1. Background
The Iranian economic system is a vulnerable economic system. In the last few years, the word "economic resistance" has entered the economic literature due to the intensification of economic sanctions (1). Economic resistance means the identification of areas under pressure in the conditions of sanctions and then attempts for their control and deactivation ideally to turn pressures into opportunities. Inevitably, this requires the prerequisites for macroeconomic stability, social development, public participation, and rational and thoughtful management (2). In other words, economic resistance is defined as the capacity of the economy to improve or adapt to the effects of exterior shocks undesired (3). Therefore, planning based on economic resistance requires addressing factors that disturb sustainable growth and choosing strategies that minimize risks and uncertainty in achieving goals (4).
In Iran, the general policies of economic resistance with a flexible, making opportunity, and endogenous approach were imparted in 24 paragraphs by the government in 2014 - 18, aiming at dynamic growth, improving the indicators of the economic resistance, and achieving the 20-year goals of the vision policy (5). The economic resistance policies, as a documented system, are supported both legally and theoretically (6). Economic resistance policy packages often have a long-term perspective and are designed to support long-term goals (7).
The health system, as one of the dominant infrastructures of the country, is an economically high-risk context due to its functional, structural, physical, and technological complexity (8). Therefore, health care structures must cope with high-risk situations through increasing flexibility, which means the same goals of economic resistance (5). The implementation of economic resistance policies in the health system can promote the general development of the country, improve the efficiency and effectiveness of the health system, and influence the efficiency of economic management in other sectors of the country (9).
The spread of COVID-19 has affected all aspects of human life worldwide (10) and has disturbed the health systems and economies of millions of people around the world, both directly and indirectly (11). The first and most important effect of this disease is undoubtedly on the global economy is further lowering the economic growth at the international level. From a health economics viewpoint, COVID-19 has similarly affected health systems around the world. In the United States, the pandemic imposed severe financial pressure on its health system despite allocating 20% of GDP to health care in 2020, which is twice the global average cost of health systems (12). In COVID-19 pandemic, hospital revenues have dropped in part due to the low demand for non-emergency surgeries, which can account for 50% of hospital revenues; on the other hand, costs and workload have increased simultaneously to respond to new demands (13). In addition, COVID-19 pandemic has caused many economic crises for insurance companies, incurring financial losses to health care system sponsors and severely affecting the health system infrastructure (14). In the United States, the direct cost burden of COVID-19 treatment was estimated to be between 160 $ and 650 $ billion in the early stages of the epidemic (15). In COVID-19 pandemic, two goals were pursued simultaneously to prioritize health system financing, namely ensuring adequate funding for common health goods and removing financial barriers to access health services. The most important health financing procedures to support these goals include increasing public funding to improve the health system accountability and setting health financing policies to remove financial barriers to accessing health services and care. The first step requires budgeting and mechanisms for public financial management to expand and re-prioritize the budget and financial atmosphere to deal with COVID-19, as well as to establish coordination processes, ensuring the completion and balancing of (internal and donated) funds. The second step is to provide free health services at the site of receiving the service and should, if possible, be considered a complement alongside other strategies such as encouraging home care and telephone counseling (16-18).
2. Objectives
The present study tries to identify the main components of economic resistance in the health system in epidemics such as COVID-19; thereby providing policymakers and authorities of health systems with a better and practical understanding of these components.
3. Methods
The qualitative content analysis method through semi-structured face-to-face interviews was used to determine the components of economic resistance in the Iranian health system. To gather the round views of key informants and experts based on the study objectives, the research population consisted of experts aware of the health system and the concept of economic resistance, including former and current ministers and deputies of the Ministry of Health, former and current chancellors and vice-chancellors of universities of medical sciences, and faculty members of health services management and health economics. Among these, 30 individuals were selected by goal-oriented or purposive sampling using the snowballing method. First, all experts aware of the health system and familiar with the concept of economic resistance who agreed to participate in the study were purposively selected. These people needed to have at least five years of executive and managerial experience at universities of medical sciences or at the Ministry of Health, membership in the headquarters of economic resistance or similar cases at universities of medical sciences or at the Ministry of Health, and to have a research background in the economic resistance theme. The withdrawal conditions of the participants were the unwillingness to participate in the study and unavailability of people due to the far distance or busy schedule to participate in the study. Sampling was continued until achieving the theoretical data saturation and no achievement of a new theme.
