1. Background
The coronavirus disease, a distinctive worldwide occurrence, is considered an empirical situation due to its impacts on different aspects of public and personal life (1).
This constant pandemic imposed societal quarantine associated with psychosomatic suffering and tension (2-6).
Most studies confirm that COVID-19 has considerably influenced individuals’ psychological well-being along with performance (7-11), with limited studies signifying the opposite (12).
However, young people are the least vulnerable (13). They are mainly vulnerable to mental health decline (14, 15). It is noteworthy that high stress levels were detected among students before the pandemic, too (16, 17).
A current review of virus occurrences and pandemics identified stressors like infection panics, irritation, monotony, insufficient supplies, lack of information, and financial difficulties (2). Most of the current literature on the mental effects of COVID-19 has emerged from hotspots in China. Nevertheless, most studies assessing the mental health impacts of epidemics have targeted the healthcare staff, youngsters, and the universal population (18, 19).
A survey of Turkish students in 2020 using the Generalized Anxiety Scale showed that 57% of the subjects had generalized anxiety disorder, while 63% had depressive disorder (20).
Late adolescence is typically considered a period of neurodevelopmental vulnerability, as there is a developmental discrepancy between established subcortical areas involved in reward-seeking and emotional processing and still developing prefrontal cortical sections (21, 22). This discrepancy can lead to poorly regulated risk-taking and emotional functioning (23, 24).
Cao et al. (25) found that almost a quarter (24.9%) of college students faced nervousness before COVID-19 in China.
There were investigated higher degrees of tension and distress signs in studies on the overall population in USA and Europe, although some studies from China were excluded (25, 26).
In an attempt to curb the COVID-19 spread, many countries worldwide have assumed different disease control measures, including strict social distancing measures, mandatory lockdowns, or stay-at-home orders (27, 28).
Although lockdown strategies successfully moderated the COVID-19 spread, they have negatively influenced people's way of life, resulting in serious mental and psychosomatic health consequences, particularly among young adults (29, 30).
Among the universal population, university students are predominantly vulnerable to the harmful effects of isolation (31-37).
Psychological well-being among university students seems to be a major public health issue that requires further research and data collection. Recent systematic reviews of primary research worldwide have highlighted the increased psychological burden associated with the COVID-19 pandemic (38, 39).
A large number of surveys have mentioned an enhancement in students’ tension levels through the pandemic and the detention time (40, 41), including diverse categories of hazard features, such as mental, genetic, and societal features, etc. (42).
2. Methods
The present research was a cross-sectional study conducted at the University of Medicine in Tirana, Albania, between March and May 2020. Our team of researchers conducted the study during the quarantine period of the COVID-19 pandemic in Albania.
The Ethics Committee of the University of Medicine in Tirana approved the study. Electronic informed consent was obtained from all participants before registration.
The study adhered to ethical requirements regarding the anonymity and voluntariness of participation. We added an informed consent question to the survey, and each participant consented to participate in the survey. The participants completed it in 15 minutes. Five hundred twenty-one participants replied to the invitation.
An online anonymous self-rated questionnaire was expanded through Google Form. The study link was sent to the participants via social media.
The survey was conducted only among students with Internet access.
The study’s inclusion criteria included having access to the Internet and being a student at the University of Medicine in Tirana, Albania.
To prevent multiple responses from the same participant, each device (e.g., mobile phone or computer) was allowed to submit the questionnaire only once, and logic tests were used to identify invalid responses. All valid responses were stored in a data folder and reviewed by two independent researchers.
The online questionnaire included questions about demographic characteristics, information on the transmission ways of COVID-19, mental health, health behaviors, social distancing, COVID-19-related social media use, and the impact of COVID-19 on their lives.
The Albanian-adapted version of the Perceived Stress Scale (PSS10) (43) was employed to measure whether the respondents appraised the situation in their life as stressful. The PSS10 consists of 10 items referring to the frequency of stressful events that occurred the month preceding the study and is assessed on a 5-point scale (0 = never to 4 = very often). The internal reliability of the Albanian students was adequate at 0.70 (43). The Cronbach’s alpha for this sample was 0.72.
The Perception of COVID-19’s Impact (PCI) on Well-being (44) was measured using five statements rated on a 5-item Likert scale (“1 = strongly disagree” to “5 = definitely agree”). The PCI measures how much students are afraid that the present circumstances associated with the COVID-19 pandemic may negatively impact their life in each of the following areas:
(1) School performance,
(2) Relationships with family and friends,
(3) Emotional status, and
(4) Social distancing etc.
