Introduction
The Coronavirus Disease 2019 (COVID-19) pandemic has immensely affected worldwide, giving rise to significant morbidity and mortality (1). Besides age, underlying disease represents a major risk factor for COVID-19 severity, with kidney and liver transplant recipients being highly susceptible to a severe course of the disease despite not being at a greater risk of infection relative to the general population (1-3). In fact, patients with solid organ transplants have a higher rate of mortality (~20%) due to COVID-19 than their non-transplant counterparts (1, 4).
The clinical presentation and outcome of COVID-19 in solid organ transplant recipients vary widely between patient groups and countries (1). Furthermore, limited data are available about the state of such patients (particularly liver transplant recipients) in Iran, with only a small number of cases having been studied (5-7). Therefore, the present study aimed to shed light on the situation of kidney and liver transplant recipients admitted with COVID-19 in Iran.
Methods
We report 30 kidney and liver transplant recipients who were admitted to Abu Ali Sina Organ Transplant Center (the largest transplantation referral center in the Middle East) due to COVID-19 between March 20 and October 20, 2020. All kidney/liver transplant adult recipients who had a positive severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) nasopharyngeal RT-PCR assay and required admission were included. A second SARS-CoV-2 RT-PCR assay was performed in our hospital for further confirmation.
Results and Discussion
In this cross-sectional study of COVID-19 in kidney and liver transplant recipients, 30 adults with a mean age of 52 ± 11.75 years were included. In this population, 76.70% were males and the remaining patients 23.30% were females. The mean Body Mass Index (BMI) was 25.38 ± 3.21 kg/m2. The majority of the patients were kidney transplant recipients (70%), while 30% were liver transplant recipients.
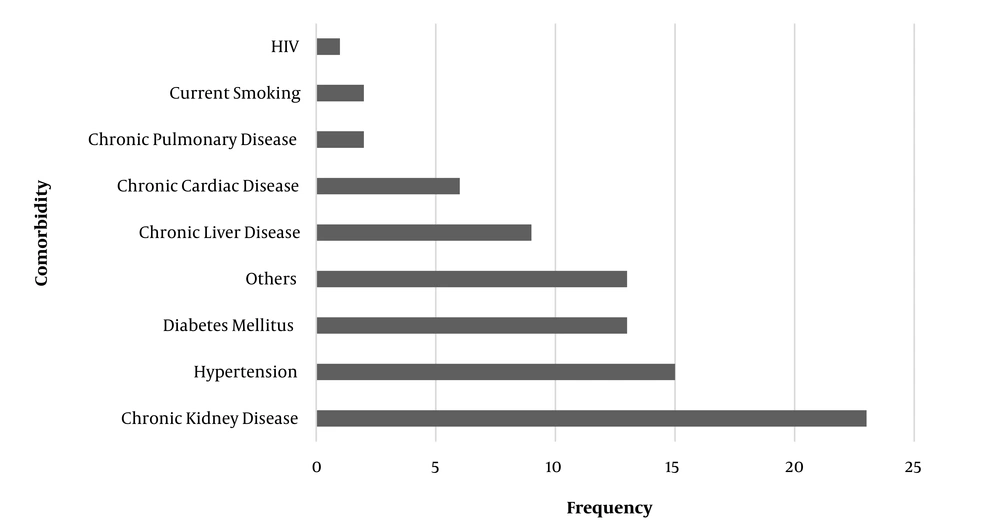
The mean temperature, heart rate, respiratory rate, systolic blood pressure, diastolic blood pressure, oxygen saturation, and Glasgow Coma Scale (GCS) score were 36.94 ± 0.52°C, 92.83 ± 18.95, 18.76 ± 1.85, 129.23 ± 22.19 mmHg, 77.90 ± 18.33 mmHg, 89.60 ± 11.22 %, and 14.80 ± 0.61, respectively. Notably, four patients had prolonged capillary refill times, three of whom were severely dehydrated. Also, 40% of the patients required wheelchair assistance at the time of presentation. The comorbidities of the patients prior to admission are represented in Figure 1.
