1. Background
The prevalence of human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS) is estimated to be 0.2% in the Middle East and North Africa (MENA) region (1). Among them, Iran has a significantly high percentage of people living with HIV (PLWH), the lowest rate of antiretroviral therapy (ART) coverage, and inadequate viral load monitoring (2). Clearly, some barriers, such as a lack of an effective surveillance system, difficulty accessing HIV care facilities, and the complexity of the socio-economic situation in these regions, prevented MENA countries from meeting the 90-90-90 target by 2020, except for a few (2). Obviously, these countries, including Iran, will face the same difficulties in achieving the 95-95-95 global targets until 2030 unless they adopt a new approach and eliminate the significant impediments based on previous experiences (3).
Notably, late HIV diagnosis is highly prevalent in Iran (75.3%) and is associated with sex, age, mode of transmission, and socio-cultural factors such as stigma and illegality of sexual and drug use behaviors (4, 5) Concealment created by Iran’s criminalization of high-risk behaviors has made it challenging to reach people who engage in these behaviors, such as female sex workers (FSW) and injecting drug users (IDUs). According to a population size estimation study, the projected population of FSW in Iran’s 31 provincial capital cities was 130,800 (95% UIs 87,800–168,200) for all urban settings and 228,700 (95% UIs 153,500 - 294,300) for all rural settings (6).
Bordbar et al. found that the total cost of active and passive screening methods was $855.39 and $1528.90, respectively. Their study established that active screening is more cost-effective in aggregate than passive screening (7). Additionally, the mean value of total costs in passive screening method was greater than the active screening method. Moreover, Keshtkaran et al. observed that the costs of intervention (excluding non-IDUs) were less ($204,297.7) than those of non-intervention ($13,942,756.8) (8).
Several HIV service providers have begun to offer more frequent screening to a number of men who have sex with men (MSM) once every three or six months. Early HIV care and adherence to ART prolong life and reduce the risk of HIV transmission (9, 10). Due to the ease with which rapid HIV tests can be obtained, many infections can be detected earlier in the acute stage of infection (11) However, HIV case-finding is mainly passive in Iran based on the national strategic plan. This means that suspected high-risk cases can self-refer to voluntary counseling and testing centers (VCTs); otherwise, healthcare units do not have an active screening program (12).
Noticeably, since 2016, optimized HIV case-finding (OCF) has been introduced and implemented in Ukraine as an effective strategy for developing active case finding (ACF) in drug users. OCF is a case-finding strategy based on respondent-driven sampling, targeting high-risk individuals and their partners. The first step in this approach is to identify as many cases and their partners as possible and provide them with an identification code or coupon to be attached to healthcare units or teams (13). According to the Ukrainian method, when combined with Directly Assisted HIV self-testing (DATS), this strategy has a synergistic effect.
2. Objectives
As a result of the preceding evidence and international experiences, Iran should revise some of its current strategies and strengthen others, focusing on ACF to combat this epidemic. Accordingly, this policy report aimed to shed light on the process of implementing ACF of HIV among high-risk groups in Iran on a nationwide scale.
3. Methods
This policy report is based on the experiences gained during the pilot implementation of first and second phases of OCF program in Iran. From March 2018 to September 2019, the first phase of the OCF program was successfully implemented in Fars, Iran’s fourth most populous province. From November 2020 to May 2021, the second phase of the OCF program expanded coverage to the covered population of eight Iranian universities of medical sciences, including Shiraz, Tehran, Shahid Beheshti, Iran, Alborz, Iranshahr, Abadan, and Chabahar. The OCF program targeted all FSWs and intravenous drug users (IDUs) living in formal or informal settings or on the streets in Iran. The objectives of OCF in this pilot were as follows: (1) to realize more than 95% of high-risk groups’ undercover population venues; (2) to educate more than 95% of those who work in recognized venues; (3) to identify HIV status in more than 95% of high-risk groups at the venues; (4) to provide healthcare to more than 95% of HIV+ individuals identified; (5) to cover the harm reduction program for more than 95% of HIV+ people identified; (6) to assess the prevalence of sexually transmitted infections (STIs) among more than 95% of high-risk groups in the venues; and (7) to register the details of over 95% of high-risk groups in venues.
