1. Background
Vaginitis is the most common reason for women of reproductive age to visit medical centers, so it receives 10 million visits every year (1, 2). Candida albicans is one of the most important human pathogenic yeasts and the most common species in the vagina of 20 - 50% of healthy women (3, 4). It can be claimed that at least 75% of women have been infected at least once in their lives, and 40 - 50% of cases experience recurrence. Candida vulvovaginitis severely affects the quality of life of patients and causes a waste of time and high costs for treatment and consequently causes a lot of stress in patients (5, 6). Prolonged treatment and indiscriminate use of antifungal drugs are the most important factors in the isolation of candida isolate from patients with chronic vulvovaginitis compared to common azole drugs (7-9). In recent years, the use of medicinal plants has increased due to the lower side effects and costs and patients’ adaptation to these drugs and in terms of known side effects and resistance to chemical drugs (10-12).
Cinnamon belongs to the Lauraceae and dark-leaf family, which has been approved as herbal medicine by the Food and Drug Administration (FDA). This plant contains protein, fiber, minerals, selenium, calcium, iron, phosphorus, potassium, vitamins A, B, and C, cinnamic aldehyde, eugenol, tannin, amidone, saferol, and cinnamyl acetate (13-15). Cinnamon aldehyde, the active ingredient in cinnamon, has an anti-inflammatory effect and inhibits COX-32, a proinflammation (16, 17). Some laboratory and animal studies indicate that cinnamon bark and its essential oil strongly inhibit fungi and can be introduced as a drug of choice in some fungal species, such as C. albicans (18-20). The lack of human studies on the use of cinnamon in the clinic, especially female fungal infections and controversy in the safety and efficacy of this plant, and knowing that there is a strong tendency to use herbs, have led the research team to plan the study to investigate the effectiveness of cinnamon capsules in women’s vaginitis in comparison to clotrimazole vaginal cream.
2. Methods
The present study is a double-blind clinical trial study, which was carried out from April to August 2014 in Tehran, Iran. This study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences, number PHARMACY.SBMU1392, and registered in the Clinical Trials Center, number IRCT201206104317N7. Besides, the ethical considerations were applied according to the revised Helsinki Statement 2013 (21).
Sampling in this study was purposive firstly, and encompassed all women who were referred to the selected health centers (8 centers) at the time of the study with a diagnosis of vaginitis. The inclusion criteria were those who married with the age range of 15 - 45 years; not being in pregnancy, breastfeeding, or prematurely menopausal periods; no abnormal vaginal bleeding and chronic diseases; no history of taking antibiotics in the last 2 weeks; not using birth control pills or IUDs; not using herbal or chemical medicines to treat vaginitis in the last 2 weeks; and no allergy to herbal medicines. Exclusion criteria were drug-related allergies or illnesses, not taking more than 1 dose of the drug, and having sex without a condom during the treatment. For any reason, no willingness to continue the treatment. Sample size in this study was calculated by mean differences formula, power of test 0.90 and effect size 0.60, type 1 error 0.05; finally, 60 patients were determined for each group (13).
A questionnaire of personal and midwifery characteristics and a checklist for recording vaginitis signs were made by a researcher based on referenced documents and different articles. Content validity of the instruments was done by 15 professors of Midwifery and Reproductive Health, Pharmacy, and Laboratory Sciences at Shahid Beheshti University of Medical Sciences. Reliability tests are not indicated for demographic questionnaires and this type of checklist. Women who met the inclusion criteria completed a questionnaire and a checklist. The sterile speculum was then placed in the vagina without impregnation with a substance to confirm the presence of a candidate infection. A sample of secretions from the upper part of the vaginal wall was then removed with 3 sterile cotton swabs. The first swap was applied to the slide by adding normal saline. To examine the secretions for fungal elements, 10% potassium hydroxide was poured on the second slide and the second swab was drawn on it. Both slides were examined under a microscope (Nikon-Japan) with a magnification of 10 - 40 X. If key cells or flagellate parasites were observed on the first slide, they were diagnosed with Gardenela or Trichomonas and prescribed appropriate treatment by a gynecologist. If blastopores mycelium was observed on the second slide, the presence of Candida was confirmed. If the smear was positive for Candida, pH paper (Merck KGaA, 64271 Darmstadt, Germany) was used. If the pH was 4 - 4.5, it was recorded as a positive candidate and if the pH was high due to mixed infection, it was excluded from the study, and appropriate treatment was prescribed. If the smear is positive for Candida, for the final diagnosis of the third swab, it is transferred to Cio dextrose agar (Dandurand 2331, Montreal, Canada H5G 3C5) and sent by the researcher to the hospital laboratory. The samples were incubated at a temperature of 30 - 37°C, and the formed colonies were evaluated by a laboratory doctor after 48 - 72 hours. Samples for which this diagnosis was finalized (more than 10 colonies per sterile swap) were coded as definitive samples and entered into the study after approval by a gynecologist. Then, the coded subjects were randomly allocated to 2 groups: Clotrimazole and placebo capsule; and clotrimazole with oral cinnamon capsule by the researcher using excel software (random digit table).