Data were collected using a topics guide form containing general questions to clarify the research objectives. The questions were designed by reviewing the literature and using the opinions of expert professors in the field of health policy and health services management in the form of a brainstorming session. A draft version was prepared, and the questions were selected based on the research objectives. To determine the validity and ensure the significance of the questions from the respondents’ viewpoints, interviews were done with two faculty members who were not among the selected interviewees, and necessary corrections were made to complete the questions according to their views. The interview guide included warm-up questions, main questions, sub-questions, and exploratory questions. Table 1 shows demographic characteristics, including gender, age, marital status, level of education, academic degree, managerial background, and the interviewees’ work area related to economic resistance.
| Variables | No. (%) |
|---|---|
| Gender | |
| Female | 3 (10) |
| Male | 27 (90) |
| Age | |
| 40 - 50 | 12 (40) |
| 51 - 60 | 12 (40) |
| 61 - 70 | 6 (20) |
| Marital status | |
| Married | 30 (100) |
| Single | 0 (0) |
| Level of education | |
| Ph.D. | 17 (57) |
| Medical specialist | 13 (43) |
| Academic degree | |
| Assistant Prof. | 8 (27) |
| Associate Prof. | 13 (43) |
| Full Prof. | 9 (30) |
| Managerial background | |
| 5 - 10 | 6 (20) |
| 11 - 15 | 14 (46) |
| 16 - 20 | 5 (17) |
| 21 - 25 | 5 (17) |
| Related work area | |
| Headquarters of Ministry of Health | 5 (17) |
| Universities of medical sciences | 25 (83) |
Demographic Characteristics of Participants
The pre-arranged timing of the interview sessions was coordinated with the individuals by telephone or in-person. During these arrangements, the individuals were provided with the necessary explanations about the goal of the interviews and were assured about confidentiality of the data and full anonymity of the interviewee. Besides, the participants were allowed to cancel the interview at any time despite the initial agreement. Then, all individuals, who were fully informed and agreed to cooperate, completed and signed written consent forms. To increase the issues related to the accuracy, precision, and confidentiality of the interview content, it was tried to perform interviews in a quiet place away from the bustle of the work environment to avoid disturbing the meeting. In addition, the duration of each interview was between 40 and 55 min depending on the level of interest and tolerance of the interviewees. To avoid possible problems, the whole sessions were recorded through two electronic devices. Data were analyzed simultaneously with data collection so that each recorded file was listened several times immediately after the end of each interview, all textual conversations were typed verbatim, and the primary meaningful units were extracted thereof. A copy of the typewritten interview text was sent to the interviewee via email for member check validation, after which the text data were analyzed in the next stage, where the initial codes were obtained based on the extracted meaning units. Then, these codes were classified and reviewed to obtain the final codes. In addition, the key points of the speeches, facial expressions, and non-verbal signs of interviewees were recorded during the interview to confirm the content of their interviews, and these records were also taken into account during the typewriting of the files.
The interview data were analyzed using the theme analysis method as a combination of inductive and deductive approaches. The six-step Clarke and Braun approach cited in Horntvedt et al., including familiarization with the data, generation of initial codes, searching for themes, forming sub-themes, defining and naming the main themes, and producing the report, was used to analyze the theme (19). The accuracy and validity of the data were examined using the four criteria of Guba and Linkon, namely credibility, transferability, consistency or dependability, and confirmability (20). To do this, the researchers tried to increase the research creditability by long-term participation and adequate interaction with the participants, collection of valid data, and confirmation of data by the participant. The dependability of data was improved through step-by-step repetition, data collection and analysis, and revision by experts. For data transferability, it was tried to provide a detailed description of the research report to evaluate the applicability of the research in other fields using special procedures for coding, analysis of symbols, signs, and other methods in the data analysis stage, which helps ensure the transferability. To increase the confirmability of data, the findings were adjusted in such a way to reflect the voice of the participants and the situation under study. This was done by the peer check method in which the coding and extraction of classes were performed by several experienced people in qualitative research who had no conflicts of interest with the subject. Finally, the texts were analyzed by the manual method.
