1. Background
According to the World Health Organization (WHO), cancers are the second cause of death globally, which cause more than 10 million deaths and cost over a trillion dollars every year (1-5). Cancers are a diverse set of diseases that involve the abnormal and uncontrolled growth and spread of cells in different organs or tissues of the body (3). It is estimated that the incidence of cancer in Iran will increase by 42.6%, from 112,000 cases in 2016 to 160,000 cases in 2025. Cancer mortality in Iran was over 79,000 people in 2020 (6, 7). Since cancer is a chronic condition that affects people for a long time, it is very important to assess the situation of cancer patients comprehensively. This assessment should not only include the clinical and medical outcomes of the patients but also their quality of life (QoL) (8). The QoL is a key indicator of the effectiveness of cancer treatments (9). The WHO defines QoL as an individual’s perception of his or her position in life within the context of his or her personal values and goals (10).
The QoL is an important treatment objective, especially for chronic diseases. Research on QoL is used for various purposes, such as policy-making, treatment evaluation, and descriptive and individual clinical purposes (10). The EORTC (European Organization for Research and Treatment of Cancer) Core Quality of Life (QLQ-C30) tool is a specific instrument developed by the European EORTC group to measure the QoL of cancer patients. Every year, more than 5 000 studies use this tool, which has been translated and validated in over 120 languages (11). Cancer patients live longer due to new treatment methods, but their QoL also changes over time. Moreover, QoL has a significant impact on the long-term survival of cancer patients. Therefore, more research is needed to understand how QoL findings can inform the care of cancer patients (12, 13).
Cancer is a growing burden that has enormous physical, emotional, and financial effects on individuals, families, communities, and health systems. Many health systems in low- and middle-income countries are not equipped to handle the high number of cancer patients and their needs. As a result, cancer patients often face delays or barriers in accessing diagnostic and treatment services for cancer (3). Stressful situations can also create problems that exacerbate these challenges and affect the QoL of cancer patients significantly (14-16). One of these situations that has caused a lot of worry and stress is the outbreak of coronavirus disease 2019 (COVID-19) (17, 18). The coronavirus outbreak has been stressful for everyone, but especially for people with cancer who are at higher risk of complications (19, 20). This stress and mental pressure caused by the coronavirus outbreak may lead cancer patients to suffer from these conditions and postpone their treatment due to fear of infection or even avoid going to the hospital and receiving care (18). Therefore, COVID-19 can negatively affect the routine treatments of cancer patients and lower their QoL (21, 22).
2. Objectives
To the best of our knowledge, there has been no study on the QoL of cancer patients during the Coronavirus outbreak in Iran. Therefore, we conducted this study with the aim of investigating cancer patients’ QoL during the COVID-19 outbreak in an Iranian hospital.
3. Methods
We measured the QoL of cancer patients who had to visit public hospitals during the COVID-19 outbreak. We used a survey called QLQ-C30 that measures different aspects of QoL, such as physical, emotional, and social well-being. The EORTC QLQ-C30 is a disease-specific measure of QoL that evaluates the functional health, symptom burden, and HRQoL of cancer patients across different disease stages. It was developed by the EORTC, a European organization dedicated to cancer research and treatment. The original version was published in 1993, but the current version (QLQ-C30 v3.0) has been in use since 1997. It has 30 items and includes 15 scales. Five scales measure how well people can do physical, role, emotional, cognitive, and social activities, and 9 scales evaluate how much people suffer from fatigue, nausea and vomiting, pain, shortness of breath, sleep problems, loss of appetite, constipation, diarrhea, financial troubles and a scale that assesses their overall health and QoL. The QLQ-C30 can be supplemented with disease- or treatment-specific modules (11). The Persian version QLQ-C30 was used, as its validity and reliability have been established (11, 23). The reliability and validity of the Persian version of the QLQ-C30 questionnaire have been evaluated, and the results have shown that the Iranian version of EORTC QLQ-C30 is reliable (alpha = 76 - 93%) and valid (almost all inter-scale correlations were significant in the expected direction; Pearson’s r was ≥ 40 in conceptually related scales and < 40 in scales with less in common) for measuring the QoL of cancer patients. Also, the content validity index (CVI) and content validity ratio (CVR) of the questionnaire were 0.94 and 0.76, respectively (11, 23, 24). We used the manuals from the EORTC QoL group website as our guide for scoring. These manuals have essential information for scoring the EORTC core questionnaire and its related modules (11). The range score of each dimension was from 0 to 100. We focused on the Dialysis Department of Rasoul Akram Hospital in Tehran, which treated both COVID-19 and cancer patients at the same time in 2021. We asked all the cancer patients who met our criteria to fill out the survey. They had to be 18 years or older, have a cancer diagnosis, and understand Persian. We had 150 eligible patients between January and February 2021, but only 85 completed the survey. At the time of the study and based on inclusion and exclusion criteria, all eligible patients (87 patients) in the study period were included in the study by census sampling method, and 85 of them completed the questionnaire. We did not exclude any patients based on their type or stage of cancer. We explained the purpose of the study to the patients and received their consent before giving them the survey. If they could not read, we read the questions to them and recorded their answers. We used SPSS (IBM Corp., Armonk, NY, USA) to analyze the data with an independent t-test and analysis of variance (ANOVA).