The second pilot phase was designed to eliminate trial and error during the program’s national implementation. The following steps were taken to conduct the second phase of the OCF program.
3.1. Software Preparedness
A web-based application termed PAS was developed to collect and report on-site data from the target population (PAS is the Persian abbreviation for the software’s name, which translates as ‘monitoring of healthcare services to hard-to-reach groups’).
PAS has the following general characteristics: (1) it provides a foundation for assigning unique identifiers to clients; (2) it electronically inserts services provided at hard-to-reach centers; (3) it monitors and evaluates the provided services; (4) it records the time and place of service in environmental units; (5) it operates data in the referral and follow-up of positive primary cases; (6) it operates data in the referral and follow-up of other cases; (7) it extracts periodic reports for specific geographic areas; (8) it transmits warning messages to ensure service continuity; and (9) it provides analyses and charts based on program indicators.
Table 1 presents the organizational access level to PAS.
| Level | Organizational Level | Types of Possible Units at Each Level | Events at Each Level |
|---|---|---|---|
| 1 | Office of AIDS control in Communicable Disease Management Center | Central Bureau | Information analysis and appropriate managerial measure |
| 2 | University of Medical Sciences | Provincial Health Center | Information analysis and appropriate managerial measure |
| 3 | Health Center of County | Health Center of County | Information analysis and appropriate managerial measure |
| 4 | Behavioral Disease Counseling Center | Behavioral Disease Counseling Center | Receiving referrals from hot spots, environmental units, and service centers |
| 5 | Service providing centers | Drop-in center; Vulnerable Women's Counseling Center; Behavioral Disease Counseling Center | Receiving referrals from hot spots and environmental units |
| 6 | The most peripheral unit of service | Hot spots; drop-in centers; Vulnerable Women's Counseling Center; Health resorts; Comprehensive Health Service Centers | Inserting the client information; Inserting the peripheral service information (screening, prevention, and follow-up) |
3.2. Staff Preparedness
This phase includes training health care professionals who would be involved in the pilot and the mobile team member. To prepare the executive staff, all principals of HIV/AIDS surveillance offices at piloted universities and their county and district counterparts, as well as members of mobile teams, were invited to attend a three-day workshop. The objective of the workshop was to familiarize participants with the pilot plan’s significance and implementation process, geographical mapping method, use of prepared software, and plan monitoring and evaluation (M&E).
3.3. Financing and Logistics
In this regard, the Ministry of Health and Medical Education (MOHME), in collaboration with the World Health Organization (WHO), sponsored the funds to cover the costs of all necessary software and hardware, including tablets for on-site data collection by mobile teams, consumables, such as diagnostic kits, and finally, payment of lecturers’ honoraria.
3.4. Mapping Venues
This phase entails mapping venues frequented by high-risk groups, such as FSWs and IDUs. Geographical mapping is a technique for estimating population size and identifying hotspots and times for target groups. It is used to determine the location of gatherings and the population size of high-risk groups (geographical mapping). This method allows for direct estimation of the size of high-risk populations, gathering places, and hot spot congestion to plan for local and even national programs and plans, and then for the provision of appropriate services based on the type of prevailing behavior in each region.
The pilot plan identified hotspots in three stages according to the size and population of cities, as follows: (1) identifying the primary locations of FSWs in large urban areas using a city map; (2) identifying high-risk areas within the local areas of large cities such as Tehran or Shiraz; and (3) amassing information on hot spots within the specified area from earlier stages.
