1. Background
Over the last decade, remarkable changes have occurred in service provision in the healthcare industry. Patients’ increased expectations, technological advances, greater access to health-related information through digital media (the internet), and the development of a comprehensive approach to health and well-being are among the most important changes (1-3), leading to a more competitive market for health services. In a competitive market, organizations that prioritize customer loyalty succeed (4). Therefore, many health service providers are looking for strategies to retain their customers by providing high-quality services to meet their needs and desires (5). The moving of health systems from a service-centered approach toward satisfaction- and hospitality-based approaches, which affect people emotionally, is a factor that ultimately improves health care quality and increases customer loyalty to health organizations (6).
In addition to the quality of clinical services, the features of care, including the quality of hoteling services, care process, and interactions between patient and hospital staff, are important to enhance health services’ quality (7). Hoteling services (the physical environment and accommodations) have been identified as one of the dimensions of hospital service quality in previous studies (8). Currently, the healthcare industry recognizes the quality of hoteling services as one of the most important cornerstones of patient satisfaction and loyalty (1). The quality of hoteling services can be more important than the quality of clinical services for choosing a hospital from the patient’s perspective (1, 9). The proper design of the hospital and its infrastructure (such as light, color, sound, and ventilation) increase the safety of patients and staff (10). Patient satisfaction is also related to the quality of the hospital’s physical environment, accommodations, and hoteling facilities (2, 10, 11). The results of various studies indicate the positive effect of the physical environment on the patient's perception of hospital services’ quality (12-15).
In the past, hoteling services were limited to "housekeeping" and cleaning the public space of hospitals. Meanwhile, the word "hoteling" goes beyond housekeeping and includes several criteria. Hoteling services are defined as tangible services of healthcare providers. In another definition, hoteling includes "non-medical services provided to patients in a hospital" from admission to discharge, including physical factors (facilities, equipment, food, housekeeping, and accommodation), human factors (responsiveness, caring behavior, and physical appearance), functional factors (integrated services, patient-centeredness, and promptness), safety, economic factors, etc. (6).
Regarding the dissatisfaction of patients with the physical and accommodation facilities of public hospitals, a special package was developed to improve the quality of hoteling services in Iran's health transformation plan (HTP) (16). Improving the quality of hospitality services provided by the hospitals affiliated with the Ministry of Health and Medical Education is one of the costly priorities of the HTP packages. The package covers seven aspects: (1) Buildings and installations, (2) Equipment and facilities, (3) Welfare services, (4) Cleanliness and safety, (5) Food services, 6) Administrative affairs, and (7) Patient and staff education. The aim of this package is to improve the quality of hoteling services, meet the expectations of patients regarding hoteling services, and ultimately increase patient satisfaction (16). In this regard, and given the importance of this package, hoteling services are among the qualification items of Iran’s national hospital accreditation plan.
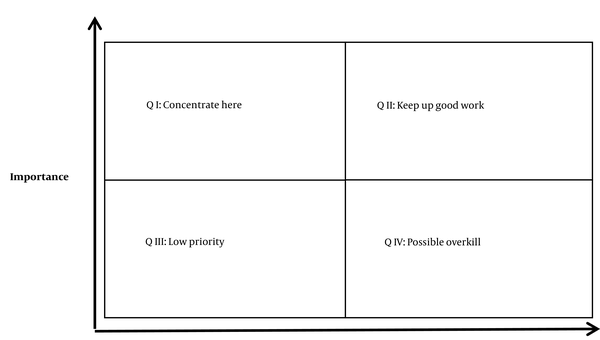
Patients’ perception is an important primary indicator of the quality of health services and an essential component for improving clinical performance and effectiveness (17). Since hoteling services are more focused on patients’ convenience and welfare, patient perception of the quality of hoteling services can help hospitals identify the areas and dimensions that can bring them competitive advantages (18). All perceived weaknesses may not matter to patients. Therefore, hospital managers seek a method to prioritize the hoteling services needed to be improved. Several tools have been introduced to measure the quality of services, which are different in terms of quality definition, content, and the type of measurement. The importance-performance analysis (IPA) is a method developed by Martilla and James to measure the relationship between performance (perceptions) and importance (expectations) (19). The advantage of this model is that it can quickly identify the strengths and weaknesses of an organization in terms of customer satisfaction. This model assumes that some quality features are more important than others; in other words, each feature is viewed differently.
