1. Background
According to reports, around 284 million 15 - 64-year-old people used drugs worldwide in 2020, showing a 26% increase over the previous decade. Men used drugs three times more than women (1, 2). Among the various forms of drug use, drug injection is a global and regional problem (3).
In countries located in the Middle East and North Africa, including Iran, 0.2% of the population inject drugs (4). Over the past few years, the number of these people has grown significantly in some areas, which is assumed to be due to the globalization of illegal drug trades (5, 6). For example, from 1995 to 2005, the number of injecting drug users (IDUs) increased from zero to 124,000 - 196,000, 43,000 of whom developed AIDS (acquired immunodeficiency syndrome) up until the end of 2005. There is a similar situation in other South East Asian countries, where addiction related to intravenous drug abuse shared an important role in the AIDS epidemic in those areas (3, 7).
In this regard, harm-reducing programs, especially the needle and syringe program (NSP), are among the important priorities for health researchers and officials in different countries. These studies, often conducted with a cost-effective strategy, provide important information resources to health policymakers. However, the evaluation of the NSP is regarded as a quite complicated task to be accomplished (1, 8). Various studies in the world indicate the importance of this issue in different countries. Many factors, including environmental and social conditions and national policies in every country, affect the implementation of such programs, so the results of a study conducted in a specific country should be generalized to other countries with caution (9, 10).
There are different indicators, such as behavior change (i.e., a reduction in co-injection and lending and borrowing syringes), to evaluate the effectiveness of syringe distribution programs (11, 12). Researchers have affirmed the effectiveness of syringe and needle distribution programs in reducing high-risk behaviors and the occurrence of HIV (13). However, these studies are generally limited to high-income countries, and some studies have been conducted in low- and middle-income countries, such as Nepal, India, and Vietnam, only in recent years (14). Contradictory findings in the studies conducted in various countries have encouraged researchers in many countries to accurately assess the effectiveness of such programs and nurture appropriate grounds and views before launching them.
Drug abuse has a prolonged history in Iran due to its close and long borders with Afghanistan. Recently, easy access to heroin and fluctuations in opium prices have increased the tendency of users to choose heroin, leading to an increase in IDUs in Iran (15, 16). The reduction in the age of onset of drug abuse and the high prevalence of IDUs have made addiction an important cause of social harm in Iran (17). This form of drug abuse has grown significantly in the last decade due to its secrecy, cheapness, and short time required for its effects. In a study assessing drug abuse status in the country in 2007, about 18% of drug users reported that injection was their dominant method of drug use, and 26% reported drug injections within the last year (18, 19). Estimations indicated that there were 200 - 300 thousand IDUs in Iran in 2001, which was estimated to rise to approximately 400 thousand in 2007 (15, 20). Injecting drug users show a variety of high-risk behaviors that can be divided into two main categories. The first category includes substance-related behaviors such as co-injection or sharing syringes and needles, and the second category encompasses unprotected sexual behaviors (21), exposing these individuals to the risk of a variety of infectious diseases, including HIV and hepatitis B and C infections.
3. Methods
This was an interventional study with a before-after design. The intervention included training on different ways of low-risk injection, methods of the sterilization of injection devices, reducing the risks associated with drug abuse and sexual behaviors, counseling and testing for HIV and hepatitis B virus infection, distributing sterile syringes, needles, cotton, alcohol, and condoms, offering methadone maintenance treatment, gathering and discarding contaminated syringes and needles, and patient referral to specialized medical centers.
This study was conducted in two drop-in centers (DICs) in Hamadan City in 2020 - 2021. The statistical population included injecting and non-injecting drug users referring to these DIC centers in Hamadan.
The research protocol was approved by the Ethics Committee of Hamadan University of Medical Sciences, Iran, under code IR.UMSHA.REC.1398.304.
