1. Context
HIV/AIDS has been one of the most important challenges of public health in the last few decades (1). By the end of 2018, about 37.9 million people were living with HIV, 770000 died from HIV-related causes, and 1.7 million were newly infected in 2018 (1, 2). Prevalence and mortality rates among 15 - 24-year-old people were 3.5 million and 45000, respectively (1, 2). Although there are different estimates of HIV prevalence, they give information about the trends of HIV prevalence around the world (3). According to the Joint United Nations Program on HIV/AIDS (UNAIDS) report in 2019, among the countries in the Middle East and North Africa (MENA) region, Iran was on the top with 61000 cases living with HIV, of whom 2400 patients were in the age range of 15 - 24 years (4). Importantly, the majority of HIV-infected population in Iran still remains undetected and unregistered (5).
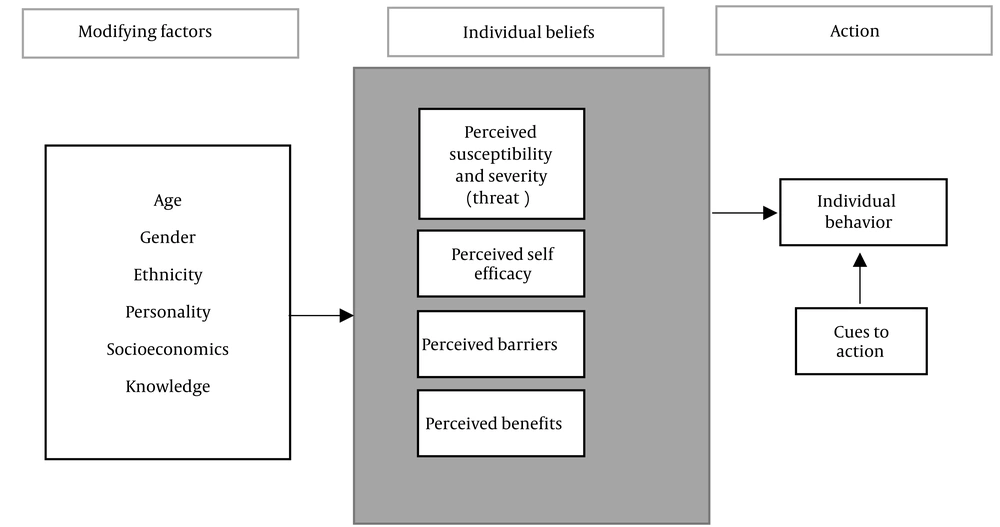
In Iran, people aged 15 - 24 years make up a significant portion (almost 15%) of the population (6). Some factors such as increasing age of marriage, risky sexual behaviors (7), and high rate of drug use (8) have posed Iranian youths at a high risk for risky behaviors, and consequently being infected with HIV/AIDS. Although many papers have studied the knowledge, attitude, and practice of youths toward the issue, few Iranian studies have assessed such issues as perceived risk, perceived risk susceptibility, perceived self-efficacy, perception barriers and benefits, and cues to action. Since future effective interventional programs should be based on new evidence, this systematic review was carried out to help the national health policymakers in this area. We utilized the Health Belief Model (HBM) (Figure 1), which is used for health promotion and disease prevention programs, as well as predicting individual changes in health behaviors (9).
Health belief model components and linkages (9)
2. Objectives
The main objective of this study was to assess the knowledge, attitudes, risk perception, and practices of Iranian youths toward HIV/AIDS. Meanwhile, the specific objectives were to determine the role of HBM components in relation to HIV/AIDS and its related risky behaviors among Iranian youths (Figure 1).
3. Evidence Acquisition
3.1. Search Strategy
To find the related published studies, three online databases, including Scopus, PubMed, and Web of Science were searched with no date restriction. The search keywords were as follows: ‘HIV’, ‘AIDS’, ‘knowledge’, ‘attitudes’, ‘risk susceptibility’, ‘risk perceptions’, ‘practices’, ‘alcohol’, ‘sexual transmitted disease (STD)’, ‘sexually transmitted infection (STI)’, ‘drugs’, ‘reproductive health’, ‘Iran’, ‘youths’, ‘young’, ‘adolescents’, ‘teens’, ‘teenagers’, and ‘student’. Only studies published in English language focusing on the Iranian people were included. Also, the studies that combined information of all age groups were excluded if the data of youths could not be extractable from the articles.