Due to the increasing importance of IPA in identifying a system’s strengths and weaknesses and its efficiency in prioritizing items and adopting an improvement strategy, the model is used in various fields, including industry and trade (20), information technology (21), tourism & hospitality (22, 23), and higher education (24). In this regard, the health sector also uses IPA to improve patient safety (25), hospital services (26, 27), medical tourism (28), health information technology (29), etc.
2. Objectives
Due to the importance of measuring and analyzing the quality of hoteling services as a tangible quality component of hospital services, the current study aimed at ranking the dimensions of hospitals’ hoteling services in Iran using IPA from the viewpoint of patients.
3. Methods
The current cross-sectional study was conducted on 440 patients hospitalized in selected hospitals affiliated with Shahid Beheshti University of Medical Sciences in Tehran from June to September 2017. Willingness to participate in the study, hospitalization for at least 24 hours, and age above 18 years were considered the inclusion criteria. Patients with a low level of consciousness or critical conditions and patients who stayed in psychiatric departments, isolated rooms, and intensive care units were excluded from the study.
Shahid Beheshti University of Medical Sciences provides health services to a part of the population living in Tehran’s north, northwest, east, and southeast regions. Sampling was performed in several stages. First, from each region, a hospital was randomly selected (i.e., a total of four hospitals). The number of patients recruited from each hospital was proportional to the size of hospitalized patients in that hospital in the previous year. Accordingly, 80, 90, 210, and 60 patients were considered from the hospitals located in the north, northwest, east, and southeast regions, respectively. The subjects were selected using systematic sampling based on admission lists in each hospital. The researcher was present during the data gathering process and clarified research objectives to all patients. From 440 questionnaires distributed; all were returned (the response rate = 100%).
The data gathering tool was a questionnaire developed by Shirzadi et al. (9). The questionnaire consisted of 44 items (both on the importance and performance) in the six dimensions of hoteling services’ quality, including physical-structural (24 items), functional-process (six items), human-behavioral (six items), religious-cultural (three items), safety-security (three items), and economic-financial (two items). The reliability of the questionnaire was assessed through Cronbach's alpha, reporting a coefficient of 0.97 for both the importance and performance areas, confirming the tool’s internal consistency. Respondents answered each item on importance and performance, and a five-point Likert scale (very high, high, moderate, low, and very low) was used for scoring.
Data were analyzed using SPSS software version 21. Mean, standard deviation, and percentage were used to summarize descriptive data. The quality gap was calculated by deducting the performance and importance scores (Gap = performance - importance). The paired student t-test was used to compare mean differences in the two aspects of importance and performance. P values less than 0.05 were considered statistically significant.
The four-dimensional importance-performance (IP) matrix was used to prioritize the improvement points required in hoteling services (Figure 1). In this model, the mean values of performance and importance in each dimension were used to determine its coordinates, which were then displayed on the IP matrix. Thus, by pairing these two sets of values, each of the items was placed in one of the four quadrants of the IP matrix.
The hoteling services’ quality dimensions placed in the Q1 quadrant indicate that patients are more interested in such features but are not satisfied with their current performance. These features are the main weaknesses of the organization, and hospitals should pay more attention to them by developing appropriate improvement action plans as soon as possible. The Q2 quadrant of the IP matrix is a place for the hoteling service quality dimensions that were important to patients, and the hospital’s performance in that area was also high. Such attributes mark the organization’s main sources of strength. Features in the Q3 quadrant have a low priority for improvement since they are not very important to patients. These denote minor organizational weaknesses and need limited resources for improvement. Ultimately, the hoteling service quality dimensions placed in the Q4 quadrant are considered overemphasized. In other words, patients pay less attention to them, yet hospitals’ performance is beyond patients’ expectations. Therefore, the resources allocated to these features are needed and should be consumed elsewhere (30). The current research protocol was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences (code: IR.SBMU.REC.1396.76).