4. Results
We studied 85 cancer patients visiting the hospital for chemotherapy. The mean (standard deviation) of their age was 54.42 ± 14.76 years. The median of the disease’s duration in the patients was 12 months; the first quartile and third quartile were 7 months and 30 months, respectively. Moreover, 70.6% (60 people) of the patients were female, and 29.4% (25 people) were male. shows the other demographic characteristics of the patients.
| Demographic Status | Variables | No. (%) |
|---|---|---|
| Sex | Female | 60 (70.6) |
| Male | 25 (29.4) | |
| Age (y) | ≤ 40 | 13 (15.3) |
| 41 - 50 | 16 (18.8) | |
| 51 - 60 | 20 (23.5) | |
| 61 - 70 | 22 (25.9) | |
| ≥ 71 | 14 (16.5) | |
| Insurance type | Without insurance | 7 (8.2) |
| Social security | 57 (67.1) | |
| Medical service | 21 (24.7) | |
| Duration of cancer diagnosis (mo) | ≤ 12 | 50 (58.8) |
| 13 - 60 | 20 (23.5) | |
| > 61 | 15 (17.6) | |
| Cancer type | Blood | 11 (12.9) |
| Lung | 11 (12.9) | |
| Breast | 31 (36.5) | |
| Glands | 5 (5.9) | |
| Genital area | 15 (17.6) | |
| Head | 12 (14.1) |
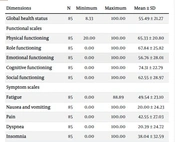
Table 2 shows the indicators of descriptive statistics related to the QoL of cancer patients based on the EORTC QLQ-C30 questionnaire. The patients’ average (standard deviation) QoL in the dimension of global health status was 55.49 ± 21.27. In functional scales, the average cognitive functioning score had the highest (74.31 ± 22.79) value, and emotional functioning had the lowest (56.76 ± 28.01) value. In the symptom scales, the average score of financial difficulties was the highest (62.75 ± 35.04), and nausea and vomiting were the lowest (49.54 ± 23.10).
| Dimensions | N | Minimum | Maximum | Mean ± SD |
|---|---|---|---|---|
| Global health status | 85 | 8.33 | 100.00 | 55.49 ± 21.27 |
| Functional scales | ||||
| Physical functioning | 85 | 20.00 | 100.00 | 65.33 ± 20.80 |
| Role functioning | 85 | 0.00 | 100.00 | 67.84 ± 25.82 |
| Emotional functioning | 85 | 0.00 | 100.00 | 56.76 ± 28.01 |
| Cognitive functioning | 85 | 0.00 | 100.00 | 74.31 ± 22.79 |
| Social functioning | 85 | 0.00 | 100.00 | 62.55 ± 28.97 |
| Symptom scales | ||||
| Fatigue | 85 | 0.00 | 88.89 | 49.54 ± 23.10 |
| Nausea and vomiting | 85 | 0.00 | 100.00 | 20.00 ± 24.23 |
| Pain | 85 | 0.00 | 100.00 | 42.55 ± 27.03 |
| Dyspnea | 85 | 0.00 | 100.00 | 20.39 ± 24.72 |
| Insomnia | 85 | 0.00 | 100.00 | 38.04 ± 32.59 |
| Loss of appetite | 85 | 0.00 | 100.00 | 34.51 ± 33.51 |
| Constipation | 85 | 0.00 | 100.00 | 29.41 ± 31.88 |
| Diarrhea | 85 | 0.00 | 100.00 | 20.78 ± 25.71 |
| Financial difficulties | 85 | 0.00 | 100.00 | 62.75 ± 35.04 |
Table 3 shows descriptive indicators and results of independent t-test and ANOVA to compare patients’ average quality of working life in global health status and functional scales. The global health status scores did not vary significantly by any demographic factors. However, the type of insurance had a significant effect on the average cognitive functioning scores in the functional scales (P-value = 0.043). Patients with Medical Service insurance had the highest (79.37 ± 21.02) cognitive functioning, while patients without insurance had the lowest (54.76 ± 29.99). The average scores of other dimensions based on demographic characteristics were not statistically significant.