Higher scores indicated the most significant COVID-19--related concerns. Internal reliability of the scale was appropriate (Cronbach’s alpha = 0.72).
We used the statistical package SPSS 26.0. To analyze numeric variables, we used descriptive statistics and the chi-square test to analyze cross-tabulations of the survey response data for categorical variables.
3. Results
A total of 521 students participated in the online survey. The students’ age range was 18 - 22 years, with a mean age of 20 (1.3) years. According to gender, 92.9% were female, while 7.1% were male.
The demographic characteristics of the respondents are reported in Table 1.
| Variables | Values |
|---|---|
| Age, y | 20 ± 1.3 |
| 18 | (16.5) |
| 19 | (27.6) |
| 20 | (35.2) |
| 21 | (13.6) |
| 22 | (7.1) |
| Gender | |
| Male | 37 (7.1) |
| Female | 484 (92.9) |
| Place of birth | |
| Urban | 333 (64) |
| Rural | 188 (36) |
| Field of study | |
| Medicine | 85 (16.3) |
| Dentistry | 122 (23.4) |
| Public health | 48 (9.25) |
| Nursing | 61 (11.7) |
| Pharmacy | 45 (8.67) |
| Physiotherapy | 59 (11.32) |
| Imaging | 28 (5.37) |
| Speech therapist | 17 (3.26) |
| Laboratory technician | 32 (6.14) |
| Midwife | 24 (4.6) |
Values are expressed as Mean ± SD or No. (%).
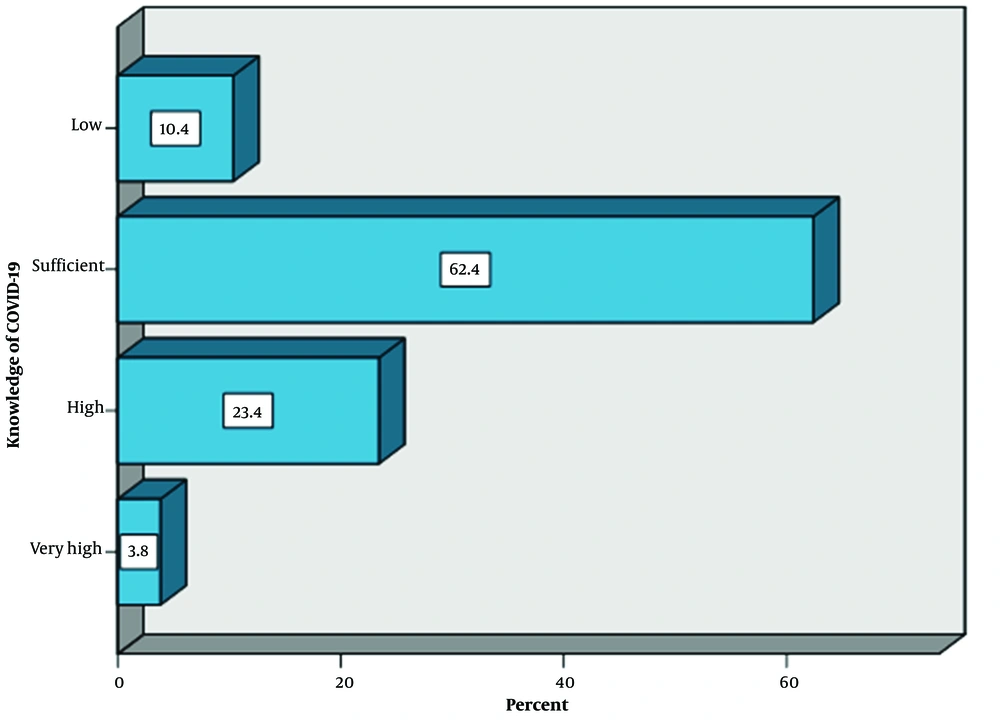
The students’ approach regarding knowledge of COVID-19 (Figure 1) stated that 62.4% had sufficient knowledge about the transmission ways of COVID-19, whereas 10.4% had low knowledge.