Finally, key informants and stakeholders compiled a list of hot spots, which included FSWs and other informants, as well as providing features and specifications for hot spots (where the hot spots are located in the city; how these hot spots are accessible; how the hot spot security is). At this point, the map was complete, and the areas were fully segmented. Two separate group discussions were held to elicit information from these individuals and compile a list of hot spots: One with a group of FSWs (based on their species diversity) and another with additional informants not included in the FSW group. At least 12 interviews with key informants from four distinct sources were recommended, including public sector managers and experts, non-public sector managers and experts, the target group [FSWs in various fields], and researchers or professionals working with FSWs.
4. Results
The first and second phases of OCF program successfully reached the target population. The most significant outcome of these phases was that the health system had adequate capacity for nationwide expansion. The results of implementing the second phase are summarized in Table 2. Additionally, it has made significant contributions to HIV management and control, including identifying active hot spots, issuing an anonymous card with a unique barcode to new cases for further follow-up, ensuring the target population’s continuity of screening and care, improving follow-up of reactive diagnostic cases, and establishing monitoring and evaluation (M&E) of the OCF program.
| Pilot Universities | New Registered Venues | Number of New Cases Receiving Services Total (Male/Female) | Registered Services During Pilot | Number of Activated Barcodes |
|---|---|---|---|---|
| Chabahr | 23 | 27 (17/10) | 58 | 63 |
| Abadan | 72 | 201 (126/75) | 1569 | 302 |
| Iran | 21 | 73 (64/9) | 74 | 170 |
| Tehran | 57 | 262 (190/72) | 346 | 1086 |
| Shahid Beheshti | 74 | 116 (72/44) | 121 | 41 |
| Shiraz | 185 | 359 (172/187) | 628 | 834 |
| Iranshahr | 49 | 139 (0/139) | 272 | 233 |
| Alborz | 55 | 105 (48/57) | 188 | 105 |
| Total | 536 | 1282 (689/593) | 3256 | 2834 |
5. Discussion
The OCF program with an active screening strategy has the potential to be scaled up to the entire country, as this pilot plan is being implemented in eight universities with a combined population of approximately 21 million people and diverse socio-cultural contexts. The following sections discuss the proposed steps and strategies.
5.1. Advocacy Plan to Attract Stakeholder’s Support and Cooperation
Given Iran’s diverse socio-cultural context, implementing HIV/AIDS ACF among FSWs or IDUs is challenging. It is necessary to enlist the participation of all stakeholders, including religious leaders, politicians, judiciary officials, community leaders, and non-governmental organizations, to achieve consensus on this sensitive and hidden issue. Achievable goals would include developing an advocacy strategy, conducting a stakeholder analysis, defining roles for each stakeholder, forming a coalition, engaging the media, and sketching a road map (14). Thus, the first step toward extrapolating this plan to the entire country, developing an advocacy strategy, and forming a coalition is necessary.
5.2. Preparedness
Along with the socio-political context, OCF requires the provision of prerequisites such as human resources, software, and hardware. As with the pilot plan, all executive staff at the meso- and micro-levels of HIV/AIDS surveillance and healthcare in the entire country should be trained to become more involved prior to the program initiation. Additionally, as pilot phases approve, existing mobile teams and voluntary counseling and testing (VCT) centers can be assigned to geographical mapping and case-finding throughout all identified high-risk behavior venues, eliminating the need to hire additional staff to run this program throughout the country. Furthermore, the PAS platform was debugged and approved during the pilot’s second phase and is now available for nationwide data collection and reporting. Finally, as mentioned in the method, the mobile teams were equipped with only an electronic tablet for data entry, suggesting that a nationwide expansion of the program would not require as much funding to establish new teams and their equipment.