4. Results
Based on our findings, 48.6% of the patients were female, and the overall mean age was 40.4 (± 12.1) years. About 16% of the patients had a history of hospitalization in the hospitals studied. The average length of stay (LOS) was 4.9 (± 4.0) days. The LOS of 28.6% of patients was over five days, and most patients had health insurance (n = 392; 89.1%). Only 8.2% (n = 36) of patients stayed in single rooms, while 250 (56.8%) individuals were hospitalized in quad rooms (Table 1).
| Variables | No. (%) |
|---|---|
| Gender | |
| Male | 224 (51.4) |
| Female | 216 (48.6) |
| Age (y) | |
| 18 - 39 | 202 (45.9) |
| ≥ 40 | 238 (54.1) |
| Education level | |
| Basic | 292 (66.4) |
| Academic | 148 (33.6) |
| Length of hospital stay (d) | |
| 1 - 5 | 314 (71.4) |
| > 5 | 126 (28.6) |
| Prior history of hospitalization in the current hospital | |
| Yes | 70 (15.9) |
| No | 370 (84.1) |
| Health insurance | |
| Yes | 392 (89.1) |
| No | 48 (10.9) |
| Hospital room type | |
| Single | 36 (8.2) |
| Double | 70 (15.9) |
| Triple | 84 (19.1) |
| Quad | 250 (56.8) |
Patients’ Demographic Characteristics
The highest mean score of importance (4.11) belonged to the "human-behavioral" factor and the least (3.59) to the "cultural-religious" factor. The highest (3.55) and lowest" (2.86) mean scores of hospital performance were related to "human-behavioral" and "economic-financial" factors, respectively. In addition, the largest negative gap was observed in the "economic-financial" factor, and the smallest gap was related to the "functional-process" factor. In all dimensions of hoteling services’ quality, there was a significant negative gap between the performance of hospitals and the importance (i.e., patients’ expectations) (P < 0.001, Table 2).
| Dimensions | Importance (I), Mean ± SD | Performance (P), Mean ± SD | Gap (P-I) | P-Value | |
|---|---|---|---|---|---|
| F1 | Physical-structural | 3.85 ± 0.87 | 3.01 ± 0.83 | -0.84 | < 0.001 |
| F2 | Functional-process | 3.64 ± 0.83 | 3.13 ± 0.74 | -0.51 | < 0.001 |
| F3 | Human-behavioral | 4.11 ± 0.76 | 3.55 ± 0.92 | -0.56 | < 0.001 |
| F4 | Cultural-religious | 3.59 ± 1.03 | 3.03 ± 1.15 | -0.56 | < 0.001 |
| F5 | Safety-security | 3.76 ± 1.07 | 2.97 ± 1.19 | -0.79 | < 0.001 |
| F6 | Economic-financial | 3.89 ± 1.15 | 2.86 ± 1.21 | -1.03 | < 0.001 |
The Mean Scores of Importance, Performance, and Gap in Hospital Hoteling Services’ Quality
The matrix was drawn after the scores of importance and performance of quality dimensions were calculated. As mentioned, the mean of the study’s data was used to determine the coordinates of the point in the matrix. The mean scores of importance and performance were 3.1 and 3.8, respectively. The "physical-structural" and "economic-financial" dimensions were placed in the Q1 quadrant. This meant that hospitals’ performance in these factors was poor in spite of their high importance from patients’ perspectives. These factors were the main weaknesses of hospitals’ hoteling services and required immediate attention and appropriate improvement measures. The "human-behavioral” dimension fell in the Q2 quadrant, meaning that besides its high importance for patients, hospitals also had a good performance there. The "religious-cultural" and "safety-security" dimensions were placed in the Q3 quadrant. These factors had little importance for patients, where hospitals also had poor performance. Therefore, these factors had low priority for quality improvement. Finally, the "functional-process" dimension was placed in the Q4 quadrant, reflecting that it did not matter to patients, but hospitals performed well in it. Given their low importance, these factors are not considered remarkable strengths for hospitals (Table 3).