3.2. Screening of the Articles
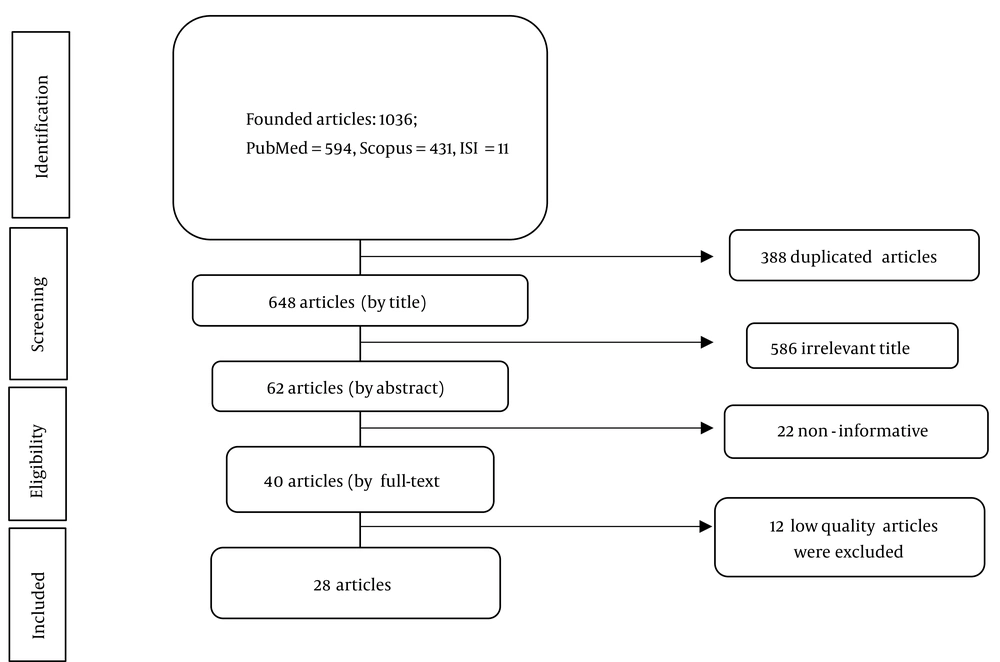
The searching process was conducted from December 2019 to April 2020 and was accomplished by a team of two independent researchers along with a supervisor to resolve any possible disagreement between them. The selection of articles was planned through three main steps (Figure 2). Firstly, we checked titles of all papers and removed the duplicated ones. Then, abstracts of remained papers were read carefully to insure if they are matched with the subject of the study. Finally, the full-texts of studies that were completely relevant to the topic of this review were entered into the quality assessment stage.
3.3. Quality Assessment
The quality of selected studies was assessed using two standard checklists, including the strengthening the reporting of observational studies in epidemiology (STROBE) checklist (10) and the preferred reporting items for systematic reviews and meta-analyses for protocols (PRISMA-P) (11). The STROBE and the PRISMA-P checklists consist of 22 and 27 items, respectively. The score 1 was considered for each item of the checklists which were met by the selected articles, and 0 for those which were not met. Accordingly, the studies which were scored over 70%, between 40 and 70%, and lower than 40% of the total achievable score were categorized into three groups of A (high-quality), B (moderate-quality), and C (low-quality), respectively. Finally, the articles of groups A and B were included in the study.
4. Results
4.1. Characteristics of the Studied Articles
The initial search resulted in 1036 articles, including 594, 431, and 11 articles from PubMed, Scopus, and Web of Science, respectively. After removing the duplicate articles (n = 388) and papers with irrelevant titles (n = 586), 62 abstracts were remained to be reviewed. Out of all the included abstracts, 40 were considered as appropriate for full-text assessment, of which 12 were excluded due to low quality (group C) (Figure 2). Finally, 28 papers (11 in grade A and 17 in grade B) were included in this study. Among the included articles, 11, ten, nine, and three of studies assessed knowledge, attitudes, risk perception, and practices of youths toward HIV, respectively. Most studies (n = 26) had a cross-sectional design, and two were systematic reviews. Six studies were conducted at national level, and nine were performed in Tehran, the capital city of Iran. The majority of studies (n = 17; 60.7%) were carried out among both males and females, while seven (25%) and four (14.3%) studies were conducted only among females and males, respectively. A total of 34,628 individuals were studied in these 28 articles. The number of subjects in the reviewed studies ranged from104 to 4,868 individuals. Seven studies were conducted in the universities, five among adolescents, three among high school students, three in the general population, three in the young adults, three in the female sex workers (FSWs), two in pre-university and college students, one in singles, and one in the people who inject drugs (PWIDs). Tables 1 and 2 summarize the characteristics and findings of the analyzed articles, respectively.
| Authors | Study Design | Place of Conducting Study | Sample | Gender (M/F) | Population Description | Mean/Range of Age (y) | Index |
|---|---|---|---|---|---|---|---|
| Abedian and Shahhosseini, 2014 (12) | Cross sectional | Sari, Iran | 548 | M/F | University students | 21.57 | Opinions toward facilitators and barriers of sexual and RH services |
| Alimoradi et al., 2017 (13) | Systemic review | National, Iran | 16 | F | Adolescents | ND | Factors contributing to the high-risk sexual behaviors |
| Armoon et al., 2017 (14) | Cross sectional | Kermanshah, Iran | 433 | M/F | PWIDs | 33.5 ± 7.6 | Drugs injecting and sexual behavior, exposure to harm reduction, and interventions for HIV prevention |
| Baheiraei et al., 2013 (15) | Cross sectional | Tehran, Iran | 1201 | M/F | Adolescents | 16.74 ± 1.09 | Prevalence of alcohol and substance use and associated factors |
| Bahrami and Zarani, 2015 (16) | Cross sectional | Kermanshah, Iran | 151 | M | University students | 23 | Correlation between knowledge, motivation and risk perception toward HIV/AIDS and risky sexual behaviors |