A questionnaire enclosing contextual variables and variables related to the effectiveness of the interventional program was used to collect data. The following measures were performed to improve the quality and accuracy of the data collected:
To eliminate possible problems with data collection tools, as well as administrative problems, a pilot study was primarily conducted. During this phase, researchers surveyed 30 people and performed all the steps of data collection to become acquainted with the details of the data collection procedure. The validity and reliability of the instrument were also assessed.
The preliminary study showed that Cronbach’s alpha between the items of the different sections of the questionnaire was above 0.7. The content validity of the questionnaire was confirmed by three experts, and the structural validity of the questionnaire was determined using principal component analysis, which showed that in each section of the questionnaire, the first and second factors extracted explained 80% of the total variance of the variables.
All 188 volunteers, including IDUs and non-injecting drug users (NIDUs) who received services in the two DICs of Hamadan City, were included in the study. Informed consent was obtained from all the participants.
Data analysis was performed in three steps:
Step 1: Analysis of the survey data to calculate the frequency and ratio of high-risk behaviors among the subjects.
Step 2: Assessment of the accuracy of self-reported high-risk behaviors (i.e., injection via a common syringe).
Step 3: Analysis of the program’s effectiveness by comparing the frequency of high-risk behaviors before and after the intervention over a specified period.
Descriptive statistics used to present quantitative variables included mean, and standard deviation, and absolute and relative frequencies were used for ranked and classified data. Inferential analyses for high-risk behaviors before and after the intervention were performed through the tests related to paired data.
4. Results
A total of 188 people participated in this study, of whom 112 (59.6%) were male, and 76 (40.4%) were female. The mean ± standard deviation of their age was 47.72 ± 10.88 years. Table 1 shows the central and dispersion parameters of the quantitative variables assessed in this study.
| Variables | Statistical Indicators | |||||
|---|---|---|---|---|---|---|
| Mean | Standard Deviation | Median | Mode | Minimum | Maximum | |
| Monthly income (Tomans) | 1257735 | 114550 | 900000 | 1000000 | 42000 | 7000000 |
| The monthly payment for drugs (Tomans) | 805952 | 850733 | 500000 | 51000 | 5500 | 400000 |
| Age of onset of substance use | 22.4 | 5.6 | 19.00 | 21.00 | 14.00 | 38.00 |
| Age of onset of injecting drugs | 24.6 | 6.3 | 25.00 | 22.00 | 15.00 | 38.00 |
| Number of injections per day | 3.1 | 1.3 | 3.00 | 3.00 | 1.00 | 6.00 |
| Number of injection partners | 3.1 | 1.4 | 3.00 | 3.00 | 1.00 | 8.00 |
| Frequency of imprisonment | 5.4 | 2.6 | 4.0 | 1 | 1 | 10 |
| Duration of imprisonment (mo) | 18.1 | 4.6 | 3 | 3 | 1 | 216 |
Overall, 67% of the subjects had a history of injecting drugs, of whom 22.3% had co-injections. Also, 46.3% of the people admitted to the DICs had sexual intercourse with individuals other than their spouses, and only 36.2% of them used condoms. Table 2 shows the absolute and relative frequencies of the subjects’ demographic variables.
