function & dyspareunia | 0.04 | 0.08 | 0.12 | 0.56 | 0.218 | |
| Number of sexual intercourse → sexual function & dyspareunia | 0.48 | 0.19 | 0.67 | 4.30 | 0.01 |
Table 4 shows the amount of explained variance, cross-validated communality (CV-communality), and cross-validated redundancy (CV-Redundancy) of the research variables. All amounts of CV-communality seen in Table 4 are positive, which indicates the appropriate and acceptable quality of the present research model. In the present study, for the tested model, the GOF was 0.41, which indicates the appropriate fit of the tested model.
| Variables | CV-Redundancy | CV-Communality |
|---|---|---|
| Age | - | 0.514 |
| Spouse age | - | 0.567 |
| Education | - | 0.601 |
| Duration of marriage | - | 0.524 |
| Gravida | - | 0.536 |
| Number of sexual intercourses | - | 0.541 |
| Marital satisfaction | 0.574 | 0.635 |
| Sexual function & dyspareunia | 0.624 | 0.614 |
5. Discussion
Sexual function during postpartum is one of the most important issues that is always a concern for couples and is influenced by physical, psychological, and genetic factors (24). On the other hand, in addition to physical discomfort, psychological trauma significantly impacts the relationship between couples (25, 26). Also, following the birth of a baby, due to insufficient sleep of the mother, excessive fatigue and mood swings, and changes in the couple's emotional relationship and satisfaction are observed (27).
Due to these issues, the researchers designed the present study aimed at investigating the sexual function and postpartum dyspareunia using structural equation modeling on 400 women who gave birth vaginally in Hormozgan Province. Recently, many studies have been conducted to evaluate sexual function after childbirth (5, 7, 8), but due to uncontrolled interactions with various effects of confounding variables, there is disagreement about the power of the association between physical and psychological factors with sexual function. Hence, because of the importance of the subject, it seems that the present study is one of the first studies to evaluate the hypothesis of the association between physical and psychological factors and their effect on sexual function after vaginal delivery.
In line with the present study's findings, El-Esway & Hanafy results, who assessed 150 Egyptian women one year after delivery, showed that maternal age significantly affects postpartum sexual dysfunction (28). Also, Rezaei et al. found that demographic factors, such as age, education, family income, breastfeeding, and the number of pregnancies, are related to the sexual function of women after childbirth (29). A joint study by Rahmani and Grylka in Iran and Switzerland found that many women did not begin sexual activity three months after giving birth, and cultural differences caused changes in sexual behavior. Awareness of the factors affecting the quality of postpartum sexual life is important, and sex education should be considered in postpartum care (30).
Odar et al. also reported maternal age as the most important factor affecting postpartum sexual function (31). In the study by El-Esway & Hanafy, there was a significant association between sexual function and parity and the number of children (28), which was unlike our study. It seems that one of the important reasons that affect this difference of results is the influence of different cultural factors, such as religion, ethnicity, and race, on diverse dimensions of sexual function in postpartum, which is suggested in future studies to pay special attention to this substantial issue. Culture can be an important factor in postpartum sexual function. In some developing countries, sexual intimacy is prohibited for a long time after childbirth, and in modern countries, due to insufficient postpartum care that causes awareness of couples, sexual intimacy does not exist (32).
Alidost et al. investigated the association between sexual function and prenatal stress and quality of life on 300 pregnant women aged 15 - 45 years and showed that there was no significant association between education level and sexual function (23) that was similar to present study's findings. Also, the results of El-Esway & Hanafy, in this regard, were in line with the results of the two aforementioned studies (28). About the length of the marriage variable, the results of the present study were not consistent with those of Banaei et al., who investigated sexual dysfunction and its related factors in the postpartum on 432 women in Bandar Abbas (20). The results of the present study showed no significant association between the length of the marriage and sexual dysfunction, while in the study by Banaei et al., the highest sexual dysfunction was observed in women who had been married for a short time (20). The reason for this difference can originate from more rooted reasons that should be contemplated about the couple's sexual health. Only increasing the length of the marriage is not enough to have a good relationship. There was a significant association between marital satisfaction and sexual function and postpartum dyspareunia, which is in line with the results of Banaei et al. and Boroumandfar. According to their results, satisfaction with marriage, adjustment, and a better marital relationship by reducing psychological worries will improve sexual function (20, 33). The results indicated a significant association between sexual function and father’s age; no study was found investigating the association between these two variables.
Based on the above-mentioned points, it can be concluded that sexual issues play an important role in marriage and sexual compatibility and also have a great impact on the happiness and satisfaction of couples. The carelessness of sexual issues can have an irreversible effect on interpersonal relationships and the sexual dysfunction and dissatisfaction that can lead to the disintegration of the family (34). It seems that consideration and identification of women's sexual function and effective factors on it, as shown by the results of this study (variables of age, spouse's age, education, the average number of intercourse, and marital satisfaction had a significant association with sexual function) are of great importance. Thus, training couples and health care providers about this leads to promoting sexual function and strengthening the physical and emotional relationship between couples. In the meantime, the importance of encouraging couples to talk about and share their emotional relationship as one of the most effective factors in postpartum sexual function should not be underestimated because it will lead to more closeness of couples and improve their sexual function. Therefore, it is hoped that by using the present study results and similar ones to identify the factors affecting sexual function, by training couples and healthcare providers, sexual relations and emotional performance between couples will be established and strengthened more than before.
5.1. Conclusions
In the present study, age, spouse age, and education had both a direct and an indirect effect on marital satisfaction. However, the number of pregnancies and the average number of intercourses on marital satisfaction were not significant. The findings also showed that the effects of age, spouse age, education, and the average number of intercourses on sexual function and dyspareunia after vaginal delivery were significant at the level of 0.01, whereas the variables of the length of marriage and number of pregnancies had not a significant effect on sexual function and dyspareunia after vaginal delivery.