Cinnamon capsules in this study were prepared by a pharmacognosist in the laboratory of the Faculty of Pharmacy of Shahid Beheshti University of Medical Sciences in Tehran in the form of 500 mg capsules. The researcher instructed the samples to consume 2.5 g daily (1 g in the morning, 1 g at noon, and 0.5 g at night) for 7 days. The placebo capsule containing 500 mg of starch was prepared in the same color and shape as the cinnamon capsule, and cinnamon was prescribed in the same way. Because of the inherent aroma of cinnamon capsules, placebo capsules were placed next to them so that they could not be detected. Capsules were packed by a pharmacognosist at box A and B separately, and then according to random numbering, allocated to each group. For randomized allocating participants to groups, a random digit table was used by excel software. Consumption of 1 applicator of clotrimazole 1% vaginal cream (10 μg/mL), made by Behvarzan company, was prescribed for both groups every night for a week. The researcher asked all the samples to come to the clinic on the 7th day and 2nd month after the treatment to complete the checklist by the gynecologist and researcher.
All participants had to have a vaginal smear for microscopic examination before treatment, and 7th day after treatment. The researcher asked all the samples about the side effects of taking the drug. All samples were given medication instructions orally, and health advice was given. The participants were advised to refrain from condom-free intercourse, vaginal douches, other vaginal medications, and antibiotics while taking the medication. Otherwise, they would be excluded from the study. If left untreated, the patient would be referred to a gynecologist. It should be noted that telephone access to the researcher and gynecologist was possible for all samples during the study. This clinical trial was double-blinded, so neither researcher nor the samples knew what kind of treatment was prescribed for them.
2.1. Statistical Analysis
For descriptive and analytic statistical analysis, SPSS version 21 was used. t-test, Cochran’s Q test, chi-square (χ2), or Fisher’s exact test were used to compare intergroup changes, and McNemar test was used to compare intragroup changes. P-value < 0.05 was considered statistically significant.
3. Results
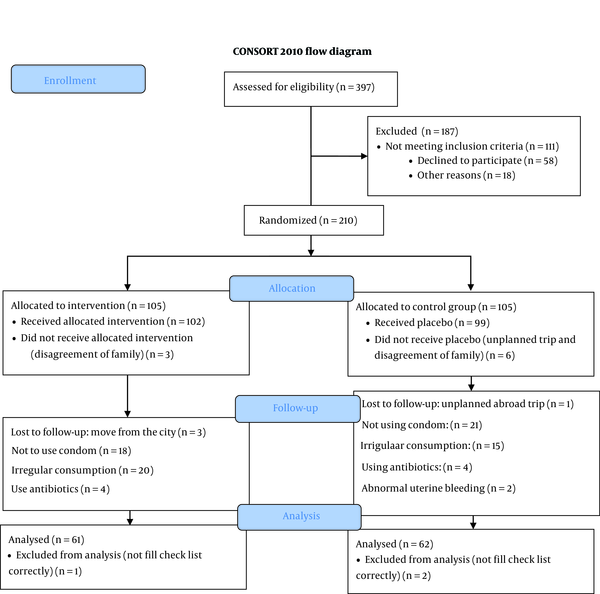
The present study was performed on 120 women with candidal vaginitis referred to the selected health center of Shahid Beheshti University of Medical Sciences. The consort flow chart describes the status of the sampling process, briefly 397 participants registered at first, and 187 women were excluded (because of not meeting inclusion criteria, no willingness, and other reasons), 210 women were allocated to each group, and according to the flow chart finally, 120 women were analyzed (Figure 1). The two groups were similar in terms of demographic characteristics, but not in spouse education, occupation, and income (Table 1). In fact, economic status was better in the cinnamon group (P = 0.011).