| Variables | No. (%) |
|---|---|
| Education | |
| Illiterate | 35 (18.6) |
| Elementary | 40 (21.3) |
| Senior high school | 60 (31.9) |
| Diploma | 40 (21.3) |
| Above diploma | 7 (3.7) |
| Bachelor | 6 (3.2) |
| Job | |
| Worker | 25 (13.3) |
| Sex worker | 62 (33.00) |
| Waste collector | 21 (11.2) |
| Unemployed | 16 (8.5) |
| Businessman | 45 (23.9) |
| Housewife | 1 (0.5) |
| Farmer | 4 (2.1) |
| Other | 14 (7.4) |
| Place of drug use | |
| Inside prison | 20 (10.6) |
| Outside prison | 118 (62.8) |
| Home | 22 (11.7) |
| Unknown | 28 (14.9) |
| Substance | |
| Opium and its juice | 41 (21.8) |
| Heroin | 111 (59.00) |
| Crack | 1 (0.5) |
| Norchizek | 1 (0.5) |
| Methadone | 10 (5.3) |
| Opium syrup | 1 (0.5) |
| Cannabis | 13 (6.9) |
| Methamphetamine | 10 (5.3) |
| Substance injecting | |
| Yes | 126 (67.00) |
| No | 45 (23.9) |
| Unknown | 17 (9.00) |
| Type of syringe | |
| New syringe | 90 (47.9) |
| The syringe already used by the person | 25 (13.3) |
| Syringe already used by another person | 29 (15.4) |
| The syringe was found on the ground | 3 (1.6) |
| Unknown | 41 (21.8) |
| Joint injection | |
| Yes | 42 (22.3) |
| No | 104 (55.3) |
| Unknown | 42 (22.3) |
| History of imprisonment | |
| Yes | 121 (64.4) |
| No | 60 (31.9) |
| Unknown | 7 (3.7) |
| Sex with a person other than the spouse | |
| Yes | 87 (46.3) |
| No | 87 (46.3) |
| Unknown | 14 (7.4) |
| Using condoms | |
| Yes | 68 (36.2) |
| No | 73 (38.8) |
| Unknown | 47 (25.00 |
| HIVtest | |
| Yes | 172 (91.5) |
| No | 16 (8.5) |
| HIV test result | |
| Positive | 11 (5.9) |
| Negative | 160 (85.1) |
| Unknown | 17 (9.00) |
| Place of injecting drugs | |
| Personal home | 84 (44.7) |
| Public places | 59 (31.4) |
| Prison | 3 (1.6) |
| DIC centers | 2 (1.00) |
| Unknown | 40 (21.3) |
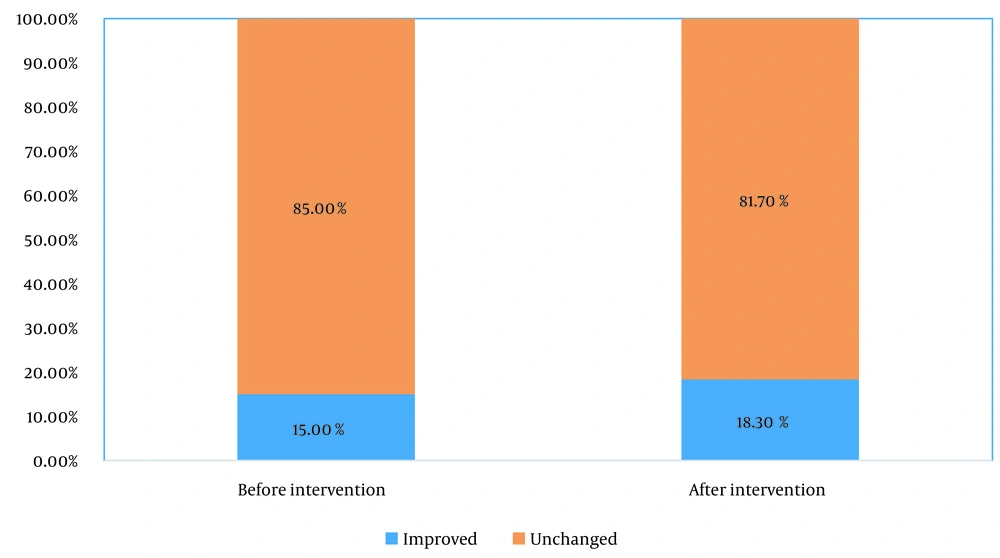
Table 3 shows the proportion of NIDUs before and after the intervention (i.e., harm-reduction programs at DICs). McNemar’s test showed that the difference between the proportion of NIDUs before admission to DIC centers and two months after discharge from these centers was statistically significant (P = 0.03), showing a decrease from 85% to 81.7 % after the intervention.
| After Intervention | Sum | P | OR | %95 CI OR | ||
|---|---|---|---|---|---|---|
| Unchanged | Improved | |||||
| Before intervention | 0.031 | 0.04 | 0.2 - 0.9 | |||
| Unchanged | 147 (81.7) | 6 (3.3) | 153 (85.00) | |||
| Improved | 0 (0) | 27 (15.00) | 27 (15.00) | |||
| Sum | 147 (81.7) | 33 (18.3) | 180 (100) | |||
a Values are expressed as No. (%).