4. Results
The findings indicated that the categories of economic growth, economic stability, justice, and economic resilience as the four main components were involved in the economic resistance of the health system in COVID-19 pandemic. For the economic growth component, the four sub-components of supporting domestic/national production, empowering the private sector,
improving the competitive environment, and knowledge-based economy were identified as sub-components of creating economic growth. In terms of economic stability, the present data led to
the identification of two sub-components of reducing unemployment and developing employment, and deflation and strengthening people’s purchasing power. On the other hand, two sub-components of social justice and elimination of deprivation were recognized in the justice component, which were among the most important components affecting the economic resistance of the health system. Finally, consumption pattern reform, internal self-reliance of the health system, and endogenous financing were identified in the economic resilience component.
According to Table 2, all components embrace several sub-components that can help strengthen the health system in two categories of restorative and resistive. It is noteworthy that restorative factors are able to play a role in restoring the economic resistance in crises and short-term shocks to the health system and help the resilience, restoration, and maintaining the current status of the health system to overcome critical conditions. Therefore, these factors can be used and implemented to manage and respond to pandemics and epidemics, such as COVID-19 conditions. In contrast, resistive factors can be effective in crises and long-term economic shocks, such as recession, sanctions, etc., which have an indirect, macro, and shocking role in the health system, and should be considered by policymakers and health managers. Obviously, to design intervention strategies for each of these sub-components, the context where it is implemented should be deemed by policymakers.
| Factors (Components) | Sub-themes | Categories | Codes |
|---|---|---|---|
| Economic growth components | Empowering the private sector | Restorative components | Facilitating privatization rules and regulations |
| Motivation for private and charitable investment | |||
| Support for private and supplementary insurances | |||
| Improving health service licensing systems | |||
| Boosting public-private sector cooperation | |||
| Resistive components | Amending privatization rules and regulations | ||
| Establishing and strengthening the services of small and medium health enterprises | |||
| Activation/development of health exchange | |||
| Development of domestic and foreign medical tourism | |||
| Agility of the public sector of the health system | |||
| Supporting the domestic/national production | Restorative components | Supporting local and national entrepreneurs | |
| Promoting the use of Iranian medical products and remedies | |||
| Control of drug and equipment smuggling | |||
| Opening financial credit lines for affected businesses | |||
| Supporting targeted research in the production of domestic goods | |||
| Developing alternative short-term production strategies and providing services in crises | |||
| Resistive components | Boosting per capita health budget | ||
| Reforming the tariff system | |||
| Commercialization of domestic products | |||
| Creating/developing a health capital market | |||
| Establishment/development of domestic industries for drug production (esp. vaccines) and medical equipment | |||
| Development and direction of insurance systems from being patient-centered to service-centered state | |||
| Elucidation of health information systems | |||
| Improvement of competition atmosphere | Restorative components | Encouraging and supporting the activities of small and medium enterprises in the health system | |
| Improving health market monitoring and control practices | |||
| Supporting research and development | |||
| Strengthening the support function of the existing insurance system | |||
| Development of an electronic (software-based) health system | |||
| Resistive components | Development of IT infrastructure (hardware) | ||
| De-monopolization of providing services or production of domestic health goods | |||
