1. Background
Unintentional or spontaneous abortion (SA) is one of the most common complications of pregnancy (1, 2). It refers to abortion without any intentional measure. The underlying mechanisms of SA are very complex, and hence, SA prediction and prevention are very challenging for healthcare providers (1). Around 10% - 20% of all pregnancies end with abortion, and the prevalence of SA in the southeast of Iran is 15.7% (3).
Review studies on thousands of women reported that abortion has many different complications for women. Examples of these complications are loss of self-confidence in 90% of cases, substance abuse in 50% of cases, suicidal thoughts in 60% of cases, suicide attempts in 28% of cases, and severe post-traumatic stress disorder in 20% of cases (2). Abortion also has a heavy disease burden and high mortality rate in some countries, particularly developing countries (4, 5).
Psychological complications are among the most common complications of SA. Studies show that at least 48% - 51% of women with SA experience psychological complications (2, 6). Anxiety is one of the highly prevalent psychological complications of SA (2), such that many women with SA experience high levels of anxiety during the first 6 months after abortion (7). Anxiety is more common and more severe during the first 12 weeks after abortion (3). Some studies reported that abortion does not directly cause psychological complications; rather, factors such as pre-abortion mental health status, domestic violence, desire for pregnancy, and financial status can contribute to post-abortion anxiety and depression (8, 9). However, a study reported abortion as a stressful and traumatic event that leads to psychological complications (10).
The psychological manifestations of SA are almost identical to the psychological complications of losing an infant (11) or an adult significant other. Accordingly, grief is one of the common reactions to SA (12). The American Psychiatric Association considers grief as a normal depression in response to the death or loss of a beloved one (13). Grief at SA is as severe as grief at other types of major losses (14). Grief at the loss of a significant other is a completely personal process with a relatively predictable course and includes reactions such as temporary impairment of daily activities, retreat from social activities, intrusive thoughts, and subjective sense of numbness and emotional unresponsiveness that last for various periods of time (15). Although grief is a normal and non-pathologic phenomenon, it may lead to complex and long-term grief, particularly if the loss is sudden, violent, or traumatic (16).
Self-talk (ST) is a non-pharmacological therapy for psychological problems. By definition, ST is an internal voiceless, low-voice, or loud-voice dialogue through which individuals interpret their thoughts and emotions, change their evaluations and beliefs, and teach or promote themselves. It plays a significant role in the relationship of events and emotions and can help individuals calm themselves, control their anger, cope with difficult conditions, maintain their concentration and mental readiness, improve their motivation and skills, and retain their self-confidence (17). The 2 types of ST are positive ST and negative ST. Positive ST aims at correcting interpretations of events and can resolve most emotional and behavioral disorders (18), reduce anxiety, and improve self-confidence. On the other hand, negative ST can lead to anxiety, low self-esteem, and burnout. Self-talk can turn into a habit and influence individuals' attitudes and behaviors (19). It is a key factor in studying individuals' thoughts and beliefs, and its effective management without any force, command, or personal advice is a prerequisite to behavioral modification (17).
Most studies into the effects of ST were conducted on individuals with high educational levels and athletes. A study in this area reported that negative ST had a significant role in the pathology of eating disorders (20), while another study found that positive ST improved coping skills among women with breast cancer (21). A study on patients with coronavirus disease 2019 (COVID-19) also showed that ST had significant effects on death anxiety and coping strategies (22). However, there are no reliable data about the effects of ST on anxiety and grief among women with SA, and hence, the current study was conducted to provide further data in this area.
2. Objectives
The aim of this study was to assess the effects of positive ST on anxiety and grief among women with SA.