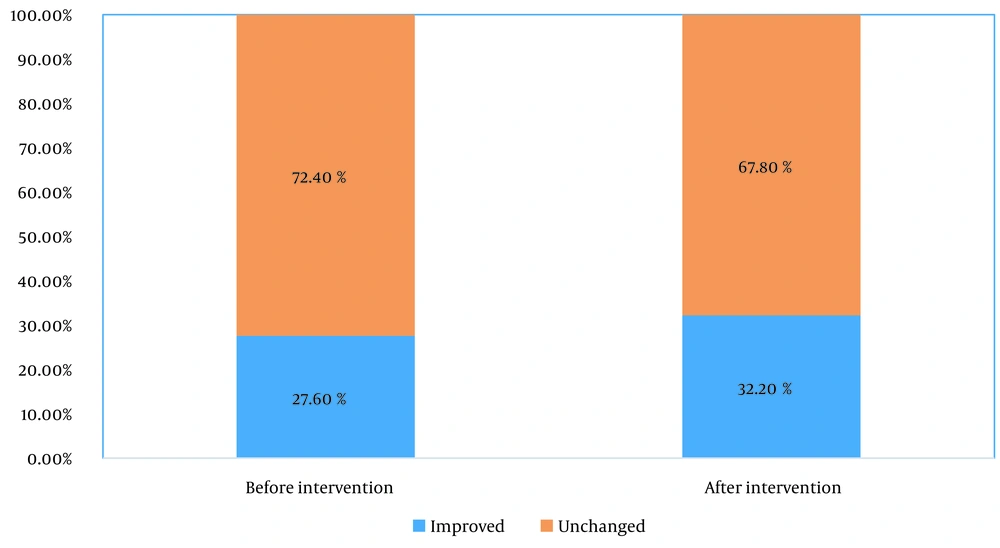
Table 4 shows the ratio of IDUs before and after the intervention (i.e., harm-reduction programs at DICs). McNemar’s test showed that the difference between the proportion of IDUs before admission to the DIC centers and two months after discharge from these centers was statistically significant (P = 0.008), showing a decrease from 72.4% to 67.8 after the intervention.
| After Intervention | Sum | P | OR | %95 CI OR | ||
|---|---|---|---|---|---|---|
| Unchanged | Improved | |||||
| Before intervention | 0.008 | 0.06 | 0.03 - 0.12 | |||
| Unchanged | 118 (67.8) | 8 (4.6) | 126 (72.4) | |||
| Improved | 0 (0) | 48 (27.6) | 48 (27.6) | |||
| Sum | 118 (67.8) | 56 (32.2) | 174 (100) | |||
a Values are expressed as No. (%).