| Variables | N | Global Health Status | Physical Functioning | Role Functioning | Emotional Functioning | Cognitive Functioning | Social Functioning | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Female | 60 | 56.11 ± 20.69 | 0.679 | 64.33 ± 20.12 | 0.496 | 69.17 ± 24.52 | 0.467 | 55.97 ± 27.45 | 0.689 | 74.44 ± 23.26 | 0.935 | 63.61 ± 27.01 | 0.604 |
| Male | 25 | 54 ± 22.96 | 67.73 ± 22.58 | 64.67 ± 29 | 58.67 ± 29.8 | 74 ± 22.09 | 60 ± 33.68 | |||||||
| Age (y) | ≤ 40 | 13 | 62.82 ± 17.55 | 0.155 | 69.74 ± 16.47 | 0.517 | 60.26 ± 26.82 | 0.525 | 58.33 ± 29.07 | 0.615 | 78.21 ± 18.49 | 0.941 | 73.08 ± 19.88 | 0.474 |
| 41-50 | 16 | 59.9 ± 24.95 | 70 ± 21.22 | 76.04 ± 22.75 | 58.85 ± 28.78 | 76.04 ± 30.41 | 65.63 ± 26.15 | |||||||
| 51-60 | 20 | 59.17 ± 24.32 | 67 ± 22 | 68.33 ± 29.07 | 62.5 ± 29.68 | 74.17 ± 21.27 | 55.83 ± 32.12 | |||||||
| 61-70 | 22 | 47.35 ± 15.51 | 61.21 ± 22.5 | 68.94 ± 26.38 | 48.86 ± 28.32 | 72.73 ± 20.92 | 58.33 ± 31.6 | |||||||
| ≥ 71 | 14 | 51.19 ± 20.89 | 60 ± 19.74 | 63.1 ± 22.81 | 57.14 ± 24.21 | 71.43 ± 23.96 | 65.48 ± 30.29 | |||||||
| Insurance type | Without insurance | 7 | 48.81 ± 16.96 | 0.673 | 59.05 ± 22.58 | 0.705 | 57.14 ± 31.71 | 0.513 | 42.86 ± 28.23 | 0.394 | 54.76 ± 29.99 | 0.043 | 54.76 ± 12.6 | 0.707 |
| Social security | 57 | 56.43 ± 21.88 | 66.08 ± 20.56 | 68.42 ± 25.91 | 57.89 ± 28.5 | 74.85 ± 21.62 | 64.04 ± 27.24 | |||||||
| Medical service | 21 | 55.16 ± 21.32 | 65.4 ± 21.56 | 69.84 ± 23.93 | 58.33 ± 26.61 | 79.37 ± 21.02 | 61.11 ± 37.02 | |||||||
| Duration (months) | ≤ 12 | 50 | 57 ± 21.39 | 0.715 | 66.13 ± 20.11 | 0.903 | 68 ± 25.83 | 0.438 | 56.17 ± 27.08 | 0.427 | 76 ± 21.6 | 0.576 | 65.33 ± 27.53 | 0.571 |
| 13 - 60 | 20 | 54.17 ± 25.58 | 63.67 ± 25.91 | 72.5 ± 26.09 | 62.92 ± 31.7 | 74.17 ± 21.27 | 59.17 ± 34.4 | |||||||
| > 61 | 15 | 52.22 ± 14.25 | 64.89 ± 16.23 | 61.11 ± 25.72 | 50.56 ± 26.06 | 68.89 ± 28.78 | 57.78 ± 26.63 | |||||||
| Cancer type | Blood | 11 | 53.79 ± 18.77 | 0.131 | 64.85 ± 17.66 | 0.648 | 56.06 ± 21.44 | 0.130 | 60.61 ± 25.84 | 0.449 | 80.3 ± 17.98 | 0.368 | 66.67 ± 29.81 | 0.667 |
| Lung | 11 | 59.85 ± 21.99 | 63.64 ± 18.22 | 69.7 ± 27.71 | 60.61 ± 33.35 | 78.79 ± 19.85 | 62.12 ± 35.82 | |||||||
| Breast | 31 | 62.1 ± 22.75 | 69.46 ± 20.35 | 71.51 ± 22.85 | 61.56 ± 25.15 | 77.42 ± 22.99 | 67.2 ± 24.9 | |||||||
| Glands | 5 | 51.67 ± 16.03 | 66.67 ± 8.16 | 80 ± 21.73 | 56.67 ± 19.9 | 70 ± 27.39 | 66.67 ± 11.79 | |||||||
| Genital area | 15 | 51.11 ± 22.68 | 64.89 ± 25.38 | 74.44 ± 28.78 | 52.78 ± 32.83 | 71.11 ± 23.12 | 52.22 ± 36.66 | |||||||
| Head | 12 | 43.06 ± 13.69 | 56.67 ± 24.7 | 54.17 ± 28.54 | 42.36 ± 28.08 | 62.5 ± 25.75 | 58.33 ± 27.06 | |||||||