3. Methods
3.1. Design
This quasi-experimental study was conducted in 2021 using a two-group pre-test-post-test design. Participants were women with SA purposively selected from a teaching hospital affiliated with Zahedan University of Medical Sciences, Zahedan, Iran. Inclusion criteria were age of 18 - 35 years, no serious mental health disorder, no history of significant life events in the past 2 months except for SA, no history of substance abuse or cigarette smoking, hospitalization during the first 24 hours after SA, and an anxiety score of more than 11 on the Hospital Anxiety and Depression Scale. Exclusion criteria were voluntary withdrawal, using other counseling services during the study, missing more than 2 educational sessions, risk of threatened abortion, and pregnancy during the study. Participants who were recruited in the first week of the study were randomly allocated to 1 of the study groups, and participants recruited in the second week of the study were randomly allocated to the other group. This alternative randomization was continued until 40 women were allocated to each study group. This type of randomization was employed to prevent between-group leakage of information.
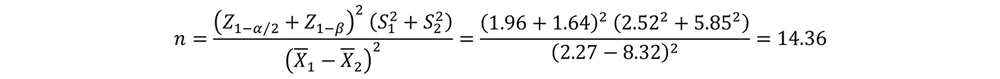
The sample size was calculated based on the results of a previous study, which reported that the mean score of anxiety was 2.27 ± 2.52 in the intervention group and 8.32 ± 5.85 in the control group (23). Accordingly, with a confidence level and a power of 0.95, the sample size was determined to be 15 per group (Figure 1). Yet, 40 women were recruited in each group to compensate for probable withdrawals and improve the power of the study.
3.2. Instruments
The study instruments were a demographic questionnaire, the Hospital Anxiety and Depression Scale, and the Perinatal Grief Scale. The items of the demographic questionnaire examined age, educational level, occupation, number of children, number of abortions, duration of marriage, gestational week, and intention for pregnancy.
Hospital Anxiety and Depression Scale (HADS): Zigmond and Snaith introduced this scale in 1983 for the assessment of depression and anxiety. It has 14 items in 2 dimensions, namely anxiety (odd items) and depression (even items). We used only the anxiety dimension of this scale. Items are scored on a 4-point Likert scale as follows: 0: "Never"; 1: "Mild"; 2: "Moderate"; and 3: "Severe". Items 1, 3, 5, 8, 10, 11, and 13 are reversely scored. Anxiety scores are interpreted as follows: 0 - 7: Normal; 7 - 11: Mild anxiety; 11 - 15: Moderate anxiety; and 15 - 21: Severe anxiety. This scale is suitable for mental health screening (24). A study reported validity (r = 0.53, P < 0.001) and reliability by test re-test (r = 0.75, P < 0.001) and by internal consistency of the Cronbach's alpha was 0.85 25 of the anxiety dimension of the scale. The Cronbach's alpha of this dimension in the present study was 0.83, confirming its acceptable reliability.
Perinatal Grief Scale (PGS-P): Potvin et al. developed this scale to assess grief at pregnancy loss. It has 33 items in three 11-item dimensions, namely active grief, difficulty in coping, and despair. Items are scored on a 5-point Likert scale as follows: 1: "Strongly disagree"; 2: "Disagree"; 3: "Neither agree nor disagree"; 4: "Agree"; and 5: "Strongly agree." Items 11 and 33 are reversely scored. The total scores of the scale and each of its dimensions are 33 - 165 and 11 - 55, respectively. Evaluation of the pre-final PGS-P content validity index (CVI) showed that the CVI of 31 items was higher than 0.79; hence, they were considered appropriate items. The reliability of the scale was assessed using the internal consistency methods. Cronbach's alpha was calculated as 0.95 for the total scale and 0.88, 0.87, and 0.84 for the subscales of active grief, difficulty coping, and despair, respectively (25). The Cronbach's alpha of the scale in the present study was also 0.85.
3.3. Intervention
Study intervention for participants in the intervention group was education about positive ST. During the sessions of the study intervention, participants were invited to interpret their thoughts and emotions and change or strengthen their beliefs (19). Audiovisual education about positive ST was provided in 80 twenty-minute individualized sessions held twice weekly. The first session was held in the study setting, and the remaining 7 sessions were held online using WhatsApp. Patients' questions were also answered during the sessions. Participants in the control group received the care services that were routinely provided to all women with SA in the study setting. All participants completed the study instruments before and 2 months after the intervention through the self-report method. Data collection at post-test was performed at the participants' preferred place, which was either primary healthcare centers near their houses or their houses.