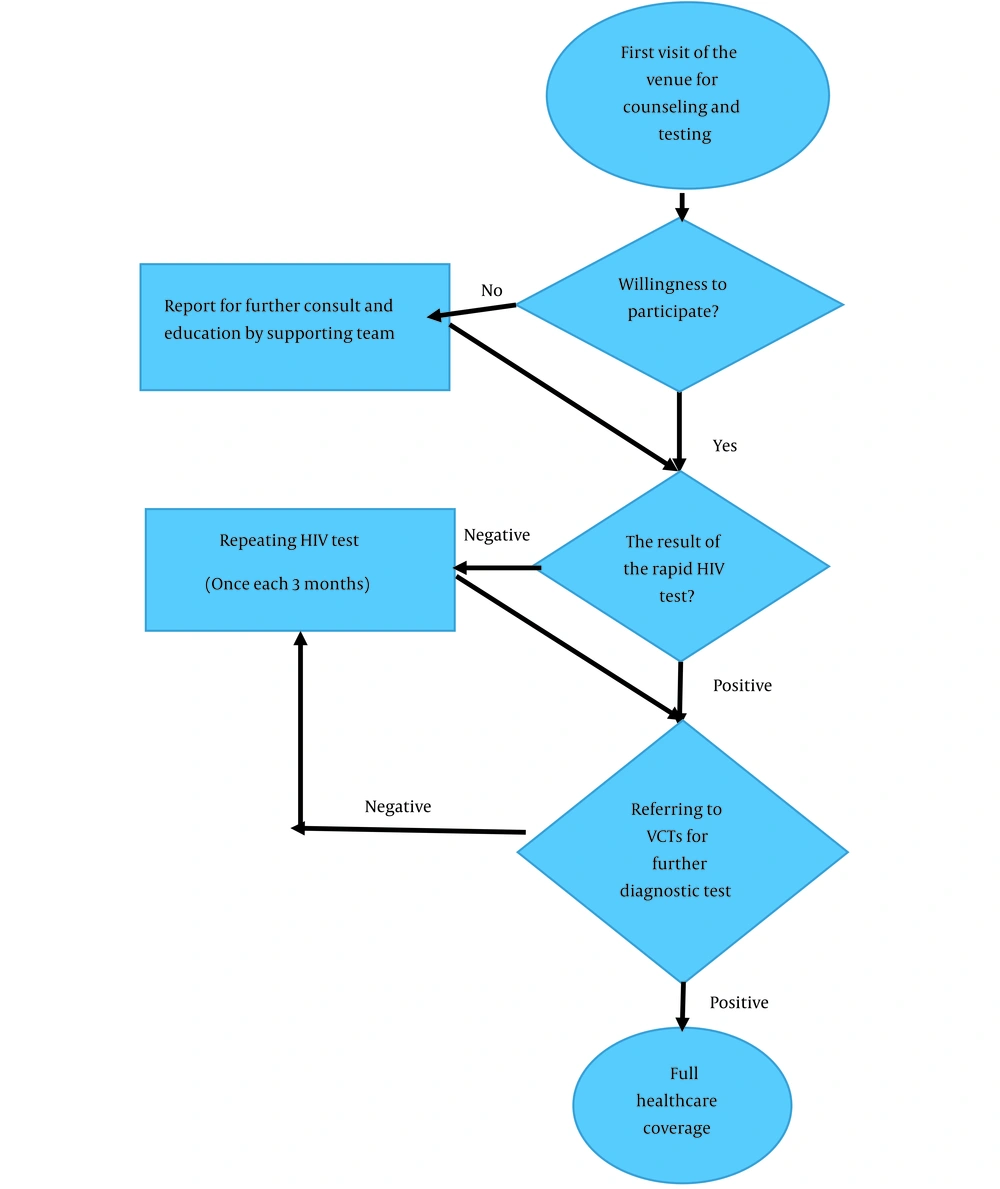
Overall, as we learned from the pilot, extending this project to the entire country will require improving the efficiency of the existing system and a slight increase in financial and other resources. Figure 1 depicts the flow diagram for the ACF process based on the OCF program.