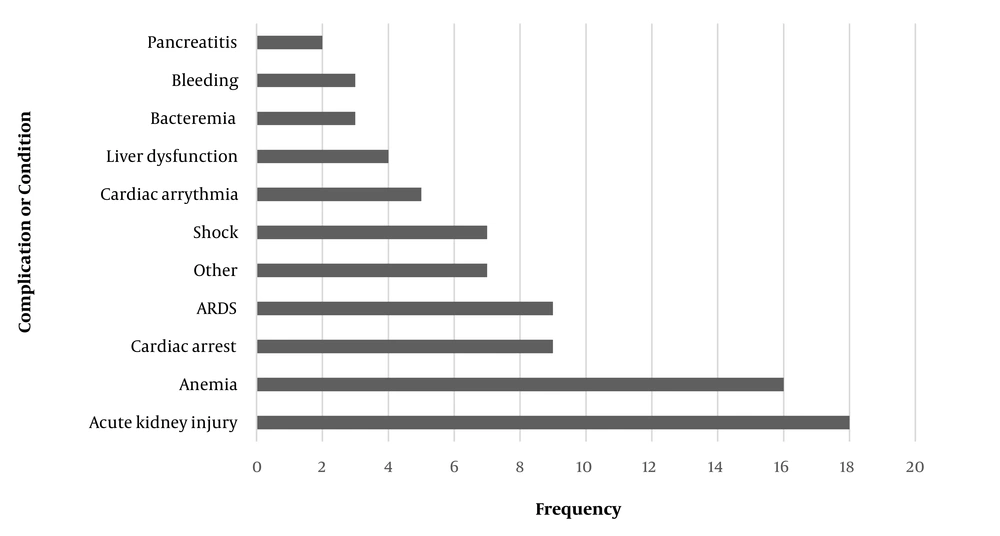
Figure 2 summarizes the frequency of different complications and conditions diagnosed during hospitalization among these patients. Clearly, the most frequent complication was acute kidney injury.
There were nine recorded COVID-19-related deaths in this population during the study period, representing a 30% in-hospital mortality rate. This included six out of 21 (28.6%) kidney transplant patients and three out of nine (33.3%) liver transplant patients. Notably, the majority of these patients experienced acute kidney injury prior to their death, including five of the six in the former group and two of the three in the latter group. The remaining 21 patients were discharged, and complete recovery was recorded for them all at the three-month follow-up.
Among our sample population of solid organ transplant patients, the most prominent signs and symptoms were fatigue and shortness of breath (each 73.3%), followed by fever and headache (each 53.3%), nausea/vomiting (50%), myalgia (43.3%), and cough (40%). Notably, 36.7% of our patients had altered consciousness. Compared with reports on general Chinese and Iranian populations, it seems that our patients had a fairly higher rate of shortness of breath and fatigue, which is probably explained by the underlying condition and highlights a more severe disease course in these patients (8, 9). Among kidney transplant COVID-19 patients, the most frequently reported symptoms are fever (85%), dry cough (70%), myalgia (60%), and dyspnea (57%) (10). Variations may be explained by differences in study populations, with our results being limited to those solid organ transplant recipients that required hospitalization.
Among our study population, the most frequent complication was acute kidney injury, which occurred in 60% of the patients. This is comparable with the reported rate of AKI in the general population of hospitalized COVID-19 patients (56.9%) (11), implying that solid organ transplant recipients are not at a greater risk of AKI than non-transplant recipients. Our result is also comparable with that of the study by Monfared et al., where 12 out of 22 (~55%) kidney transplant recipients with COVID-19 in Rasht, Iran, developed AKI during hospitalization (6). However, a notable finding of our study was that roughly 78% of the liver or kidney transplant recipients who died due to COVID-19 experienced AKI, compared with a rate of 53% among those who recovered. This indicates the necessity of paying greater attention to this complication as a marker associated with fatality.
In Iran, the in-hospital mortality rate of COVID-19 has been reported as 24.4% in a national retrospective cohort study (9). According to the literature, solid organ transplants have a higher rate of mortality (~20%) due to COVID-19 than their non-transplant counterparts (1, 4). This issue was corroborated by our results, where an in-hospital mortality rate of 30% was recorded, comprising 28.6% of kidney transplant patients and 33.3% of liver transplant patients. This is in line with a mortality rate of 27.27% reported in a similar Iranian study, involving 22 kidney transplant recipients hospitalized due to COVID-19 (6), and is also comparable with the rate of 29.2% reported among kidney transplant patients in Scotland (12). The slightly higher mortality rate in the Iranian studies relative to some research from other countries involving solid organ transplant recipients with COVID-19 may be explained by differences in healthcare systems. Our relatively high rate of mortality may also be explained by the high mean age (52 ± 11.75 years) of our study group considering that COVID-19 mortality increases with age (13). Nonetheless, what is clear from our study is that the situation of hospitalized liver and kidney transplant patients afflicted with COVID-19 may be worse in Iran than in other countries, and further efforts must be devised to prevent and, when necessary, manage this disease in this high-risk population group.
It can be concluded that, following the trend described in studies from other countries, liver and kidney transplant patients afflicted with COVID-19 in Iran experience a higher rate of severe disease and mortality than the general population.