3.4. Data Analysis
Data were analyzed via SPSS v. 16.0 (SPSS Inc., Chicago, IL, USA). Normality was tested through the Shapiro-Wilk test, and within- and between-group comparisons were performed through the paired-sample t-test, independent-sample t-test, and the chi-square test. The level of significance was set to < 0.05.
4. Results
The age mean of participants was 26.40 ± 5.63 years in the intervention group and 24.45 ± 5.11 years in the control group, and most participants in these groups were homemakers (62.5% vs. 65%). Groups did not significantly differ from each other respecting participants' baseline demographic and clinical characteristics (P > 0.05), except gestational age (Table 2), but the variable of gestational age did not show a significant difference between the 2 groups after evaluation by the general linear model test (P = 0.54).
| Sessions | Content |
|---|---|
| 1 | Explaining the regulations and structure of the sessions, explaining the problems and complications of abortion, and providing a general overview of self-talk |
| 2 | Explaining suppressive thoughts when encountering problems and their role in self-talk, discussing different types of thoughts and beliefs, giving assignments |
| 3 | Review of the assignments, training about the elimination of negative internal dialogues and using positive expressions, giving assignments |
| 4 | Review of the assignments, training about positive storytelling, encouraging participants to replace negative factors of life with positive factors, giving assignments |
| 5 | Review of the assignments, training about focusing on the present moment and controlling fears, giving assignments |
| 6 | Review of the assignments, identification of fears and strategies to control them, giving assignments |
| 7 | Review of the assignments, training about focusing on pleasurable moments, and encouragement to start positive self-talk |
| 8 | Review of the previous sessions, drawing conclusions, and emphasizing treating one's self as a friend |
The Content of the Positive ST Educational Sessions
| Group and Characteristic | Intervention | Control | Test Results |
|---|---|---|---|
| Age | 26.40 ± 5.63 | 24.45 ± 5.11 | t = 1.62 b P = 0.10 |
| Number of children | 2.42 ± 2.25 | 2.30 ± 2.12 | t = 0.25 b P = 0.79 |
| Number of abortions | 1.40 ± 1.44 | 1.30 ± 1.88 | t = -0.33 b P = 0.73 |
| Duration of marriage | 4.85 ± 3.46 | 4.55 ± 4.06 | t = -0.35 b P = 0.72 |
| Gestational week | 8.52 ± 3.62 | 6.87 ± 3.20 | t = -2.15 b P = 0.03 |
| Employment status | χ2 = 0.05 c P = 0.81 | ||
| Employed | 15 (37.5) | 14 (35) | |
| Homemaker | 25 (62.5) | 26 (65) | |
| Education level | χ2 = 2.11 c P = 0.54 | ||
| Basic | 13 (32.5) | 8 (20) | |
| Junior high school | 14 (35) | 15 (37.5) | |
| High school diploma | 7 (17.5) | 11 (27.5) | |
| University | 6 (15) | 6 (15) | |
| Intention for pregnancy | χ2 = 0.000 c P = 1.00 | ||
| Intended | 28 (70) | 28 (70) | |
| Unintended | 12 (30) | 12 (30) |
Between-Group Comparisons of the Participants' Demographic and Clinical Characteristics a
The independent-sample t-test indicated no significant between-group difference respecting the pre-test mean score of anxiety (P = 0.745) and grief (P = 0.958). The paired-sample t-test showed that the mean scores of anxiety and grief significantly decreased in both groups, respectively (P < 0.001, P = 0.004), while the amount of decrease in the intervention group was significantly more than the control group (P < 0.05). The post-test mean scores of anxiety and grief in the intervention group were significantly less than the control group (P = 0.001, P = 0.003) (Table 3).