| Variables | Cinnamon and Clotrimazole Group (n = 60) | Placebo and Clotrimazole Group (n = 60) | P-Value |
|---|---|---|---|
| Age | 30.7 ± 6.6 | 31.16 ± 8.2 | 0.61 b |
| Body mass index | 19.25 ± 3.9 | 24.86 ± 4.4 | 0.45 b |
| Gravidity | 1.1 ± 0.25 | 1.1 ± 0.32 | 0.68 c |
| Number of children | 1.30 ± 1.01 | 1.40 ± 1.41 | 0.45 c |
| Education | 0.42 c | ||
| Elementary | 7 (11.6) | 14 (23.4) | |
| High school | 45 (75) | 36 (60) | |
| Academic | 8 (13.4) | 10 (16.6) | |
| Husband’s education | 0.002 c, d | ||
| Elementary | 5 (8.3) | 15 (25) | |
| High school | 41 (68.3) | 39 (65) | |
| Academic | 14 (23.4) | 6 (10) | |
| Job | 0.95 e | ||
| Housewife | 48 (80) | 46 (76.6) | |
| Employee | 6 (10) | 7 (11.4) | |
| Worker | 2 (3.3) | 2 (3.5) | |
| Self -employment | 4 (6.7) | 5 (8.5) | |
| Husband’s job | 0.001 e, d | ||
| Retired /not unemployed | 2 (3.3) | 2 (3.3) | |
| Employed | 26 (43.3) | 9 (15.1) | |
| Worker | 9 (15) | 25 (41.6) | |
| Self-employed | 23 (38.4) | 24 (40) | |
| House status | 0.33 e | ||
| Rental | 37 (61.6) | 42 (70) | |
| Private | 23 (38.4) | 18 (30) | |
| Income | 0.011 c, d | ||
| Low income | 40 (66.6) | 52 (87) | |
| Middle | 18 (30) | 7 (11.4) | |
| Appropriate | 2 (3.34) | 1 (1.6) |
Demographic Characteristics of Samples in the Cinnamon and Placebo Groups a
Mann Whitney and chi-square tests also showed that interfering variables such as the number of intercourse per week (P-value = 0.084), methods of pregnancy prevention (P-value = 0.181), use of tight underwear and pants (P-value = 0.358), use of cotton underwear (P-value = 0.831), wet underwear (P-value = 0.256), use of pool (P-value = 0.509), bathtub and public bath (P-value = 0.408) are also the same in 2 groups.
Table 2 shows the frequency distribution of signs and symptoms in the pre-treatment evaluation in the cinnamon and placebo groups. Distribution of discharge in the cinnamon group vs. the placebo group was 51% vs. 47% (P = 0.345), itching 50% vs. 54% (P = 0.283), burning 43% vs. 49% (P = 0.195), dyspareunia 48% vs. 47% (P = 0.822), suprapubic pain 39% vs. 41% (P = 0.699), and dysuria 26% vs. 25% (P = 0.853). Chi-square test between the two groups showed no significant differences in symptoms and signs.
| Symptoms | Cinnamon and Clotrimazole Group | Placebo and Clotrimazole Group | Chi-square Test |
|---|---|---|---|
| Vaginal discharge | 0.345 | ||
| Yes | 51 (85) | 47 (78.3) | |
| No | 9 (15) | 13 (21.7) | |
| Itching | 0.283 | ||
| Yes | 50 (83.3) | 54 (90) | |
| No | 10 (16.7) | 6 (10) | |
| Burning | 0.195 | ||
| Yes | 43 (71.7) | 49 (81.7) | |
| No | 17 (28.3) | 11 (18.3) | |
| Dyspareunia | 0.822 | ||
| Yes | 48 (80) | 47 (78.3) | |
| No | 12 (20) | 13 (21.7) | |
| Suprapubic pain | 0.699 | ||
| Yes | 39 (65) | 41 (68.3) | |
| No | 21 (35) | 19 (31.7) | |
| Dysuria | 0.853 | ||
| Yes | 25 (41.7) | 26 (43.3) | |
| No | 35 (58.3) | 34 (56.7) |
Frequency of Signs and Symptoms of the Disease in Pre-treatment Evaluation in the Cinnamon and Placebo Group a
According to McNemar’s test (Table 3), significant treatment effects in the cinnamon group began on the 4th day and remained until 2 months later (P < 0.001). However, vaginal discharge treatment occurred on the 7th day (p < 0.001). In the placebo group, itching and burning decreased significantly on days 4th and 7th (P < 0.001), and vaginal discharge increased significantly on day 4th (P = 0.001). Dyspareunia (P < 0.001), dysuria (P = 0.02), and suprapubic pain (P = 0.001) decreased on day 7th, and all signs and symptoms of vaginitis recurred 2 months after follow-up.