Table 4 shows the descriptive indicators and results of independent t-test and ANOVA to compare patients’ average quality of working life in the symptom scales dimension. According to Table 4, The patient’s age (P-value < 0.001) and type of cancer (P-value < 0.001) had a significant impact on the average score of appetite loss. Therefore, the average score of appetite loss was the highest in patients under 40 years (51.28 ± 35) and the highest in patients with head cancer (61.11 ± 34.33). The difference between the average of other dimensions of symptom scales based on demographic characteristics was not statistically significant.
| Variables | N | Fatigue | Nausea and Vomiting | Pain | Dyspnea | Insomnia | Loss of Appetite | Constipation | Diarrhea | Financial Difficulties | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Female | 60 | 49.81 ± 21.21 | 0.867 | 18.61 ± 24.76 | 0.416 | 41.67 ± 27.01 | 0.644 | 21.11 ± 26.01 | 0.680 | 36.11 ± 31.47 | 0.401 | 32.78 ± 32.18 | 0.464 | 29.44 ± 31.94 | 0.988 | 18.89 ± 24.06 | 0.295 | 61.11 ± 34.81 | 0.509 |
| Male | 25 | 48.89 ± 27.59 | 23.33 ± 23.07 | 44.67 ± 27.52 | 18.67 ± 21.69 | 42.67 ± 35.38 | 38.67 ± 36.87 | 29.33 ± 32.38 | 25.33 ± 29.31 | 66.67 ± 36 | ||||||||||
| Age (y) | ≤ 40 | 13 | 52.14 ± 21.46 | 0.467 | 20.51 ± 21.68 | 0.932 | 34.62 ± 26.75 | 0.377 | 15.38 ± 17.3 | 0.367 | 46.15 ± 34.8 | 0.611 | 51.28 ± 35 | < 0.01 | 30.77 ± 34.59 | 0.655 | 23.08 ± 25.04 | 0.822 | 66.67 ± 33.33 | 0.634 |
| 41 - 50 | 16 | 40.97 ± 22.12 | 16.67 ± 25.09 | 38.54 ± 26.33 | 14.58 ± 17.08 | 31.25 ± 33.26 | 8.33 ± 14.91 | 22.92 ± 29.11 | 18.75 ± 27.13 | 60.42 ± 34.89 | ||||||||||
| 51 - 60 | 20 | 47.78 ± 26.27 | 21.67 ± 29.67 | 51.67 ± 26.98 | 16.67 ± 20.23 | 31.67 ± 29.57 | 25 ± 28.36 | 38.33 ± 37.89 | 18.33 ± 25.31 | 66.67 ± 34.2 | ||||||||||
| 61 - 70 | 22 | 54.55 ± 18.75 | 18.18 ± 22.95 | 44.7 ± 29.72 | 27.27 ± 33.55 | 42.42 ± 32.82 | 48.48 ± 35.23 | 27.27 ± 31.93 | 25.76 ± 28.97 | 66.67 ± 32.53 | ||||||||||
| ≥ 71 | 14 | 51.59 ± 27.08 | 23.81 ± 21.4 | 38.1 ± 23.05 | 26.19 ± 26.73 | 40.48 ± 35.03 | 40.48 ± 32.5 | 26.19 ± 23.31 | 16.67 ± 21.68 | 50 ± 42.87 | ||||||||||
| Insurance type | Without insurance | 7 | 53.97 ± 17.48 | 0.872 | 26.19 ± 25.2 | 0.757 | 45.24 ± 20.89 | 0.770 | 23.81 ± 31.71 | 0.908 | 47.62 ± 26.23 | 0.716 | 47.62 ± 26.23 | 0.563 | 28.57 ± 29.99 | 0.813 | 38.1 ± 29.99 | 0.146 | 85.71 ± 17.82 | 0.168 |
| Social security | 57 | 49.12 ± 25.97 | 19.88 ± 25.09 | 43.57 ± 27.59 | 20.47 ± 25.78 | 36.84 ± 33.14 | 33.33 ± 35.07 | 28.07 ± 33.21 | 18.13 ± 21.89 | 61.99 ± 33 | ||||||||||
| Medical service | 21 | 49.21 ± 15.94 | 18.25 ± 22.3 | 38.89 ± 28.05 | 19.05 ± 19.92 | 38.1 ± 33.81 | 33.33 ± 31.62 | 33.33 ± 29.81 | 22.22 ± 32.2 | 57.14 ± 42.35 | ||||||||||
| Duration | ≤ 12 | 50 | 50.22 ± 22.36 | 0.948 | 20 ± 24.28 | 0.784 | 41 ± 25.47 | 0.821 | 22.67 ± 26.46 | 0.348 | 39.33 ± 34.13 | 0.764 | 36 ± 36.17 | 0.455 | 29.33 ± 32.74 | 0.832 | 23.33 ± 28.77 | 0.334 | 61.33 ± 36.49 | 0.760 |
| 13 – 60 | 20 | 48.33 ± 26.56 | 17.5 ± 19.85 | 45 ± 33.81 | 13.33 ± 19.94 | 33.33 ± 28.61 | 26.67 ± 29.81 | 26.67 ± 33.51 | 13.33 ± 19.94 | 61.67 ± 32.94 | ||||||||||