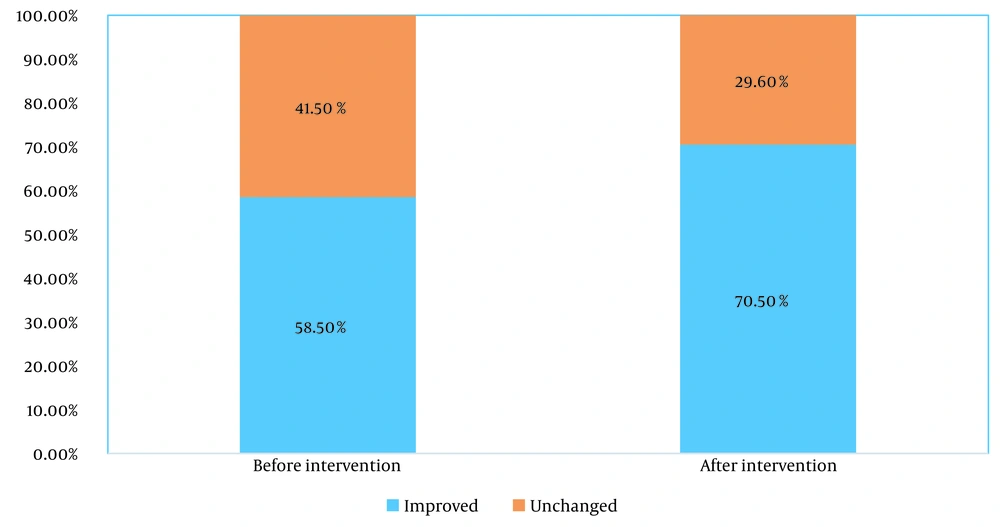
Table 5 shows the ratio of co-injecting drug users before and after the intervention (i.e., harm-reduction programs at DICs). McNemar’s test showed that the difference between the ratios of co-injecting drug users before admission to the DIC centers and two months after discharge from these centers was statistically significant (P < 0.001), indicating a decline from 41.5% to 27.3% after the intervention.
| After Intervention | Sum | P | OR | %95 CI OR | ||
|---|---|---|---|---|---|---|
| Unchanged | Improved | |||||
| Before intervention | 0.001 | 0.35 | 0.26 - 0.49 | |||
| Unchanged | 48 (27.3) | 25 (14.2) | 73 (41.5) | |||
| Improved | 4 (2.3) | 99 (56.3) | 103 (58.5) | |||
| Sum | 52 (29.6) | 124 (70.5) | 176 (100) | |||
a Values are expressed as No. (%).
Figures 1 to 3 compare the effects of the harm-reduction interventional programs on the high-risk behaviors of the participants before and after the intervention (Figures 1 to 3).
5. Discussion
Our results indicated the high prevalence of high-risk behaviors among those referring to DICs in Hamadan City before admission to these centers. This finding was comparable to the results of the National Study of Behavioral-Biological Care in Injecting Drug Consumers conducted in 2010 in Iran, reporting a relatively high prevalence of high-risk behaviors (37% for a history of non-sterile syringe use, 12.6% for co-injection in the last month, and 60% for using no condoms during the most recent sexual intercourse) (22). Therefore, it is important to pay attention to implementing these programs both quantitatively and qualitatively.
The increasing rate of drug addiction, especially among IDUs, and high-risk injections and sexual behaviors have led to a rise in the incidence of HIV in this group (1, 9, 23, 24). Today, the fact that eliminating drug use is not an easy task is accepted as a principle, highlighting the need for implementing harm-reduction programs, especially syringe and needle programs, for IDUs (25). Iran is one of the pioneers of implementing harm-reduction programs in the Middle East and North Africa, and despite its good achievements, some IDUs still continue to engage in high-risk behaviors (10).
Evaluation programs and secondary studies to review and scrutinize these programs can pave the way for evidence-based decision-making and planning by health policymakers. Various studies have been conducted around the world to evaluate the effectiveness and cost-effectiveness of syringe and needle distribution programs, underlining the importance of such programs in different countries. Given that various factors, including environmental and social conditions and national policies in every country, profoundly affect the successful implementation and launching of these programs, the generalization of the results of studies in specific countries to other countries should be made with caution (26). Most of these studies are limited to developed countries; however, developing countries, such as Nepal, India, and Vietnam, have conducted such studies in recent years (27).