| Groups | Symptoms | |||||
|---|---|---|---|---|---|---|
| Vaginal Discharge | Itching | Burning | Dyspareunia | Sup-pubic Pain | Dysuria | |
| Cinnamon | ||||||
| Before treatment | 51 (85) | 50 (83.3) | 43 (71.7) | 48 (80) | 39 (65) | 25 (41.7) |
| 4th day | 59 (93) | 34 (56.7) | 29 (48.3) | 8 (13.3) | 5 (8.3) | 8 (13.3) |
| P-value | 0.008 | < 0.001 | 0.001 | < 0.001 | < 0.001 | < 0.001 |
| 7th day | 25 (41.7) | 7 (11.7) | 3 (5) | 1 (1.7) | 2 (3.3) | 3 (5) |
| P-value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| 2 months later | 31 (51.7) | 19 (31.7) | 41 (25.7) | 18 (30) | 18 (30) | 17 (28.3) |
| P-value | < 0.001 | < 0.001 | < 0.003 | < 0.001 | < 0.001 | 0.02 |
| Placebo | ||||||
| Before treatment | 47 (78.3) | 54 (90) | 49 (81.7) | 47 (78.3) | 41 (68.3) | 26 (43.3) |
| 4th day | 60 (100) | 43 (71.7) | 28 (46.7) | 43 (71.7) | 36 (60) | 26 (43.3) |
| P-value | 0.001 | 0.001 | < 0.001 | 0.125 | 0.125 | 0.11 |
| 7th day | 38 (63.3) | 12 (20) | 5 (8.3) | 21 (35) | 10 (16.7) | 16 (26.7) |
| P-value | 0.108 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | 0.021 |
| 2 months later | 43 (71.7) | 40 (66.7) | 43 (71.7) | 34 (56.7) | 36 (60) | 38 (63.3) |
| P-value | 0.481 | 0.06 | 0.28 | 0.06 | 0.458 | 0.53 |
Comparison of Pre-treatment Symptoms in the Two Groups Days 4th,7th, and 2 Months Later a
The results of the Cochran’s Q test for comparing the ratio of positive cultures and positive wet smears in the two groups were statistically significant. Comparison of positive wet smears before treatment and the 7th day, from 100% to 14% (P < 0.001) in the cinnamon group and from 100% to 42% (P < 0.001) in the placebo group, showed a significant decrease. Positive culture before treatment (100%) was reduced to 28% in the cinnamon group (P < 0.001) and from 100% was reduced to 66% in the placebo group (P < 0.001). Although a positive effect was observed in both groups, in the comparison between the two chi-square test groups, it was shown that cinnamon and clotrimazole had a greater effect on negative culture and wet smear than placebo and clotrimazole (P < 0.002).
Examination of signs and symptoms 2 months after the treatment in the two groups of cinnamon and clotrimazole (Table 4) showed that no recurrence occurred in 55% of the patient in the cinnamon group and 28.3% of the patient in the placebo group. Based on the chi-square test, there was a significant difference in terms of improvement of signs and symptoms in the two treatment groups, and the cinnamon group showed more effectiveness than the placebo group.
| Cinnamon Group | Placebo Group | Chi-square | P-Value | |
|---|---|---|---|---|
| No recurrence after 2 months | 33 (55) | 17 (28.3) | 8.77 | 0.003 |
| Recurrence after 2 months | 27 (45) | 43 (71.7) | ||
| Total | 60 (100) | 60 (100) |
Comparison of the Frequency of Candidal Vaginitis Recurrence 2 Months After the Treatment in the Cinnamon and Placebo Groups a
4. Discussion
This study examined oral cinnamon capsules on candidal vaginitis, and the results indicate that this herbal medicine is effective in improving recurring candidal vaginitis compared to its common treatment. This study showed that the signs and symptoms significantly improved from the 4th day and after completing the treatment and even 2 months later. The effect of oral cinnamon and clotrimazole cream was better than placebo and clotrimazole craemregarding vaginitis recurrence.