| Esmaeilzadeh et al., 2015 (17) | Cross sectional | Jolfa and Hadishahr, Iran | 156 | M/F | University students | 22.15 ± 2.07 | Sexual risky behaviors, the adoption on danger or fear management processes based on the Extended Parallel Process Model variables, self-control trait, and general self-efficacy |
| Khalajabadi Farahani et al., 2018 (18) | Cross sectional | Tehran, Iran | 642 | M | University students | 22.03 ± 2.76 | HIV/STIs-related sexual risk-taking behaviors and risk perception |
| Ghabili et al., 2008 (19) | Cross sectional | Tabriz, Iran | 300 | F | High school students | 17.9 ± 0.16 | Attitude towards HIV/AIDS |
| Haghdoost et al., 2014 (20) | Cross sectional | Kerman, Iran | 1024 | M/F | High school students | 16.4 | Influences of family, risky and protective factors on the adolescents’ risky behaviors |
| Hejrati et al., 2012 (21) | Cross sectional | Toyserkan, Iran | 167 | M/F | Pre-university students | ND | Relationship between background variables and awareness towards HIV/AIDS |
| Honarvar et al., 2016 (7) | Cross sectional | Shiraz, Iran | 1076 | M/F | Singles | 24 ± 5.8 | PMS and its Determinants |
| Khajehei et al., 2013 (22) | Cross sectional | Shiraz, Iran | 557 | M/F | Adults (at pre-marital counselling) | Males: 25.5 ± 5.1; Females: 21.2 ± 4.4 | Knowledge and attitudes towards Sexual and RH |
| Khalajabadi Farahani et al., 2015 (23) | Cross sectional (mixed-method) | Tehran, Iran | 1743 | F | College students | 21.90 | Perceptions of the societal acceptability and acceptability among peers of different types of premarital heterosexual relationships |
| Kolahi et al., 2011 (24) | Cross sectional | Tehran, Iran | 256 | F | FSWs | 26.8 ± 6.1 | Knowledge and attitude towards STIs and AIDS and their preventions |
| Salehi et al., 2008 (25) | Cross sectional | Bandar Abbas, Iran | 2123 | M/F | General population | 15 - 64 | Knowledge and attitude toward HIV/AIDS |
| Shamshiri Milani and Azarghashb, 2011 (26) | Cross sectional | Tehran, Iran | 104 | F | University students | 21.3 ± 1.9 | Knowledge, attitude, and practice towards STDs and sexual relationships |
| Mirzaee et al., 2017 (27) | Cross sectional | National, Iran | 3246 | M/F | Iranian adults | 19 - 29 | Reasons for inconsistent condom use |
| Mohammad et al., 2007 (28) | Cross sectional | Tehran, Iran | 1385 | M | Adolescents | 15 - 18 | Correlates of sexual risk-taking behaviors |
| Mohammadi et al., 2006 (29) | Cross sectional | Tehran, Iran | 1385 | M | Male adolescents | 16.6 | RH knowledg, attitudes, and behaviors |
| Panjalipour et al., 2017 (30) | Systematic review | National, Iran | 9 | F | Adolescents | Teenagers | RH needs |
| Rahimi-Naghani et al., 2016 (31) | Cross sectional | Tehran, Iran | 755 | M/F | General Population | 29.4 ± 8.30 | Knowledge about sexual and reproductive health |
| Ramezani Tehrani and Malek-Afzali, 2008 (32) | Cross sectional | Saravan, Astara, Eslamshahr, Kermanshah, Iran | 1005 | M/F | Young people, truck drivers, FSWs | 15 - > 25 | Knowledge, attitudes, and behaviors about HIV |
| Sajadi et al., 2010 (33) | Cross sectional | National, Iran | 1005 | F | FSWs | 31.8 ± 9.1 | Prevalence of HIV risky behaviors |
| Shokoohi et al., 2016 (34) | Cross sectional | National, Iran | 4868 | M/F | Young population | 15 - 29 | Knowledge, attitudes, and practices about HIV |
| Simbar et al., 2005 (35) | Cross sectional | Ghazvin, Iran | 1111 | M/F | University students | Females: 21.4 ± 2.4; Males: 22.7 ± 3.5 | Knowledge, attitudes, and practices about RH |
| Tavoosi et al., 2004 (36) | Cross sectional | Tehran, Iran | 4641 | M/F | High schools | 16.2 | Knowledge and attitude about AIDS |
| Vakilian et al., 2016 (37) | Cross sectional | Shahrood. Iran | 1500 | M/F | University students | 18 - 24 | Knowledge, attitudes, and self-efficacy about condom use |
| Zadeh et al., 2018 (38) | Cross sectional | National, Iran | 3246 | M/F | Young adults | 19 - 29 | Prevalence and correlates of HIV testing |
Abbreviations: RH: reproductive health; ND, not defined; PWIDs, people who inject drugs; STIs, sexually transmitted infections; PMS, premarital sex; FSWs, female sex workers; STDs, sexually transmitted diseases.