| Development and improvement of relations with other sectors of the economy | |||
| Expansion of national and regional cooperation | |||
| Targeted identification and support of scientific elites | |||
| Knowledge-based economy | Restorative components | Improvement of university-industry interaction | |
| Targeted direction and guidance of health system research | |||
| Support for research and development centers | |||
| Improvement of the health education quality | |||
| Creating/developing distance learning systems | |||
| Offering banking facilities to research centers | |||
| Strengthening and developing startups | |||
| Resistive components | Codification and amendment of property rights laws | ||
| Research-based export development | |||
| Development of research-based economy | |||
| Development of telemedicine systems | |||
| Policy-making to support the insurance system of knowledge-based goods and services | |||
| Regulatory decisiveness | |||
| Justice components | Social justice | Restorative components | Elucidation of existing regulations |
| Meritocracy | |||
| Designing tax deferral and installment patterns | |||
| Promotion of professional ethics | |||
| Boosting and monitoring cross-subsidies in insurance systems | |||
| Designing an intelligent basket of goods/health services | |||
| Justice in access to health infrastructure | |||
| Resistive components | Creating and developing continuous service patterns in crises | ||
| Elimination of the informal economy in the health market | |||
| Development of public taxes | |||
| Promotion of social participation in the national health system | |||
| Promotion of the health administrative system | |||
| Expansion of insurance coverage | |||
| Elimination of deprivation | Restorative components | Implementation of an intelligent quota system for goods and services with a focus on the needy | |
| Activation of social charity bodies | |||
| Promotion of health indicators | |||
| Prevention of the overwhelming health system costs | |||
| Creating an optimal budget allocation system | |||
| Protection of the health rights of citizens | |||
| Promotion of support services for the poor | |||
| Resistive components | Prevention of poverty-causing costs of the health system | ||
| Redistribution of revenues | |||
| Sustainable employment of doctors and paramedics in deprived areas | |||
| Proper establishment of the referral system | |||
| Establishment and development of competitive insurance systems | |||
| Planning and construction of health infrastructure based on allocation and distribution models | |||
| Components of health economics stability | Reduction of unemployment/development of employment | Restorative components | Frequent need assessment of the health labor market |
| Support for the cooperative sector | |||
| Activation/development of internet and virtual services | |||
| Modification of the payment system | |||
| Encouraging and supporting the activities of small and medium enterprises in the health system | |||
| Insurance support for the unemployed in crises | |||
| Preparation of protocols on activities of health system employees in crises | |||
| Empowerment of the workforce | |||
| Resistive components | Long-term training and education of the workforce in keeping with the needs of society | ||
| Economic preparation of employment in the health system | |||
| Macro employment policy in the health system | |||
| Development of competency policies at different levels of the health system | |||
| Burnout management | |||
| Improvement of investment security | |||
| Modification of organizational structures | |||
| Insurance support for industries and services of the health system in crises | |||
| Developing sustainable and incentive payment systems | |||
| Deflation and boosting people’s purchasing power | Restorative components | Effective monitoring of drug and equipment prices | |
| Eliminating direct financial communication between the patient and the service provider | |||
| Modification of bank interest rates in the health sector | |||
| Prevention of the overwhelming health system costs | |||
| Continuous monitoring of point-to-point inflation in the health system | |||
| Action against hoarding | |||
| Supply and demand management of alternative and complementary goods/services in health economics | |||
| Effective promotion of public health system costs | |||