In this study, vaginal discharge, which is the complaint of the majority of patients in the cinnamon and placebo groups, significantly increased on the 4th day, which is expected to occur due to clotrimazole cream in both groups. But discharge significantly decreased after completing the treatment (7th day) and the recurrence period (2 months later). These findings are consistent with the results of a study in Iran, which examined the effect of honey cinnamon cream in comparison to clotrimazole on the treatment of vaginitis symptoms. They showed that the effect of honey cinnamon vaginal creamon vaginal discharge was better than clotrimazole cream alone (13). Another study, which determined the effect of ginger cream on candidate vaginitis, found that the effectiveness of ginger cream was equal to clotrimazole in reducing the candidate discharge (22).
In this study, pruritus and burning were significantly improved in the two groups from the 4th day, and this improvement was evident in both groups until the end of the treatment, but the improvement persisted in the cinnamon group after a two-month follow-up. Julianti et al. showed that the composition of cinnamon honey had anti-inflammatory and antifungal effects on acne-causing bacteria and acted as a long-acting antibiotic (23). Cinnamon also inhibits nitric oxide due to its cinnamaldehyde and has an anti-inflammatory effect (23). A study conducted in 2018 showed no difference in treatment results between the two groups of dill cream and clotrimazole (24).
Reports of dyspareunia and suprapubic pain in the cinnamon group revealed improvement from the fourth day and continued for a two-month follow-up. However, this improvement was significant in the placebo group just after completing the 7th day of the treatment. The main anti-inflammatory ingredients of cinnamon are its high polyphenols and protein C, which is a marker of inflammation. Cinnamon consumption reduces inflammation in the body (25). Khosravi et al. investigated the effect of cinnamon on symptoms of suprapubic pain and dysuria of vaginitis (26). They believed that complete improvement of symptoms was due to the anti-inflammatory effects of this plant (26).
Dysuria showed improvement in the cinnamon group from the 4th day until 2 months later, while the only improvement was observed in the placebo group at the time of completion of treatment (7th day). Contrary to this study, Rasooli et al. did not find any positive effect on the use of honey cinnamon cream to improve urinary symptoms (13). The improving effects of cinnamon and placebo on positive cultures and positive wet smears were reported after completion of the optimal treatment period. Notably, recurrence is significantly lower in the cinnamon group than in the placebo group. In this regard, the study of Fouladi et al. is similar to the results of the present study (27). Their study reported negative cultures in 100% of patients in the clotrimazole group and 97.3% of the thyme cream group after the treatment (27).
Microscopic evaluation and culture of secretions before and after the treatment in the case of edible plants, garlic oil, and green tea compared to clotrimazole also showed a decrease in positive cases, indicating that both acted equally. However, recurrence rates were not studied in these studies (28, 29). The results of the study of Atai et al. also showed that cinnamon, turmeric, wormwood, sage, mint, marigold, and onion all have antifungal properties against Candida albicans compared to nystatin mouthwash (30). They concluded that cinnamon extract with a dilution of 1.5 prevented the growth of fungi, and even with this dilution had lethal properties (30).
The strengths points of the present study include having a control group, double-blindness, placebo administration, random assignment, determination and control of interfering variables, review of samples and laboratory cultures by 1 person, precise control, and the reliability and validity of the tools. Starting to evaluate the recovery process from the 4th day and following up the recurrence of the infection after 2 months are also other unique features of the present study that are not seen in other studies. Also, despite providing the necessary training on how to use the drug and observing health tips to research patients, the possibility of non-compliance with health standards should be considered.
4.1. Conclusions
Community-based midwifery has a great role in using the latest scientific achievements in the world to promote women’s health. Paying attention to herbs such as cinnamon for improving the symptoms of vaginitis may be an acceptable and effective way to meet the health needs of women.