| Authors | Findings | Conclusions and Recommendations |
|---|---|---|
| Abedian and Shahhosseini, 2014 (12) | Mean score of personal and structural factors were significantly higher than interpersonal ones toward facilitators and barriers toward sexual and RH services. | Sexual and RH services must be provided for young people through the enforcement of facilitators and reduction of barriers. |
| Alimoradi et al., 2017 (13) | Factors influencing high-risk sexual behaviors in girls are personal, family, peer, school, and community factors. | Appropriate individual, family or school-based interventions can be designed and implemented to strengthen protective factors. |
| Armoon et al., 2017 (14) | 36% of participants reported high risk perception about HIV; Methamphetamine use and using multiple drugs at the same time were associated with the higher risk perception about HIV; PWIDs who were NSP users had higher risk perception than non-NSP users. | Predictor factors for risk perception about HIV were: initiating drug use at a younger age, using methamphetamine, poly drug use, and NSP utilization. |
| Baheiraei et al., 2013 (15) | 15.1% of adolescents had a history of alcohol consumption, which was higher in males than females; 3.1% of adolescents had a history of using opium and marijuana; 5.6% of adolescents had used ecstasy. | Gender-based interventional plans aimed at improving adolescents’ health by protection of them from substance abuse is recommended. |
| Bahrami and Zarani, 2015 (16) | Significant relationships were found between risky sexual behaviors and knowledge, motivation, and risk perception. | The risk perception is considered as the first step toward modifying sexual behaviors from risk-taking behaviors to safer behaviors; Compared to other variables, the perception of the risk of being afflicted by AIDS is a stronger predictor of the type of risky sexual behavior. |
| Esmaeilzadeh et al., 2015 (17) | 31.3% of the university students were in the fear management process; 68.7% were in the danger control about HIV/AIDS and the presence of multiple sexual partners and amphetamine consumption; Weakness in self-control and not having appropriate perceived susceptibility were significantly related to having MSPs; High level of self-efficacy significantly increased the probability of condom use. | Increasing unsafe-sex among youths showed the necessity for the preventive interventions as a serious issue of health services; The emphasis on the self-control factor in health education programs designed for the young people could play a certain role in effectiveness of the health promoting plans. |
| Khalajabadi Farahani et al., 2018 (18) | Respondents had a very low level of risk perception about HIV/STI. Only 3.4% were worried about being infected by STIs in the near future. | For protecting youth high risk sexual behavior, a complex of sexual abstinence, postponement of first sex, and clear health messages is recommended. |
| Ghabili et al., 2008 (19) | The mean attitude score was 59.9 ± 7.8 (out of 100); Only 6% of the students had a positive attitude towards HIV/AIDS. | HIV/AIDS education for Iranian students should be outspread beyond the schools to the society and families; The roles of health staff should be considered in school HIV/AIDS programs and media. |
| Haghdoost et al., 2014 (20) | Significant risk factors toward risky behavior were: age, being male, family history of antisocial behavior, and parental attitudes favorable toward antisocial behavior; Protective factors against risky behaviors were: father’s level of education (linear effect, AOR = 0.4), family religiosity (AOR = 0.6), and family attachment (AOR = 0.7) | Family has a very significant role in protecting youths against risky behaviors, and this role should be regarded in the interventional plans for protection of them. |
| Hejrati et al., 2012 (21) | Male students’ awareness towards AIDS was less than the females; Students studying experimental sciences had a relatively higher information about AIDS. No significant relationship was found between the level of education of the students’ parents and their children’s awareness towards AIDS. | Similar studies should be conducted in other regions and with more sample size. |
| Honarvar et al., 2016 (7) | 50% of the singles with history of PMS indicated that they intended to continue their sexual relationships; In 80.3% of singles who had PMS, sexual need was the main reason for having such relationships, while emotional need was reported by 8.1% of them; Among singles with PMS, 54.1% had MSPs; 33.9% of singles used alcohol, 23.3% smoked cigarettes, and 5.2% used opium. | Multidisciplinary interventions are needed to protect youths against risky behaviors. |
| Khajehei et al., 2013 (22) | Knowledge of males and females towards sexual and RH was low; Both males and females had poor knowledge about genital anatomy, STIs, and contraceptive application; The majority of participants had positive attitudes towards implementing educational programs on sexual and RH issues for youths before marriage. | To achieve health promotion policies, there should be efficient educational programs and a variety of teaching and learning strategies providing up-to-date information. |
| Khalajabadi Farahani et al., 2015 (23) | 77.5% of participants claimed that PMS was socially prohibited, while 33.1% were hesitant about the social acceptability of dating before marriage; Although youths in Tehran were still committed to traditional culture regarding premarital social interaction and romantic relationship, the study showed that a significant proportion of this group did not respect these values. | The great dilemma facing Iran is whether the trend towards greater socialization between elite young males and females should be tolerated as a healthy; development without incurring the risk of an increase in clandestine sexual relationships. |
| Kolahi et al., 2011 (24) | A small number of participants realized anal intercourse (44.9%) and oral sex (23.4%) as routes of HIV transmission; Majority of participants knew that currently AIDS has no certain treatment (81.2%) and no vaccines (73.4%); Most participants (59.4%) know that HIV can be transmitted from people who do not know that they are HIV-positive; 43.4% of participants knew that an HIV-positive individual may seem healthy. | Detecting at-risk individuals, HIV-positive sex workers, and educational campaign to improve attitude toward AIDS should be considered as high priority in Iran. |
| Salehi et al., 2008 (25) | The majority of interviewees had a low knowledge toward HIV/AIDS; Age and education were correlated with the knowledge of HIV/AIDS; Negative attitude regarding HIV-positive persons were common; People with higher education had more positive attitudes compared to the less educated ones. | There is a lot of evidence to include HIV/AIDS education in the high school curriculum; Educational advisors, physicians, and nurses have a main role in educating the community about preventive routes of HIV transmission. |