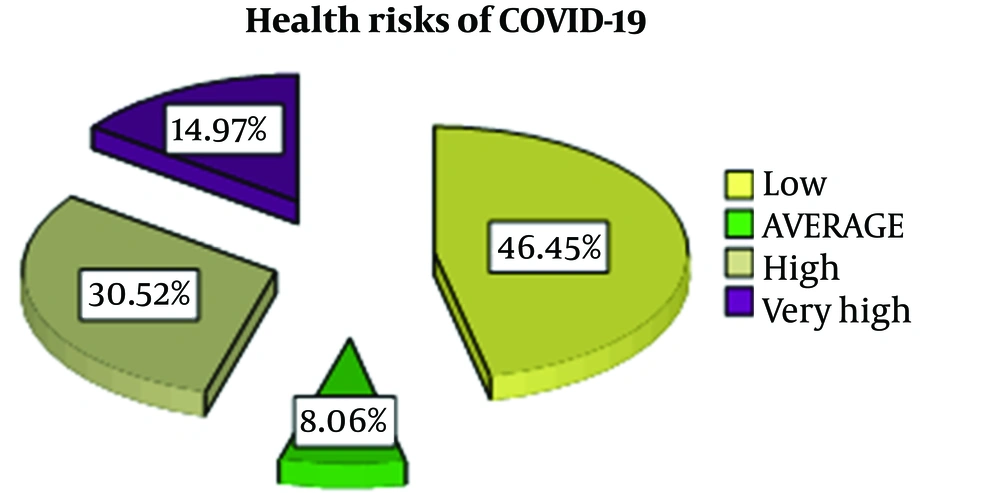
Regarding the students’ views on the risks of COVID-19, 46.4% of the respondents reported the risks of COVID-19 as low, 45.5% perceived high risk, and 8.1% reported a moderate level. The result refers to the students' perceptions of the risks rather than a general statement about the disease (Figure 2).
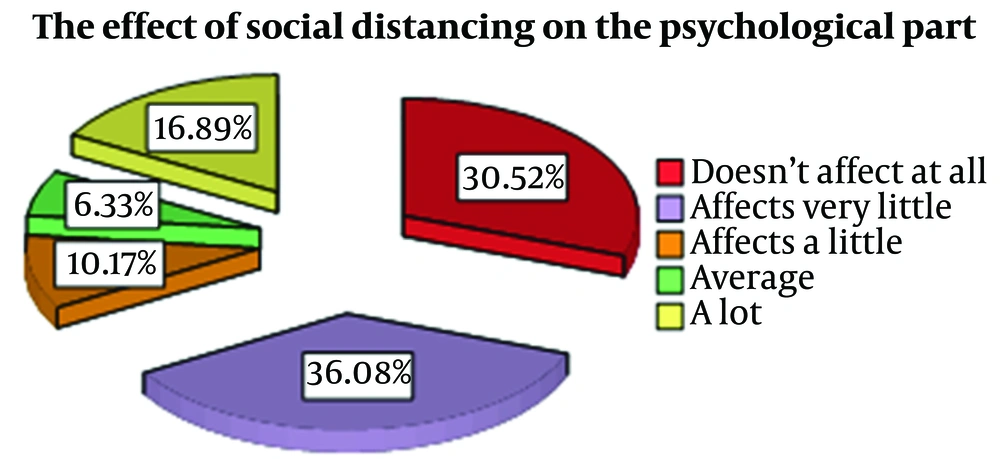
According to how social distancing in quarantine is related to the psychological status of students, 30.52% mentioned that it had no effect at all, 36.08% reported that it affected very little, 10.17% reported its effect a little, 6.33% reported its effect to a moderate level, and 16.89% reported a high level of effect (Figure 3).
The majority of university students supported social distancing measures and reported that it had no significant impact on their psychological well-being during the COVID-19 quarantine period.
Concerning stress management in quarantine, 88.1% reported that they did not manage stress, while 11.9% had tried to manage it.
Concerning the students’ approach to trusted sources of information during the COVID-19 pandemic, 85.4% mentioned friends, 11.1% mentioned the WHO, 2.1% mentioned the government, and 0.2% mentioned the media as their trusted sources of information, suggesting that the students may not be aware of the importance of relying on trusted sources, such as the WHO and the government, for COVID-19-related information.
Using the Pearson chi-square and the likelihood ratio, a significant correlation was observed between treatment for health problems and perceived health risks of the COVID-19 pandemic (P = 0.041).
Concerning discussing mental health treatment during the COVID-19 pandemic, it was found that 95.4% of the participants were not treated for mental health compared to 4.6% being treated.