Our results also showed a significant reduction in high-risk behaviors such as injecting and having multiple injection partners among the participants of this study. High-risk injection behaviors, as the most important factor affecting HIV transmission, have been evaluated in different studies using different tools (12, 28-33). The results of some of these studies showed that high-risk behaviors were significantly reduced in those who participated in syringe and needle programs (12, 32, 33). In 2006, a study by Vickerman et al. conducted to evaluate the effectiveness of a syringe and needle replacement program, injection-related behaviors were considered as indicators or outcomes, and it was found that participation in this program significantly reduced injection-related high-risk behaviors such as lending and borrowing syringes (13). A study by Islam et al. in 2007 compared two groups of IDUs (participating in the program versus not participating in the program) and indicated that people who participated in the syringe and needle distribution program compared to individuals who did not participate in the program were less likely to perpetrate high-risk behaviors, such as injecting with others’ syringes and lending their syringes to others (34). In contrast, Gibson et al. reported that the syringe-needle program increased high-risk injection behaviors, and the people participating in this program were more likely to inject and share syringes (35). Another study in Amsterdam found that there was an inverse relationship between participating in a syringe distribution program and borrowing a syringe, and this relationship was confirmed in multivariate analysis after controlling potential confounding factors (36). Contradictory findings in different studies could be attributed to selection bias, meaning the selection of people who were more likely to engage in high-risk injection behaviors than others regardless of participating in these programs (20, 37). Few studies have shown that this program has no significant effect on high-risk injection-related behaviors (38).
Moreover, our results showed that the frequency of injections among IDUs was relatively high (an average of three times a day). In a study by Shoghli et al. in Zanjan, the frequency of injection was reported as three times a day on average (39). Studies in the United Kingdom and Russia showed an average frequency of injection of two and three times per day, respectively (40). The frequency of injection is one of the most important determinants of the risk of HIV transmission among IDUs, so this behavior needs prompt attention to promote the health of drug users (41).
The reuse of syringes, although not considered a high-risk behavior associated with HIV, has been frequently studied because it plays an important role in skin infections and cellulite (42, 43). In addition, the reuse of syringes can be an indicator of insufficient access to them (44). Our study showed that the average frequency of reusing a syringe was approximately three times. In Wickerman’s study in the UK, the average frequency of reusing syringes was reported to be 2.5 times. This high-risk behavior can be due to limited access to syringes, the shortage of the syringe and needle distribution program, or other reasons such as high-frequency and overwhelming injections (8).
Due to ethical limitations in conducting a pilot study in this field, all available studies are generally based on observational evaluations about the effectiveness of the program on high-risk injection behaviors, so we cannot claim the accuracy and effectiveness of the program in reducing high-risk behaviors. This is one of the most important challenges in evaluating this program (45). Under-reporting of high-risk behaviors by drug users, especially the shared use of syringes, is another challenge in this area, leading to inaccurate predictions of HIV incidence. Although it has been reported that self-reporting of high-risk behaviors is highly valid among drug users (46), Latkin and Vlahov argued that high-risk drug users, such as co-injectors, tended to underreport such behaviors (20).
The present study, like any other study, had some limitations, including the lack of a cohort of participants and a control group due to logistical restrictions. So, the effectiveness of the intervention was evaluated by comparing high-risk behaviors before and after the harm-reduction program. The results of this study can be extrapolated to other cities and regions in Iran, highlighting the importance of creating more DICs and implementing preventive programs nationwide. Finally, the effectiveness of these programs was investigated only with regard to the incidence of high-risk behaviors.
5.1. Conclusions
Our study, in line with most previous studies in the world, showed that harm-reduction programs in DIC centers, especially the syringe and needle distribution program, had a significant role in reducing the incidence of high-risk behaviors among IDUs. Training programs play an important role in reducing high-risk behaviors, and the effectiveness of such programs can be intensified by addressing a variety of health dimensions, such as HCV prevention. Our results can be beneficial to health administrators and policymakers when designing harm-reduction programs. Therefore, the coverage dimensions of DIC centers should be extended and prioritized to prevent epidemics of risky behaviors and their consequences, including HIV outbreaks, among IDUs. It is recommended to strengthen the quantity and quality of these centers and propagate them across the country.