| > 61 | 15 | 48.89 ± 22.14 | 23.33 ± 30.08 | 44.44 ± 23.29 | 22.22 ± 24.12 | 40 ± 33.81 | 40 ± 28.73 | 33.33 ± 28.17 | 22.22 ± 20.57 | 68.89 ± 34.43 | ||||||||||
| Cancer type | Blood | 11 | 59.6 ± 21.24 | 0.272 | 33.33 ± 22.36 | 0.244 | 53.03 ± 20.84 | 0.256 | 21.21 ± 26.97 | 0.650 | 30.3 ± 23.35 | 0.305 | 45.45 ± 34.23 | 0.001 | 36.36 ± 23.35 | 0.925 | 36.36 ± 17.98 | 0.138 | 60.61 ± 35.96 | 0.673 |
| Lung | 11 | 44.44 ± 22.77 | 13.64 ± 17.98 | 33.33 ± 29.81 | 24.24 ± 15.57 | 45.45 ± 37.34 | 48.48 ± 40.45 | 27.27 ± 29.13 | 30.3 ± 34.82 | 66.67 ± 33.33 | ||||||||||
| Breast | 31 | 45.88 ± 21.03 | 16.13 ± 23.37 | 36.56 ± 24.5 | 16.13 ± 24.15 | 35.48 ± 30.95 | 18.28 ± 22.51 | 26.88 ± 34.87 | 18.28 ± 28.33 | 61.29 ± 35.59 | ||||||||||
| Glands | 5 | 46.67 ± 22.77 | 23.33 ± 19 | 40 ± 14.91 | 20 ± 18.26 | 40 ± 43.46 | 33.33 ± 23.57 | 20 ± 18.26 | 20 ± 18.26 | 40 ± 43.46 | ||||||||||
| Genital area | 15 | 45.93 ± 30.82 | 15.56 ± 20.38 | 46.67 ± 35.19 | 17.78 ± 21.33 | 28.89 ± 24.77 | 28.89 ± 33.01 | 33.33 ± 35.63 | 11.11 ± 16.27 | 64.44 ± 40.76 | ||||||||||
| Head | 12 | 60.19 ± 16.72 | 27.78 ± 35.06 | 52.78 ± 25.46 | 30.56 ± 36.12 | 55.56 ± 41.03 | 61.11 ± 34.33 | 30.56 ± 36.12 | 16.67 ± 22.47 | 72.22 ± 23.92 | ||||||||||
5. Discussion
The purpose of this study was to examine the QoL of cancer patients during the COVID-19 pandemic. We used version 3 of the QLQ-30 questionnaire, a specific instrument developed by the European EORTC group, to measure the QoL of cancer patients. This questionnaire is widely employed in many studies around the world every year (11). Besides the fear and anxiety caused by the coronavirus, cancer patients have postponed receiving some of their services due to the epidemic conditions and the healthcare system’s lack of complete response capacity. Therefore, this issue can easily change patients’ QoL suffering from chronic cancer conditions (18). Although the effect of the COVID-19 pandemic on cognitive and emotional vulnerability (17), mental health (25), and challenges related to health and treatment conditions (26) of cancer patients in Iran has been investigated, the QoL of these patients during the COVID-19 pandemic has not been paid much attention.
Examining the QoL of a number of cancer patients in Iran during the COVID-19 pandemic indicated that the overall score of their general health status was 55.5. If we put aside the rest of the confounding factors, some studies on the QoL of cancer patients in Iran before the COVID-19 pandemic showed that the numerical value of the general health status measured by the QLQ-C30 tool is 57.6 (27), 64 (28), and 60.4 (29) in many scenarios and different cancers. The average of these numbers is higher than 55.5. Therefore, pandemic conditions have reduced the QoL of cancer patients in Iran. Although the amount of health-related QoL has