A chi-square test revealed a statistically significant difference between the groups (P = 0.0001) treated for mental health compared to those not treated.
In addition, a strong correlation was found between the variables of social distancing and the right information from the Internet (P = 0.05).
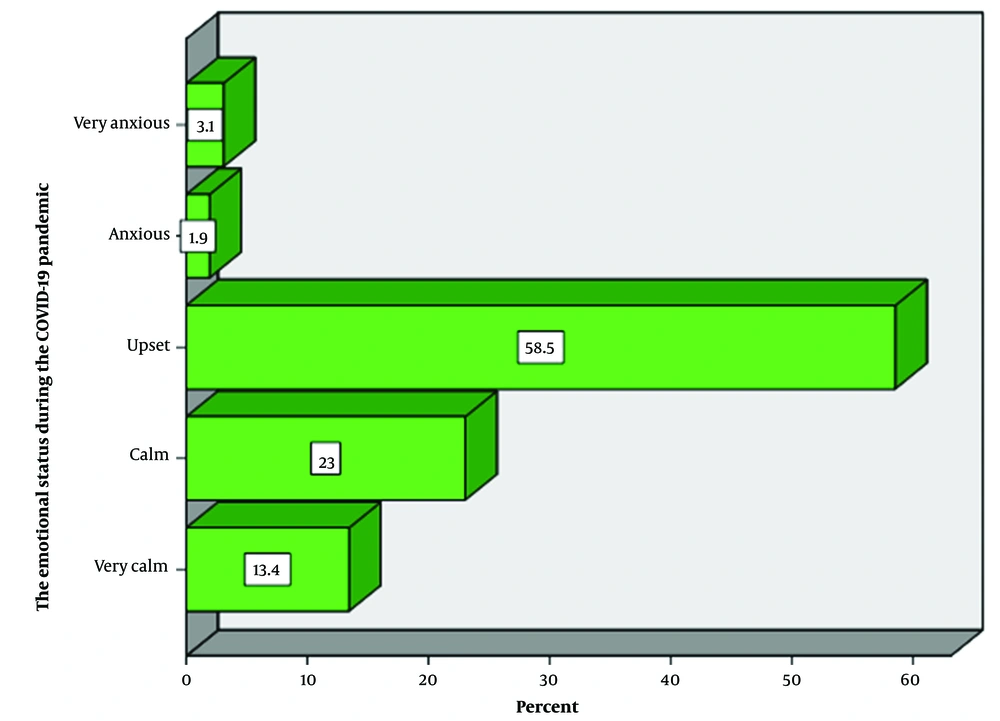
In the view of the study respondents, it was observed that before the question regarding COVID-19-related emotional status, 58.5% of the students reported to be upset, 1.9% anxious, 3.1% very anxious, and 23% calm. Using the chi-square test where P = 0.00001, a statistically significant difference was found among the abovementioned groups (Figure 4).
Regarding the evaluation of health care staff during the pandemic, 39.7% mentioned that health staff’s work was at an average level, and 38.8% replied that the health service was too little, with a statistically significant difference between the two groups (P = 0.0001).
A positive correlation was noticed between the variables of the COVID-19-related emotional status and health risks (P = 0.01).