5.3. Multi-intervention Approach
A single intervention should be phased out in favor of a multi-intervention strategy to achieve the 95-95-95 target. This means that relying solely on active screening via mobile teams is insufficient. Evidently, most high-risk behaviors, particularly sex work in Iran, are illegal and concealed (5). Thus, identifying 95% of HIV cases through a single intervention, i.e., ACF in identified hot spots, would not be promising. International evidence indicates that provider-initiated HIV testing and counseling (PITC) and mother-to-child transmission prevention (PMTCT) are two highly effective population-based interventions for case-finding (12, 15). These interventions are included in Iran’s fifth national strategic plan for HIV prevention (7, 16), but they should be strengthened. Iran’s invaluable health network system effectively enables health policymakers to improve PITC and PMTCT (17).
The other intervention that should be combined with the preceding one is increasing the general population’s health literacy regarding HIV/AIDS prevention, emphasizing at-risk and high-risk groups. According to previous studies, Iranians of all social classes lacked sufficient knowledge about HIV/AIDS prevention (18, 19). Unfortunately, socio-cultural factors are the primary impediments to communicating with people in Iran about HIV transmission routes and prevention (16). As mentioned, it is recommended that this issue be addressed through an advocacy strategy.
5.4. Monitoring and Evaluation
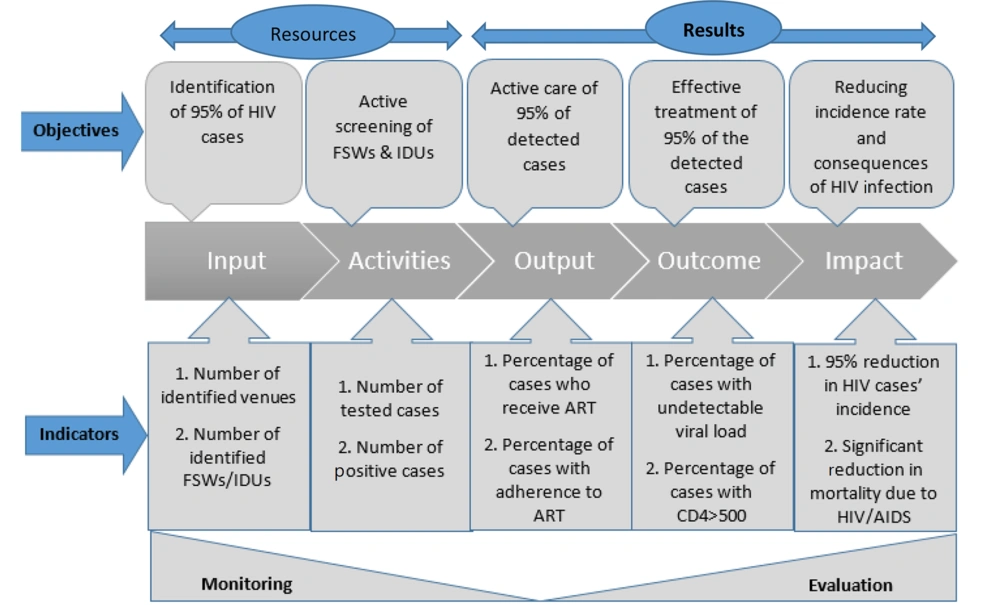
Regardless of the domain or nature of the program, the M&E plan is a required component. The project’s M&E system was designed and implemented during the pilot phase. This plan established supervisors at the national and sub-national levels and reporting systems, forms, and a feedback loop (Figure 2).
5.5. Conclusions
Evidently, OCF requires a multi-strategy approach, and ACF alone cannot guarantee this goal. Thus, current strategies such as increasing general population health literacy and PITC must be strengthened. The other critical issue is gaining the support and cooperation of stakeholders through a comprehensive advocacy strategy. Additionally, it is recommended to equip VCT centers and other components of HIV surveillance systems, as well as train and motivate their staff to ensure that their services are as efficient as possible. Finally, it is also essential to establish an inclusive M&E system based on the lessons learned during the pilot phase.