| Outcomes and Group | Time | ||||
|---|---|---|---|---|---|
| Before | After | P-Value b | Mean Difference | P-Value | |
| Anxiety | < 0.001 | ||||
| Control | 6.55 ± 2.61 | 4.57 ± 1.98 | 0.001 | -1.97 ± 1.56 | |
| Intervention | 6.37 ± 2.16 | 2.60 ± 1.59 | 0.001 | -3.77 ± 2.33 | |
| P-value a | 0.745 | 0.001 | - | - | - |
| Grief | 0.004 | ||||
| Control | 63.50 ± 23.65 | 64.85 ± 22.68 | 0.05 | 1.35 ± 5.23 | |
| Intervention | 63.22 ± 22.70 | 50.97 ± 16.22 | 0.01 | -12.10 ± 28.20 | |
| P-value a | 0.958 | 0.003 | - | - | - |
Within- and Between-Group Comparisons Respecting the Mean Scores of Anxiety and Grief
5. Discussion
This study assessed the effects of positive ST on anxiety and grief among women with SA. Findings indicated that positive ST can reduce anxiety among women with SA. We could not find any study in this area for the purpose of comparison. However, a study reported that brief supportive psychotherapy significantly reduced anxiety among women with abortion (26), which is almost in agreement with our findings. Moreover, studies into the effects of educational interventions on anxiety among women with abortion confirmed the effectiveness of these interventions. For example, 2 studies showed that educational counseling had significant positive effects on women's post-abortion anxiety (23, 27). Another study showed that cognitive-behavioral education about stress management significantly reduced anxiety and worry among women with frequent abortions and improved their ability to control their anxious thoughts (28). Moreover, a qualitative study into the women's experiences of post-abortion supportive services found that the provision of specialized care significantly reduced their anxiety over pregnancy (29). Therefore, encouragement of positive ST in counseling and psychotherapy interventions is recommended to improve the effectiveness of abortion management.
Our findings also showed that positive SA significantly reduced grief among women with SA. In line with this finding, a study found that bereavement counseling significantly reduced grief and anxiety among women with late pregnancy loss in India (30). Another study found that educational counseling had positive effects on grief after abortion in the second trimester (27). The results of a review study on 17 clinical trials published between 1995 and 2016 also showed that psychological and supportive interventions can improve mental health among women with a history of miscarriage and, therefore, reduce the negative consequences of pregnancy in later pregnancies. That study also highlighted the necessity of further studies to determine the most effective interventions for mental health improvement among women with a history of miscarriage (31).
The positive effects of positive ST on anxiety and grief in this study can be attributed to the direct relationship of individuals' ST with their behaviors. Through ST, individuals think about their behaviors and interpret and modify them (32). Self-talk also facilitates learning, improves performance and self-confidence, and reduces anxiety (33, 34). A mixed methods study on individuals with cognitive disruption, anxiety, and sadness also showed that participants in anxiety and sadness conditions had greater ST than participants in control conditions (35). Some individuals use negative self-evaluation and repeat disappointing expressions, thereby increasing their anxiety. On the other hand, some individuals have the ability to use ST as a coping strategy to improve their ability to cope with stress and stressful conditions (36).
5.1. Strengths
It seems that no similar study has been conducted on positive ST training and counseling on the anxiety of women with SA, and this is the first study in Iran and other countries on the effects of positive ST on anxiety and grief among women with SA. The satisfaction of the clients showed the necessity of conducting more research.
5.2. Limitations
Due to the COVID-19 pandemic, this study was conducted under special conditions, and all health guidelines were followed.
5.3. Conclusions
This study shows that positive ST can reduce anxiety and grief among women with SA. Nurses are in direct contact with women and are responsible for the improvement of their health and quality of life. Moreover, they are responsible for the delivery of care to women with SA in clinical settings. Therefore, they can prevent the psychological complications of SA and improve the health of women and families. They can use the positive ST educational intervention of this study to prevent SA-associated psychological complications and reduce concern for further pregnancies among women with SA.