| Resistive components | Creating/developing national health accounts | ||
| Insurance support for the health system industries and services in crises | |||
| Upgrading the health financial management system | |||
| Prevention of poverty-causing costs of the health system | |||
| Full establishment of a final service cost mechanism | |||
| Investigation and prediction of long-term inflation trends in the health system | |||
| Economic resilience components | Consumption pattern reform | Restorative components | Support for rational medication program |
| Prevention of induced demand | |||
| Stringent implementation of an operational planning system | |||
| Quality improvement of services | |||
| Development of outpatient services in society | |||
| Continuous monitoring and control of consumables and equipment in the centers | |||
| Periodic modification and revision of drug and medical equipment prices | |||
| Resistive components | Creating/developing strategic purchases of health insurances | ||
| Promotion of the resource efficiency system | |||
| Creating/developing electronic health records | |||
| Proper establishment of a referral system | |||
| Paying more attention to health and prevention | |||
| Improving the human resource development index | |||
| Internal self-reliance of the health system | Restorative components | Management of medicine and equipment imports | |
| Identifying neglected economic resources within the health system | |||
| Boosting passive defense systems | |||
| Development and facilitation of intercommunication in the health system | |||
| Creating and developing risk management programs | |||
| Creating surplus stocks of medicine and equipment throughout the country | |||
| Relocation of financial resources to maintain the existing level of production and provision of health goods and services using financial engineering | |||
| Creating/developing surplus production capacities to take action against crises | |||
| Resistive components | Development of long-term alternative strategies for production and service in crises | ||
| Development of drug safety policies | |||
| Reduction of dependence on foreign production inputs | |||
| Investigation and prediction of long-term consumption patterns in the health system | |||
| Reduction of dependence on government budget | |||
| Training of multi-professional workforce | |||
| Reinforcement and stabilization of the medicine and equipment supply chain | |||
| Paying attention to various and unusual incomes in the health system | |||
| Endogenous financing | Restorative components | Creation and development of new services | |
| Redistribution of revenues in the health system | |||
| Establishment of financial discipline | |||
| Reinforcement of the self-government plan of hospitals | |||
| Codification and development of rules for attracting intra-organizational financial partners | |||
| Resistive components | Discovery of internal markets in the health system | ||
| Modification of the tariff structure | |||
| Establishment/development of a management system for financial crisis | |||
| Establishment/development of exchange and capital markets in the health system |
Components of the Economic Resistance in the Health System During COVID-19 Pandemic
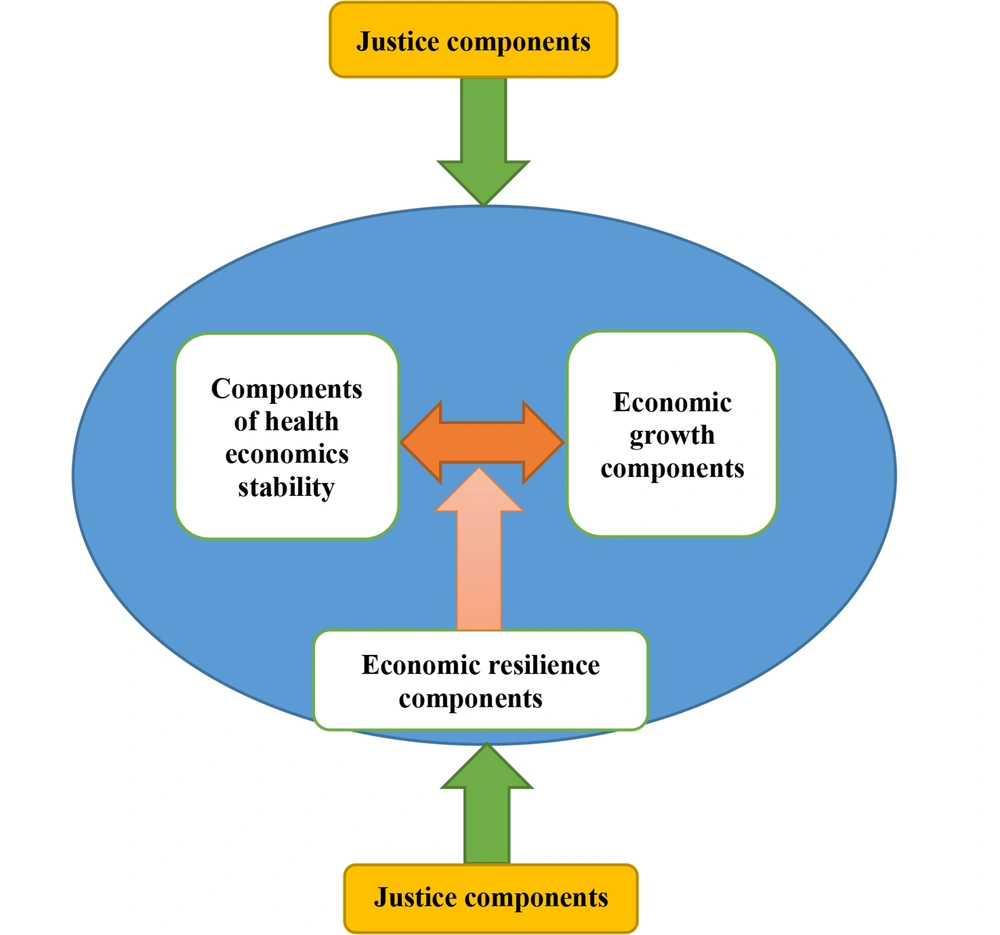
Figure 1 depicts the thematic map resulting from the relationship between the main themes of the study, indicating that the economic growth, economic stability, and economic resilience components have three-way interrelations. In other words, economic stability both as a prerequisite for growth and as a stabilizing factor can affect macroeconomics and the health sector. In addition, economic resilience in short-term or long-term crises can help maintain the status quo and create the coping power with change, shock, or shock to the economy and the health system, alongside the above two components. Finally, the justice component as an internal and external factor can influence the economic components and, as a spectrum, cause the fragility of the health system and reduce its ability to cope with incident crises, thereby causing health problems for vulnerable groups; on the contrary, it can increase the resistive power, integrity, and solidarity of the health system in the face of a crisis in different economic conditions.