| Shamshiri Milani and Azarghashb, 2011 (26) | Only, 1% of students had acceptable knowledge and the remaining had very low and low level of knowledge; 28.3% of students guessed that their intimate friends have sexual relationships with their boyfriends. | More educational opportunities must be provided for students, especially females; Life skills learning programs should be available for youths; To discover the reasons of unsafe sex and risk behaviors, more studies should be performed. |
| Mirzaee et al., 2017 (27) | 19.5% of adults had ever-extramarital sex; 77.9% did not use condoms regularly; In 49.3% of cases, the reason for inconsistent condom use was its inaccessibility; Significant associated factors with inconsistent condom use were: age, gender, knowledge about HIV, attitude towards HIV, knowing infected HIV person, and alcohol or stimulant(s) used before sexual contact. | Health providers should provide accessibility to condoms in adults with low knowledge about HIV; Distributing condoms freely among rural adults aged 19 - 24 years old, adults who used ecstasy, and those knowing infected HIV persons can help them preclude inconsistent condom use; Promotion of the culture of condom use as a routine is needed |
| Mohammad et al., 2007 (28) | Predictors of condom non-use were: having no access to the Internet, feeling regretful at sexual debut, having one sexual partner in lifetime and low knowledge about condoms; Predictors of MSPs among adolescents were: older age, using alcoholic drinks, early sexual debut, and poor knowledge about reproductive physiology | Effective interventions are necessary in Iran to encourage youths for delaying their firs sex and abstinence of unwanted penetrative sex; Putting stress on the health risks of alcohol use is needed; Enhancing knowledge on different aspects of RH and prevention against STI/HIV is needed. |
| Mohammadi et al., 2006 (29) | The relatively high prevalence of sexual activity and the lack of knowledge regarding STIs and contraceptives pose a significant threat to the sexual RH of male adolescents in Iran. | Programs are needed to provide adolescents with the information and skills to make safe sexual decisions. |
| Panjalipour et al., 2017 (30) | Most of the adolescents have unmet needs for RH services, while current services are not friendly; General groups of RH needs are: special educational needs, comprehensive counseling, and adolescent-friendly services. | Interventions to improve adolescents’ RH are needed. |
| Rahimi-Naghani et al., 2016 (31) | Males and females were moderately knowledgeable about sex and RH; Myths and misperceptions about different aspects of SRH existed; Significant predictors of better SRH knowledge were: being female and being married; Significant predictor of poor SRH knowledge was being at age group 15 - 24 years. | People need comprehensive education toward sexual reproductive health. |
| Ramezani Tehrani and Malek-Afzali, 2008 (32) | Knowledge about HIV was low on average, especially among individuals with high-risk behaviors; Youths had lower knowledge about STIs than cross border truck drivers and FSWs; Youths had a less positive attitude toward temporary marriage and pre- and extramarital sex than truck drivers; Condom use was low in all groups. | The need to create a supportive environment through a multi-sector religious, political, and programmatic approach is recommended for the implementation of effective prevention activities among high-risk groups and the general population. |
| Sajadi et al., 2010 (33) | The prevalence of HIV infection was 4.5% in FSWs, while it was 4.8% among those who were drug users and 11.2% in injection drug users; In the last sexual contact with paying clients, the rate of condom use was 57% and in non-paying clients was 36.3%; 73.8% of participants were drug users, while 20.5% were injection drug users. | A combination of prevention attempt targeting; high-risk sexual contact and injection are needed; Preventive interventions like condom use and clean syringe use are immediately needed. |
| Shokoohi et al., 2016 (34) | 69.1% of 19 - 29 years old participants reported mass media as the main source of HIV information; 13.1% had ever tested for HIV; 1.8% ever injected drugs including 2.9% males and 0.7% females; Consistent condom use was reported by only 21.8% (26.1% males and 7.1% females) of sexually active persons in this age group. | HIV health promotion research should focus on understanding how socio-cultural and religious value affect youth’s sexual lifestyle and information access; In HIV education programs, strategic plans should also emphasize involving the key individuals in youth’s networks like parents, teachers, and peers. |
| Simbar et al., 2005 (35) | The overall knowledge was 54%; Knowledge of male, female, married, and single participants was similar. 8% reported having sexual intercourse before marriage; 48% had used condoms. | Policy-makers and health authorities need to pay more attention to strengthening those aspects of social culture that keep youths safe; An appropriate strategy, which has been suggested by other predominantly Muslim countries such as Malaysia, Oman, and Egypt, is to integrate teaching of Islamic values into RH education and promotion programs. |
| Tavoosi et al., 2004 (36) | Only a few students answered all the knowledge questions about HIV/AIDS correctly, and there were many misconceptions about the routes of transmission. Knowledge was associated with the students' attitudes and discipline. | It is rational to have HIV/AIDS education as a part of high school curriculum and it should be presented by physicians, nurses, and educational advisors. |
| Vakilian et al., 2016 (37) | Knowledge about condoms in females was lower than males. 9.1% of females and 1.1% of males had a good self-efficacy about condom use. 16% of females and 27% of males had used condom during intercourse. | Knowledge and attitudes towards condoms and self-efficacy of condom use should be incorporated in AIDS control and training programs. |
| Zadeh et al., 2018 (38) | Only 13.6% of the youths had ever tested for HIV. | Promoting and pilot-testing of novel web-based and self-testing approaches, de-stigmatization of HIV testing, and accepting sexual health education in schools could improve HIV testing of youths in Iran. |
Abbreviations: RH, reproductive health; AOR, Adjusted Odds Ratio; PWIDs, people who inject drugs; NSP, needle and syringe program; MSPs, multiple sexual partners; STIs, sexually transmitted infections; PMS, premarital sex; SRH, sexual and reproductive health, FSWs, female sex workers.