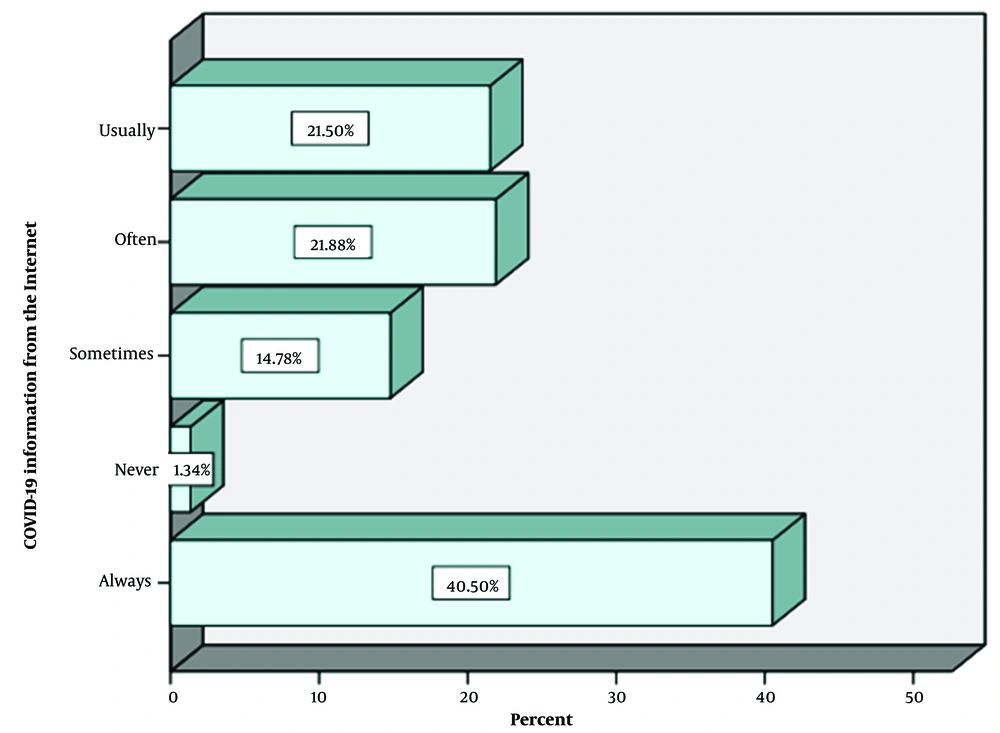
Regarding the sources of COVID-19 information, 40.5% of the students reported that they always got the information from the Internet, and 1.4% reported never getting the COVID-19 information from the Internet, with a statistically significant difference between the two groups (Figure 5).
4. Discussion
Students involve a category of measured people mainly susceptible to psychological distress. Our results reveal several outcomes of pandemic-linked alterations in psychological distress plus the students’ welfare.
According to the findings of this study, COVID-19 has had substantial harmful effects on well-being and daily life consequences. It was observed that many respondents had perceived elevated stress due to COVID-19, which they could not manage. The same results were found in a study on COVID-19 in England (45).
The present study indicates that the individuals reporting low health risks of COVID-19 had huge expectations of treating health problems.
Contributors expressed some obstacles to seeking help, like the absence of faith in psychotherapy facilities and difficulty in giving out psychological health problems due to stigma. It is frequent for students to consider stigma an obstacle and to look for assistance in psychoanalytic examinations (46).
The findings of our study showed that based on the responses to the questionnaire, 60% of the students got COVID-19-related information through the Internet and not official, reliable sources.
It has been recommended that digital web-based platforms may improve knowledge and contact with health suppliers to decrease stigma prior to psychological issues among children in deprived districts (47).
4.1. Conclusions
Twenty-three students reported being treated for mental health issues during the COVID-19 quarantine period.
Future lockdown strategies should consider the harmful consequences of COVID-19 on student mental health. They should focus on controlling individual meetings, such as in-person instruction, allowing communication in classes, entertainment spaces, etc. We must consider the significant quarantine’s impact, particularly in epidemic circumstances where individuals are missing social networks (48). Through future lockdowns, professors and psychotherapists should strengthen controlled individual university meetings.
The COVID-19 pandemic caused significant distress among students. Based on the results of this study, students were aware of the COVID-19 pandemic and had adequate knowledge of this worldwide distress, but there were gaps in different areas.
Students recognized how the virus is spread, its symptoms, and the preventive measures required to be taken by both individuals and the community. Given the WHO’s recommendation, students are in favor of the COVID-19 vaccine, while a substantial proportion of students demonstrated doubt.
From an educational perspective, students were reluctant to adopt an online merged learning approach due to technological and monetary restrictions. Despite increased stress among students concerning the risk of getting the COVID-19 infection, there is sufficient evidence that students of the University of Medicine in Tirana, Albania, practice measures to deal with stress during this global health hazard.
Through this COVID-19 pandemic, students were receptive and contented with the government’s proposals to limit the extent of infection.
However, there was augmented stress sensed by students concerning getting the COVID-19 infection. There is still sufficient evidence that the students of the University of Medicine in Tirana, Albania, practice measures to deal with stress during this global health hazard.
Universities should also adopt an innovative and supportive approach to address the students’ mental health problems during a pandemic. More importantly, as Albania is still in the phase of accepting the pattern shift in academic release, schools should begin guiding students and teachers on the relevance of online-merged learning approaches and develop information and communication technology (ICT) supplies and abilities for both teachers and students.
The government subsidy and educational sustainability in the future should include capacitating Albanian learners in applying online tools, bearing in mind health challenges like this.