5. Discussion
This study aimed to identify the economic resistance components of the Iranian health system in COVID-19 pandemic. Economic growth, justice, health economics stability, and economic resilience were the main identified components. The main goal of economic resistance policies is to develop a model of the local economy based on social values and norms, national resources, and high-quality labor to reduce the vulnerability of the country to external pressures and even to turn threats into opportunities (21). With COVID-19 pandemic, on the other hand, the economies of countries were remarkably affected in various dimensions, among which the health system is one of the aspects that suffered the most damage from this pandemic (22). The health system is one of the areas that require serious attention in the context of economic resistance in COVID-19 pandemic. The Ministry of Health, Treatment, and Medical Education, which is responsible for health in the country, can use its powerful arms and the capacity of organizations and institutions related to the area of health and welfare to achieve the economic resistance in the country in COVID-19 pandemic.
According to the results, the first identified component was economic growth, which is one of the economic resistance principles and is influenced by labor, physical capital, and human capital. In the economic literature, human capital includes education, health, skills, experience, and other capitals that increase labor productivity and contribute to economic growth. Economic resistance policies such as improving the macroeconomic status, achieving the first rank of a knowledge-based economy in the region, improving the share of health, export, and knowledge-based services, and increasing productivity in the health economy, lie at the economic growth axis. Evaluation of health services, referral system, all-encompassing social security, establishing a knowledge-based company, activating the innovation system, and strengthening and empowering factors in health tourism development have been proposed as programs to increase economic growth in the health system (5). Rose considered an economic resistance model to deal with abnormal conditions, a component of which was economic growth (23). According to Butkiewicz and Yanikkaya, developing countries need to limit their government expenditure and stimulate investment in infrastructure for their economic growth (24). According to another study, the growth components of economic resistance are among the national goals of the country, which should be provided because of the challenges in the national economy to fulfill the fundamental goals of the national economy. The economy resistance sub-components include short-term (restorative) and medium-term (improving) policies that can build the necessary long-term capacities to further strengthen the economy to eliminate and deal with shocks to the economy (25).
Some economists believe that the economic impact of COVID-19 pandemic will be greater than that of the 2008 global crisis, even if there is no global recession. Some of the world's economies will either stop or have negative economic growth. This includes some large economies. Thus, not only the coming years will face low growth rates, but also the improvement of the economic growth will take time in the future (26).
COVID-19 reduced global economic growth by 3% in 2020 (27). An effect of COVID-19 on the economic growth of the health system was the increased cost burden of diseases (10). Despite other economic sectors, the health sector has faced a sharp increase in demand for health care throughout the world due to its outstanding presence in action against COVID-19. This increased demand for healthcare services and the high death rate caused by COVID-19 have pressurized healthcare systems, leading to a substantial reduction in economic growth. All healthcare systems have always been facing potentially unlimited demands and actually limited resources. The main goals in all years include the proper allocation of resources, equitable distribution of facilities, and healthcare services. Since the health sector has usually contributed slightly to GDP, funding for this sector has always been supplied from other sectors. Therefore, health financing has also faced a crisis following the incidence of the COVID-19 pandemic (27). Noy et al. presented evidence that the direct costs of COVID-19 with disease and mortality were lower than the indirect costs incurred by this pandemic. Many countries also experience recession even if COVID-19 does not seriously influence their health status (28).