4.2. Knowledge
Among the included studies, 40% of the papers evaluated the level of youths’ knowledge toward HIV/AIDS (16, 21, 22, 24-26, 31, 32, 34-36). Four studies showed that youths were moderately knowledgeable about sexual and reproductive health (16, 31, 34, 35). However, other studies indicated that the overall knowledge level of youths was low (22, 25, 26, 32, 36). The study by Shamshiri Milani and Azarghashb revealed that only 1% of students had an acceptable level of knowledge about HIV/AID (26). In one survey, only 30% of participants gave true answers to four knowledge-related questions about condom (37). Older age, being female, being married, higher level of education, urban citizenship, and higher socioeconomic status were significantly associated with being more knowledgeable about HIV (25, 31, 34). Simbar et al. stated that there was no difference between married and single individuals regarding their level of knowledge about reproductive health, contraception, and HIV and sexually transmitted diseases (STD) (35). In another study, cultural beliefs and religious issues were reported as the reasons for low levels of knowledge about sexual reproductive health (SRH) (22). Tavoosi et al. reported that the level of knowledge among students was associated with their attitudes and discipline (36). In terms of education, three studies revealed a positive association between the level of education of youths and their knowledge about AIDS (22, 25, 35). However, another survey did not show such an association (26). According to the study by Bahrami and Zarani, university students were generally knowledgeable about HIV/AIDS (16). Simbar et al. showed that 72% of college students knew that condom is a contraceptive method (35). However, other studies found that schools or universities have not played effective roles in increasing youth’ knowledge about HIV/AIDS (25, 34, 36). In addition, the level of knowledge among technical and non-technical university students was similar (29). Another study in two universities in Iran showed that higher level of knowledge and attitudes toward HIV/AIDS among university students were significantly correlated with a higher level of education in their parents (17). Also, Simbar et al. showed that the higher level of knowledge and attitudes of youths were significantly correlated with the higher level of education of their mothers (35). However, three studies demonstrated no significant relationship between parental education and youths’ knowledge about AIDS (19, 21, 32, 36). Khalajabadi Farahani and Cleland concluded that parents’ level of education and income were associated with their children liberality in premarital heterosexual relationships (23). Considering the trend of knowledge toward HIV/AIDS, studies showed an increasing trend from very low and low to a relatively moderate level of knowledge between 2002 and 2016 (22, 24-26, 28, 31, 32, 34, 36), while misconceptions about condom, STIs, reproductive physiology (31), and routes of HIV/AIDS transmission (34, 36) remained unchanged. With regard to the age, five studies evaluated the correlation between knowledge toward HIV/AIDS and age, of which four studies showed a significant positive correlation between knowledge and age (31, 32, 34, 35), while one study revealed a reverse pattern between these factors (25). Regarding gender, six studies assessed the role of gender in the level of knowledge toward HIV/AIDS. The level of knowledge between both genders was similar in two studies (25, 35), while three studies showed a higher level of knowledge about AIDS among females (21, 31, 34). Also, one study revealed a low significant association between gender and youth s’ knowledge (36). Moreover, Shokoohi et al. showed that knowledge of females about reproductive physiology, STIs, various contraception methods, and benefits of condoms was higher than males. However, men were more aware of how to use condoms (34). In terms of sources of knowledge (as a cue to action component in HBM), mass media was mentioned as the main source of information about HIV/AIDS by most of the young groups (25, 34, 36). One of these studies showed that media (69.1%) along with family, friends, and acquaintances (40.9%) were two main sources of HIV-related information. This study also reported that the Internet (39.9%) and schools or universities (35.4%) were the other sources of information about HIV/AIDS (34). In another study, friends and peer groups were identified as the primary or secondary sources of information about puberty and sex-related issues (31). It was also revealed that by increasing age, the preferred source of information about biological aspects of SRH would change from the Internet and media to the teachers (31). In addition, other studies focused on the unmet educational needs of adolescents and the lack or inefficiencies of needed interventions (30, 34). One important challenge is that media, as one of the potential main sources of information for young people, does not have a legal and official role in education and training of youths toward sexual issues in Iran (14, 22). Thus, lower level of sexual knowledge in youths leads to consequences, such as negative attitudes towards HIV-positive people and condom use (14, 22).
4.3. Attitude, Threat Perception, and Self-egfficacy
The attitude toward HIV/AIDS was studied in more than 30% of the selected articles (7, 19, 22, 23, 25, 29, 32, 34, 36, 37). According to the study conducted by Ghabili et al., the mean score of attitude among high school students was 59.9 ± 7.8 (out of 100), while the score of 75 or above was considered as a positive attitude. Regarding attitude in students, 6% of participants stated positive attitude about HIV/AIDS (19). However, in the study by Salehi et al., this value was reported as 46%, while the participants with a higher level of education had a more positive attitude toward HIV-infected people, and there was no significant difference in attitudes of males and females about HIV/AIDS (25). Shokoohi et al. revealed that 74.6% of individuals had negative attitude toward HIV/AIDS, while older students, female students, and urban citizens had a better attitude (34). Tavoosi et al. showed that 46% of students believed that HIV-infected students should not attend ordinary schools (36). Mohammadi et al. indicated that the students who did not attend day schools, the students who had studied in non-governmental schools, and who had work experience, as well as the students who lived separately from their parents and had access to the Internet and satellite channels or consumed alcohol, had a more permissive attitude towards premarital sexual relationships (PSR) (29). Khajehei et al. mentioned that the mean score of attitude toward SRH among males was higher than females (5.37 vs. 4.48) (22). According to the study by Khalajabadi Farahani and Cleland, 77.5% of female college students believed that PSR is socially prohibited (23). In a study by Ramezani Tehrani and Malek-Afzali, 36.9% of youths had a positive attitude toward PSR (32), while 55% in the study by Mohammadi et al. believed that PSR should be prohibited (29). Regarding the condom use, 71% of university students had a moderate attitude toward it (37). Also, in the study by Honarvar et al., 52% of participants declared that condom could completely prevent STD, while 16.4% of them denied such efficacy (7). Four articles presented information about the perceived susceptibility (17, 18, 34, 38), of which two studies did not target perceived susceptibility directly but rather discussed HIV testing, which could be an indicator of perceived susceptibility (34, 38). One study indicated that 13.6% of participants had tested for HIV (38), similar to the study by Shokoohi et al., in which only 13.1% of participants had tested for HIV. Also, 6.5% (8.1% male vs. 4.9% female) of the participants tested for HIV in the past year (34). Zadeh et al. stated that low perceived susceptibility can be attributed to the young age, while those who were educated, male, or married showed a higher rates of HIV testing (38). Another survey concluded that 6.5% of participants were worried about being infected by HIV over the earlier year of the study (18). Esmaeilzadeh et al. reported that the low perceived susceptibility increased the chance of having multiple sexual partners (MSPs) by 34% (17). Risk perception toward HIV was also addressed by two articles (14, 16). A study by Armoon et al. showed a higher level of risk perception among PWIDs. In addition, they implied that initiating drug use at a younger age, using methamphetamine, poly-drug use, and attending in needle and syringe exchange program were predictors of higher risk perception about HIV in PWIDs (14). Bahrami and Zarani reported that the mean score of risk perception among university students was 22.37 ± 2.95 (out of 30), and concluded that there was a significant relationship between HIV risk perception and sexual behavior among male students. Therefore, this item should be considered as the first step to modify sexual behaviors from risky behaviors to safer ones (16). Self-efficacy is defined as the strength a person believes she/he has, which gives the ability to perform a task and fulfill them. Such a person expects a desirable consequence when performing a special behavior (18). As a result, perceived self-efficacy leads to a higher ability in avoiding high risk sexual behaviors or results in a higher rate of condom use (18). Among the studied articles, two papers discussed self-efficacy toward prevention of HIV/AIDS (18, 37). A study by Vakilian et al. showed that only a small percentage of female (9.1%) and male students (1.1%) had a high level of self-efficacy about condom use, while 68.4% and 77.5% of males and females had medium self-efficacy and 30.5% versus 13.4% of them had low self-efficacy about condom use, respectively (37). In the second study by Khalajabadi Farahani and Cleland, self-efficacy was the most important predictor of condom use (18). Esmaeilzadeh et al. concluded that low self-efficacy resulted in low condom use (17).