been negatively related to the COVID-19 pandemic (30), the effect of death anxiety on the overall QoL of cancer patients in Iran is at a medium level (16). Therefore, compared to the time before the COVID-19 pandemic, the QoL of cancer patients in Iran has also been moderately affected, and the pandemic conditions reduced the QoL of cancer patients to a medium level (not very low and not very much). The average state of public health in several studies conducted before the COVID-19 pandemic was around 70.02 (31), 60.4 (32), 67, or 70.1 (33). However, during the COVID-19 pandemic, some studies have reported similar numbers (71.3) (34), and some studies have reported a much lower amount (41.7) (21). Our results show that cancer patients’ general health status score has been very variable during the COVID-19 pandemic; its lowest level was 8.3. Cancer patients seem to suffer some reduction in the general health status score and vulnerability in QoL during pandemic conditions (21, 34, 35).
Besides the problems of receiving services during the pandemic and viral outbreak, cancer patients have a higher psychological vulnerability and suffer from problems such as mental anxiety (18), fear (20), and worry (19). They can be a factor in reducing the general health status score and overall reduction of the QoL. Therefore, during a pandemic such as COVID-19, reducing the factors that cause worry, anxiety, fear, and other psychological symptoms is necessary to control the decrease in cancer patients’ QoL and support them. In the functional scale, the scores of each situation ranged from 56.8 on the emotional scale to 74.3 on the cognitive scale. The pandemic conditions caused much psychological pressure on people, particularly cancer patients. Therefore, cancer patients postpone their treatments due to fear, worry, and anxiety. These patients also reduced their social life due to the fear of contracting COVID-19 (17, 18, 25, 26). Therefore, this situation can be aggravated for a cancer patient who suffers from a chronic illness and related challenges in emotional functioning. Although the evidence in emotional functioning before the pandemic is diverse, and we cannot conclude that the pandemic has worsened the emotional functioning situation (28, 36). This shows that cognitive functioning during the pandemic has been negatively affected (28, 36). Comparing QoL during the pandemic with other times in cancer patients, a relatively noticeable decrease is seen in other functional states, including physical, role, and social functions. Although functional scales and general health status in cancer patients during the pandemic in Iran show lower numbers compared to Denmark (34), the evidence indicates that functional scales and the average health status score during the COVID-19 pandemic have decreased. A significant part of this decrease is significant (19, 21, 37).