The economic resistance is an effort to enhance the country’s economic strength against internal and external shocks. Although economic pressures and sanctions have been the biggest reason for the implementation of this type of economy in the country, the realization of the economic resistance is becoming more necessary since the outbreak of COVID-19 as an external shock has led to the imposition of restrictions and high costs on economic activities. Therefore, it is possible to take the health economy system of the country out of this external and unforeseen shock at a lower cost and in a short time through the recommendations of the economic resistance to increase the use of the capacity and power of the production system, redesign and reform the distribution system, and change some patterns of the consumption system (29).
Another finding of the study was related to the justice component of economic resistance in COVID-19 pandemic. In a study by Rose, economic justice was a component of the economic resistance model (23). Yousefi and Moosavi Nezhad introduced social justice as a component of economic resistance (25). The equal distribution of opportunities and facilities, with the approach of public availability, in the form of justice in health, was stated as a component of social justice in economic resistance (28). Another study emphasized justice in offering service packages provided by insurance funds to people, paying subsidies to the health sector, and targeted health subsidies aiming at providing justice and promoting health, particularly in deprived areas, and special assistance to the needy and low-income groups as the principles of social justice in economic resistance (30). Ferdosi et al. considered the promotion of social justice indicators in the health sector to be necessary to achieve the goals of economic resistance (5).
COVID-19 should not make us deviate from the realization of social justice. For example, people must adhere to the principles and values of social justice regarding social distancing in the pandemic. Fair distribution of economic benefits and the burden caused by the pandemic is one of the main concerns of social justice among different populations with different levels of economic status and income. Thus, social justice requires the consideration of damages, in particular economic losses, which occurred during COVID-19 pandemic. Governments and communities can provide billions of dollars needed to help many sectors of society, including the health sector, to overcome COVID-19-related economic losses. In this regard, monetary resources should be allocated to implement quarantine and observe social distancing during the pandemic to promote social justice (31).
Another finding of this research was the health economy stability component during the COVID-19 pandemic. Economic stability was a component of the economic resistance model in studies by Rose and Yousefi and Moosavi Nezhad (23, 25). According to Ferdosi et al. economic stability is the interaction between supply and demand in the economy and a component of economic resistance in the health system. Achievement of proper economic stability and boosting the health system against the positive and negative effects of economic shocks are among the priorities of governors in the health system. Familiarity with the needs of health economics, stabilization of health economics, proper use of the real capabilities of the health sector, saving public expenditure, and reforming the government’s revenue system can be utilized in this context (5). Briguglio et al. considered economic stability, microeconomic market efficiency, good governance, and social development as the four main indicators of boosting economic resistance in their study on the concepts and criteria of economic resistance and economic vulnerability (32). Batmanghelidj assessed the vulnerability and status of economic resistance in the Iranian economy and considered economic stability as a critical indicator of economic resistance (33). According to Gondi and Chokshi, financing stability is one of the goals of reforms in the payment system during COVID-19 epidemic, and financing methods, such as prospective population-based, are flexible against such shocks as COVID-19 and support greater access to care if needed (34). In terms of the cost burden, COVID-19 has severely affected the economic stability of the health system. From an economic viewpoint, the spread of COVID-19, the daily increase in the number of patients, and the complications of this disease have imposed high medical costs and indirect costs on patients, the government, and the health system. Although these costs vary depending on the average duration of hospital stay, the disease severity, the average duration of ICU stay, and other factors, the economic burden of direct treatment costs of the disease is worrisome (35).