4.4. Practice
In terms of alcohol, cigarette, and drug use, three studies showed that 15.1 - 33.9% of youths had consumed alcohol (7, 15, 17), which was significantly higher in the males than females (15). Furthermore, 23.3 - 28.8% had a history of smoking (7, 17), and 5.6 and 5.8% of the youths had ever used ecstasy and psychoactive drugs, respectively (15, 17). Shokoohi et al. showed that 8% of the youths aged 15 - 29 years had ever injected drugs (34), while 3.1 - 5.2% of the adolescents consumed opium and marijuana (7, 15). The factors leading to higher use of alcohol in female adolescents were low parental control, lifetime cigarette use, and having a friend who uses tobacco and alcohol, while the determinants for male adolescents to use alcohol were studying in the private schools rather than public schools, lifetime cigarette use, lifetime water pipe use, experiencing sexual relationship, having a friend who uses alcohol, and having a water pipe user in the family (15). Another study found that among singles aged 15 - 29 years, alcohol use was strongly associated with PSR, followed by the lack of religious beliefs (7). The determinant factors of smoking were age, being male, mother’s level of education, family history of antisocial behavior, and favorable attitude of parents toward antisocial behavior (20). However, the protective factors against smoking were religious family, father’s level of education, and family integration (20). In terms of PSR, 11 articles provided evidence about sexual behaviors among youths (7, 13, 17, 18, 27-29, 32, 34, 35, 38), of while four studies reported the rate of premarital sexual contact between 8 and 50% (7, 18, 32, 35), including 19.5 - 20.8% in the participants aged 19 - 29 years (27, 34). In one study, it was reported that the median age for the first sexual contact of youths was 18 years. Also, 41% of singles were heterosexual, and 5.6% were bisexual (7). There are four general factors leading to the risky sexual behaviors among girls, including personal factors, family, peers, and school (13). Abedian and Shahhosseini showed a more essential role for personal and structural facilitators and barriers compared to the interpersonal ones in sexual and reproductive health of youths (12). Furthermore, 50 - 85% of those who had premarital sexual contacts expressed to have MSPs during their lifetime (7, 18, 29). Older age, using alcohol, poor knowledge about reproductive physiology (28), early sexual debut (before age 18), studying in the private university, watching pornography, and having work experience were among the predictors of having MSPs during lifetime (18). Regarding condom use and its predictors, one third of selected articles estimated the rate of condom use among youths between 22 and 57% (7, 17, 18, 27, 32-35, 37). Khalajabadi Farahani et al. revealed that 31% of participants had used condom in their first sexual contact and about 57% in their last sexual contact (18). As reported by another survey, nearly 50% of the FSWs and 35% of males did not use condom in their sexual contacts (32). In another study, the rates of condom use were 57 and 36% among paying and nonpaying clients, respectively (33). Out of all singles with PSR, 23.8% never used condom, and 42.2% used it inconsistently (7). Mirzaee et al. showed that 22% of participants had used condom regularly (27), while this rate was 49% in the study by Simbar et al. (35). In the study by Shokoohi et al., 21.8% of the participants used condom consistently (34). A survey showed that reduction of pleasure was the most common reason for not using condom by males (32), while the lack of access to condom was stated by the participants in the study by Mirzaee et al. (27). However, FSWs mentioned that the cost of condom and the disagreement of their partners were their main reasons for not using condom (32). Other variables, such as age, gender, knowledge, and attitude toward HIV, knowing HIV-positive people, consuming alcohol, and psychoactive drugs led to the inconsistent use of condom (27). One of the variables which can increase the probability of condom use is the high level of self-efficacy (17). Furthermore, it was reported that only a small percentage of students (6.1%) had a good level of self-efficacy about condom use (37). The other factors contributing to not using condom were lack of access to the Internet, regrets after sexual debut, having one lifetime sexual partner, and low knowledge about condoms (28). In another study by Khalajabadi Farahani et al., having one lifetime sexual partner, poor knowledge toward HIV, and experiencing sexual contact at lower age were the predictors of inconsistent condom use (18).