Symptomatic scales in the QLQ-C30 questionnaire, unlike the functional scales, indicate the deterioration of the QoL of cancer patients. The worst situation in symptom scales was financial difficulties, and the best situation was nausea and vomiting. Diarrhea and shortness of breath have shown almost similar numbers. Similarly, in the German and Ethiopian samples, cancer patients have shown lower mean scores of nausea, vomiting, and diarrhea in functional scales, so the QoL is less affected in this respect. In this sample, although in Ethiopia, like our study, the highest score was related to financial difficulties, in the German sample, the highest score and the worst symptom scale in cancer patients was related to insomnia. However, financial difficulties have also been significantly high (38).
A similar study in Iran indicates that before the COVID-19 pandemic, all symptom scales were significantly better in cancer patients compared to the time of the pandemic. This does not show a better situation even on 1 scale during the COVID-19 pandemic (36). The condition of Iranian patients compared to cancer patients in Denmark during the COVID-19 pandemic has been much worse in functional scales. In Danish cancer patients, the worst condition was fatigue, followed by insomnia, while in Iranian patients, the worst condition was financial difficulties, followed by fatigue. In the Danish sample, the best symptom scales included nausea, vomiting, and financial difficulties. While financial difficulties in Iranian cancer had the worst condition on symptom scales patients with a score of nearly 63, in Danish patients, it showed a number less than 6, which was one of the best conditions.
In the Danish sample of symptom scales, the highest value was about 30, and the lowest was 5. In comparison, the highest in the Iranian sample was about 63, and the lowest was 20 (32). In comparing the QoL of cancer patients before the pandemic in Germany to Ethiopia, there were significant differences in functional scales and symptom scales in favor of the German sample (36). Therefore, the evidence indicates that cancer patients in developed countries experience a better QoL than in developing countries. Several symptom scales have significantly deteriorated during the COVID-19 pandemic (21). The results indicate that no demographic variables had a relationship with functional scales and general health status in cancer patients. In this case, the difference in sex, age, duration, and type of cancer did not significantly affect the functional scales and the general health status of cancer patients. Although the effects of some variables were significant in similar studies, most had little effect on functional scales and general health status (37-39). Among the examined variables, only having or not having insurance affected the difference in cognitive performance, and people without insurance had the lowest cognitive scale. Since the lower limit of this scale was the lowest among cancer patients, it is necessary to review and reform the insurance status of cancer patients to improve their QoL. There is evidence of the effect of the insurance coverage status on the QoL in cancer patients, which confirms the present study’s results (40, 41).
Among the symptom scales, the difference in the age of the patients and the type of cancer significantly affected the difference in the loss of appetite score. The difference in other variables did not significantly affect other symptom scales. The study of cancer patients before the COVID-19 pandemic has also indicated that the age difference was significantly effective in the difference in symptom scales among patients (27). Nevertheless, further evidence exists in similar studies before the COVID-19 pandemic (42). In our study, variables such as age, type of cancer, and having or not having insurance have created significant differences in the QoL of cancer patients in Iran. Nevertheless, since the patients’ QoL has deteriorated during the coronavirus crisis compared to previous studies due to adverse psychological conditions during the pandemic period, issues such as resilience, hope, optimism, dignity, self-efficacy, family support, providing conditions to reduce fear and anxiety and worry caused by infection and death, seeking and providing conditions to receive necessary routine treatments for cancer patients to prevent the deterioration of the QoL of cancer patients are more critical. (18-20, 25, 26, 43, 44).
5.1. Conclusions
During the COVID-19 pandemic, insomnia and fatigue, along with financial difficulties in cancer patients, have caused the worst conditions related to symptom scales, which, along with the psychological problems caused by the pandemic conditions, can significantly reduce the QoL of cancer patients. QoL of cancer patients during the COVID-19 pandemic indicated that the worst situation was in the functional scales related to the patient’s emotional scales. All these cases confirm the importance of psychological and emotional support for cancer patients, especially in a pandemic. It seems the COVID-19 pandemic has generally affected the QoL of cancer patients negatively in terms of their overall health, their ability to function, and their experience of symptoms. Since only the insurance status, age, and type of cancer had an effect on the single symptom and functional scales among the examined variables, besides these factors, decision-makers and health care managers should consider other factors, such as psychological challenges related to the pandemic and control of fear, anxiety, and worry to provide services to cancer patients during the pandemic and ensure that they receive these services.