In this study, economic resilience was the last identified component of economic resistance in COVID-19 pandemic. Resilience is defined as the system’s ability to easily recover from disruptions and changes in the system and the organization’s ability to respond quickly thereto. A resilient system can withstand environmental pressures to have an optimal performance in critical situations (36). The resilience of health systems is also referred to as the readiness capacity to respond effectively to crises, while maintaining the key tasks of the health system before, during, and after the crisis (37). Yousefi and Moosavi Nezhad described economic resilience as a part of the economic resistance model (25). Pilevari and Shiva introduced financing of the health system as one of the dimensions of the health system resilience in COVID-19 pandemic. According to the results of this study, the basic service package of the Iranian health insurance is very extensive, and nearly 90% of the treatment costs of patients with COVID-19 in public sector hospitals were covered by health insurance organizations in the recognition and prevention phase. In addition, the Iranian basic health insurance companies covered some of their uninsured services, such as prescribing CT scans of the lungs by general practitioners and coronavirus diagnostic tests, in the response phase. However, a wide fraction of private hospitals, particularly in metropolitans, still do not have contracts with basic health insurance companies, leading to an increase of patients out-of-pocket in these hospitals. Additionally, home treatment services and health-related goods such as masks, gloves, and disinfectant solutions, are still paid out-of-pocket by the individuals. Financing the Iranian health system will face a financial crisis in the future, even in the event of controlling COVID-19 outbreak. The Iranian health financing system has responded to COVID-19 crisis with insufficient resilience in terms of adaptation and diversity and requires interventions to be improved and strengthened in the response phase (38).
Concerning the resilience of the Iranian medical system in COVID-19 pandemic, the Ministry of Health, as the main reference of the Corona Headquarters, has had an acceptable performance in specialized areas of treatment, control, and preparation of health protocols for prevention and conducting research and tests for diagnosis. In particular, the ministry has had a high potential from the outset for vulnerability assessment, enhancing public awareness of disaster risk assessment and mitigation strategies, and implementation of specialized training programs for managers and health workers. Dimensions of the resilience of Iranian medical system in COVID-19 pandemic include specialization through locating the Ministry of Health at the center of epidemic management, symbolizing through a common understanding of the performance of the medical system against COVID-19, and providing a network of the health system through a wide range of health centers across the country.
The proper placement of this institution at the center of the National Headquarters against Coronavirus is reflected in the design and development of national plans for public health response operations in disasters and emergencies, care instructions, diagnosis, treatment, preparation of prevention and control protocols for specific groups and environments, and national action plan to deal with the outbreak of infectious diseases prepared at the Center for Infectious Diseases Management at the Deputy Minister of the Ministry of Health and Medical Education. However, the success of measures to reduce vulnerability has been dependent on public participation in the implementation of health-centered programs to decrease the risk of the COVID-19 outbreak. This, in turn, requires deeper inter-organizational relationships and community involvement. Other important measures in increasing the resilience capacity of the health and treatment system include symbolizing and establishing common meanings and understandings to ensure effective and coordinated response of the community against the pandemic while controlling its outcomes through social media. Hence, appreciation of doctors, nurses, and all medical staff as advocates of health and symbolizing their unconditional sacrifices, along with the appointment of the Minister of Health as the Head of the National Headquarters against Coronavirus, have led to the high legitimacy of this institution in society for emergency measures. Thus, according to official reports from the government and the Corona Headquarters, the prevalence curve was flat about eight weeks after the virus was identified or entered the country, and the healthcare system in the country was stable, providing an approximately 20% empty capacity to provide services (39).
5.1. Conclusions
In this study, the economic resistance components in the Iranian health system were identified and studied during COVID-19 pandemic. Health systems have always faced epidemic crises in their various dimensions. The Iranian health system, however, has faced many economic challenges during the pandemic, in addition to COVID-19, to deal with and control the disease due to international economic sanctions. The economic resistance strategies seem to be able to help the Iranian health system to represent more resilience against the epidemic crises based on local criteria and to establish justice in its various dimensions, in particular justice in financing for the needy. The economic resistance components can serve as a guide for governors and managers in the health sector to move towards the economic growth of this sector in the post-COVID-19 period and then provide the economic stability of the health system. This study investigates the views of managers and policymakers of the Iranian health system in various fields about the economic resistance components in the health system; thereby providing access to accurate and precise information through the data integration process, which can be a guidance for the action and decision-making of policymakers.