| Dimensions | Quadrants |
|---|---|
| Physical-structural, economic-financial | Q1: Concentrate here |
| Human-behavioral | Q2: Keep up good work |
| Cultural-religious, safety-security | Q3: Low priority |
| Functional-process | Q4: Possible overkill |
Prioritization of the Attributes and Dimensions of Hoteling Service Quality Based on the Importance-Performance Matrix
5. Discussion
The current study was conducted to evaluate the quality of hospital hoteling services from patients’ viewpoints. Our findings showed that in all quality dimensions of hoteling services, there was a significant difference between the performance of hospitals and the importance (patients’ expectations). In other words, the performance of the hospitals studied did not meet patients’ expectations in any aspect of hoteling services. The findings of previous studies in Iran suggested a significant gap between the perception and expectation of patients regarding the quality of hospital hoteling services (27, 31), which was consistent with the findings of the present study.
We observed that human-behavioral factors were the most important strengths of hospitals in terms of hoteling services’ quality, which can be regarded as a competitive advantage. In other words, the hospitals studied addressed this expectation of patients to a large extent, and therefore, they should continue to work in that direction. Studies on Iran’s public hospitals in 2016 and Tehran’s private hospitals in 2018 showed that from patients’ and their companions’ perspectives, human factors were the most important aspect of hoteling services (9, 32). Shirzadi et al. showed that human factors were among the most important items affecting the quality of hoteling services from experts’ perspectives (33), which was consistent with our findings. In the study of Han et al., sociality was identified as one of the dimensions of environmental quality in health facilities in Korea (10). The hospital staff’s positive and friendly interactions can reduce patients’ stress and anxiety, create a supportive atmosphere, and ultimately boost patient satisfaction (2). A high level of empathy among health care providers was shown to increase patient satisfaction, resulting in better clinical outcomes and fewer litigation problems (34). Therefore, it is important to maintain and improve care providers’ positive communications and interactions to upgrade patient satisfaction.
Moreover, "physical-structural" and "economic-financial" factors were the most important weaknesses of hospitals in terms of the quality of hoteling services, requiring prompt corrective measures to increase patient satisfaction. The role of the physical environment and atmosphere has been well-documented in increasing patient satisfaction (10, 35). In addition, the physical environment affects the clinical outcome. A study in Iran showed that the quality of hoteling services affected the pain tolerance of patients by about 21% (36). The findings of a national survey in 2017 revealed that inappropriate physical spaces, food’s poor quantity & quality, and lack of accommodations for patients’ companions in hospitals accounted for the main causes of patients’ dissatisfaction with the services provided by public hospitals in Iran (16). In contrast, the study of Zarei et al. on Tehran’s private hospitals in 2012 showed that the least quality gap was related to tangible factors (i.e., a clean environment, new and up-to-date equipment, pleasant physical environment, and convenient accommodations), indicating a small gap between patients’ expectations and perceptions in this aspect of quality (37). This was not consistent with the results of the present study. This difference can reflect the fact that private hospitals focus more on the physical aspects of care and on the tangible and measurable quality dimensions, thereby making their patients happier compared to public hospitals. As mentioned earlier, in Iran’s HTP, attention has been directed toward this aspect of quality (16), and it is expected that hoteling services in public hospitals will be improved and more satisfactory in the future.