5. Discussion
In this systemic review, most of the included studies measured knowledge and attitude, few studies assessed threat perceptions or cues to action, and limited studies detected the practices of youths toward HIV/AIDS. Less than half of the articles were conducted among young groups of the general population, while others were conducted among special groups of youths.
5.1. Knowledge
Many studies discussed in this review showed that the level of knowledge of Iranian youths about HIV/AIDS has increased from the low to intermediate level in the recent years. However, misconceptions about some aspects of HIV/AIDS, including routes of transmission, are still remaining; these misconceptions were also common among adults from Bahrain, as another Islamic country (39). Females, young adults, higher educated people, married individuals, urban youths, and those with higher socioeconomic status were more knowledgeable about HIV/AIDS. However, the parents’ level of education did not have a significant role. Similar to our study, the media, family, friends, and acquaintances were the main sources of HIV-related information in other parts of the world (40). Overall, unmet educational needs of adolescents and the lack or inefficiencies of needed interventions, which are necessary in the process of behavioral change to prevent them from getting HIV/AIDS, are still serious challenges, especially because it is still a taboo to discuss SRH and preventive routes of HIV/AIDS in the national media, schools, and universities. School programs expose the adolescents to the limited information about SRH, which is not balanced with their educational needs. This challenge also applies to the Iranian families, as they also follow socio-cultural norms around sexuality and refuse to discuss such matters openly. Similarly, one study showed that there was a lack of knowledge in the general population in the other parts of the world about STDs, including HIV/AIDS (40).
5.2. Attitude, Threat Perception, and Self-efficacy
In general, youths had a negative attitude toward HIV-positive patients, while older youths, higher educated ones, urban citizens, and females (in some studies) had a more positive attitude toward these patients. Low attitude toward HIV/AIDS was also noticed in seven Arabian Peninsula countries that are southern neighbors of Iran (41). In terms of PSR, attitude of the majority of youths was against permission of such relationships in the community. However, those who had history of alcohol use, work experience, living separately from their parents, and not attending the day schools were in favor of PSR. Regarding the perceived susceptibility as an important component of behavioral change, few surveys were conducted; and there was not a high prevalence in the youths. In other words, assuming that HIV/AIDS rate is low in the youths may result in unprotected risky behaviors, such as having MSPs. Similarly, risk perception was studied only in few studies, even though its modification needs to be considered among the first steps toward modifying sexual behaviors from risky behaviors to safer ones. In one study, it was shown that the association between HIV/AIDS knowledge and risk perception followed a wide range (positive to negative association) (40). Self-efficacy and its role to use protective measurements was not assessed by most of the studies; however, few studies showed that it was not high regarding condom use by youths, especially in males.
5.3. Practice
About one third of youths had a history of smoking or alcohol consumption, and at least one out of 20 young people had a histroy of drug use. The use of these materials are higher in males than females. Different factors, such as lifetime cigarette smoking, having friends who use these materials, and PSR, were associated with the alcohol consumption in the youths. Being male, family history of antisocial and risky behavior, and favorable attitude of parents toward antisocial behavior were among the risk factors, while family religiosity, father’s level of education, and family integration were among the protective factors of youths against smoking. PSR was also reported by about one fifth to one third of the young populations (42). According to one study, about one out of 20 singles were bisexuals. In this respect, personal factors, family, peers, and school contribute to the risky sexual behavior among females. Most of the youths with history of PSR mentioned that they had MSPs during their lifetime. Older age, alcohol consumption, poor sexual knowledge, beginning PSR before the age 18, studying in the private university, watching pornography, and having work experience were the predictors of having MSPs in youths. The rate of condom use was less than 50%, and the rate of consistency in the condom use was also less than 50% among the young people. Another study conducted in South Africa reported that despite the good risk perception toward HIV/AIDS, there is still inconsistency about condom use among university students (43). This was also supported by another study performed among university students of Thailand (44). The reasons for the low condom use were low knowledge, low self-efficacy, having one sexual partner in the lifetime, less pleasure, cost, disagreement of the sexual partners, lack of access to condom, lack of access to the Internet, and regrets after sexual debut. The reasons for inconsistent condom use were gender, younger age at sexual debut, low level of knowledge and attitude toward HIV, knowing HIV-positive people, and consuming alcohol and psychoactive drugs.
5.4. Strenght and Limitation
As a strength point of this study, we collected all the valid knowledge, attitudes, and practices (KAP) evidence regarding threat perceptions about HIV/AIDS, and we extracted the data based on HBM, as a popular behavioral change theory, which seems to be more applicable by policymakers compared to showing only the findings to them. Regarding limitations, we did not include unpublished theses and did not perform a metanalysis due to the wide heterogenecity and differences in their qualities. Further studies might evaluate the implemented policies for harm reduction of youths, as it is emphasized by another study (45).
5.5. Conclusions
The knowledge, perceived risk, and perceived susceptibility about HIV/AIDS are low in Iranian youth. So, more effective educational and training interventions should be planned and implemented for them.
5.6. Recommendations
Knowledge, threat perception, and preventive behaviors of youths toward HIV/AIDS were not high, while their attitude was generally negative and their premarital sexual contacts was increasing. Therefore, implementation of evidenced-based strategies and multifactorial interventions by health system, instead of denying or ignoring this growing public challenge is needed to protect these populations. The role of media, schools, universities, and peer groups to answer unmet SRH and HIV/AIDS-related unmet educational needs of youths should be accepted, valued, and their potentials should be used appropriately. It should be mentioned that these educational plans should be age-dependent and based on social context (46). Sexual reproductive health services for youths should also become legal, established and integrated into the current primary health care system, and spread across the country. However, it is essential to evaluate the policies currently implemented for harm reduction in the high risk groups.