In this study, hospitals had poor performance in "economic-financial" factors despite their importance to patients. In this regard, studies carried out in USA and Vietnam showed that the transparency of costs was an organizational priority, requiring careful planning and investment in personnel training and technology. In fact, enhancing patients’ financial communication would increase their satisfaction and loyalty (38, 39). A study in China in 2014 showed that lower medical costs significantly correlated with patients’ satisfaction, and 63% of the patients expressing dissatisfaction with hospital services complained of their high costs (40). By implementing Iran’s HTP and in line with the out-of-pocket (OOP) payment reduction program, a unified bill was designed for patients in public hospitals aiming at clarifying details of costs for patients and insurers, which is expected to improve patient satisfaction (16).
Based on the current study’s findings, "religious-cultural” and "safety-security" factors were less important for patients and, therefore, have low priority for improvement. Despite the fact that hospitals had poor performance in these dimensions, managers should not focus on such areas since they seem to be less important to patients than other aspects of hoteling. So, there is no need to spend more financial or non-financial resources in these areas. A 2016 study on private hospitals in India showed that unlike other aspects of hoteling, upgrading safety and protective services had no effect on patient satisfaction (41), which was in line with the current study’s findings. It seems that unlike other service centers, such as banks, airports, and hotels, facilities such as CCTV cameras, protective equipment, and security forces appear to be less relevant than other factors in hospitals from patients’ perspectives. Despite its lower importance from patients’ perspectives, hospitals are obliged to provide a safe and secure environment for patients (42). Therefore, while maintaining mandatory standards for the safety and security of patients and care providers, safety-security factors did not require more investment to boost patient satisfaction. In addition, there was a low priority for improvement in cultural-religious and safety-security factors despite low patient satisfaction in these dimensions.
The "functional-process" factors were located in the fourth quadrant of the IP matrix, meaning that they were very likely to be overlooked by hospitals. So, patients paid little attention to functional-process factors, but they were relatively satisfied with the hospital’s performance in this dimension. The findings of two previous studies in Iran also showed that patients were highly satisfied with processes such as appointments, admission, and payment (43, 44), which was in line with our study. Unlike other aspects of hoteling services, functional-process factors such as admission, discharge, appointment, and the hospital’s website seem to be less important to patients, which can be due to their less engagement with these items during hospitalization. Hospitals can explain the importance of these factors to patients so that they would appreciate the hospital’s performance in such factors.
The current study had some limitations. First, clinical factors such as disease severity and level of patient care could have affected patients’ judgment about the quality of hospital services, which was not considered in the current study. Second, some patients might have exaggerated the importance of the hoteling services in which they had an unpleasant current or previous experience. In addition, the hoteling services with optimal quality could have been perceived as normal, and therefore, their importance would have been underestimated. An indirect assessment of the importance of hoteling service dimensions can be a subject for subsequent studies.
5.1. Conclusions
As hospitals compete to attract more patients, meeting patient satisfaction and building loyalty are becoming more important than ever. Providing proper hoteling services and meeting patients’ needs, especially in areas identified as weaknesses, are essential and important priorities for hospital managers. Our findings showed a significant gap in all of the six dimensions of hoteling services’ quality, meaning that hospitals’ performance in hoteling services was not proportional to their importance from patients’ viewpoints. In this regard, "physical-structural" and "economic-financial" factors were identified as the main weaknesses, and "human-behavioral" factors as the main strengths of the hospitals studied. Therefore, with regard to the IP matrix’s prioritization, it is essential to pay more attention to the quality and adequacy of physical-structural items, including beds, mattresses, blankets, sheets, pillows, patients’ clothes, wheelchairs, patient transporting stretchers, food, curtains (and all kinds of separators), heating and cooling devices, bathrooms, etc. Providing the necessary information to patients about costs and insurance policies in a manner and language understandable to them at the time of admission and providing a bill with clear details can boost patient satisfaction from the economic-financial standpoint. The human-behavioral dimension was an important area according to patients’ viewpoints, and its requirements can be maintained by healthcare staff’s paying attention to patients’ emotional needs. The confidentiality of patient information and obtaining permission from the patient to start treatment are other important aspects. If hospital managers better understand the roles of hoteling services, they can maximize the positive effects of hoteling service dimensions to build a strong relationship with patients in their hospitals.