1. Background
Uveitis, inflammatory condition of uveal tract (iris, ciliary body, and choroid), is an umbrella term that includes a wide spectrum of etiologies (traumatic, infectious, dysfunction of the immune system or masquerade syndromes) in which the various parts of the eye may be involved (1). It may occur in any age group, from infancy to adulthood, but people in the 2nd-6th decades of life are more susceptible to the disease, and the incidence rate of adults is estimated to be 5 times that of children.
More than two million patients worldwide have uveitis, and it has an estimated incidence of 17 –52/100,000 person-years (2). Approximately 35% of these individuals experience severe visual loss and legal blindness and it is the third leading cause of blindness (approximately 5 – 10% worldwide) (2, 3). The prevalence of phenotypic characteristics and the distribution of different types of uveitis depend on genetics and epidemiological factors such as age, gender, race, socio-economic factors, environmental-geographical influences, diagnostic criteria and diagnostic facilities (4). The epidemiology of non-infectious uveitis is more dependent on racial rather than regional features. Also, the prevalence of a number of causes of uveitis depends on regional conditions. Therefore, demographic characteristics seem to play a prominent role in the incidence and prevalence of uveitis in different societies. In order to prepare a suitable list of differential diagnoses, practitioners classified uveitis on the basis of the anatomical location of involvement (anterior, intermediate, posterior or pan-uveitis), pathology (granulomatous vs. non-granulomatous), laterality (unilateral vs. bilateral), the clinical course (acute, recurrent, or chronic) of the inflammation, and frequency and pattern of uveitis in a certain population. Investigating this is especially important in countries with poor financial resources because it prevents unnecessary diagnostic tests and greatly helps the classification of uveitis, approach, management and treatment of the disease by the physician.
The pattern of uveitis in certain studies is affected by certain factors, and any comparison should be based on these factors. Uveitis patterns may change over time or be affected by diagnostic criteria and study design. In the majority of studies, anterior uveitis is the most common type of involvement, followed by pan uveitis, posterior uveitis, and finally intermediate uveitis (5). However, there are controversies in this issue among different studies and it is highly dependent on the level of patient referral. A systematic review study reported idiopathic uveitis as the prevalent etiology of uveitis in the Iranian population, followed by toxoplasma chorioretinitis, Behcet’s disease (BD), and Fuchs heterochromic iridocyclitis (FHI) (6).
Due to this fact that the etiology and pattern of uveitis are highly distributed in different races on one hand and lack of a comprehensive study to evaluate the epidemiologic pattern of uveitis in western Iran on the other hand encouraged us to design this study.
2. Methods
Given that this research was a descriptive cross-sectional study, the files of all patients diagnosed with uveitis referring to the specialized retina-uveitis clinics in a referral hospital in the west of the country were assessed from April 2016 to October 2022. The current study was approved by the local Ethical Committee of the Kermanshah University of Medical Sciences (code: IR.KUMS.MED.REC.1401.155) and complied with the tenets of the Declaration of Helsinki. Sampling was performed as a census by examining all patients’ files and we have obtained the patients consent to use their information for research purposes. According to the aim of the study, which was to investigate the pattern of uveitis in adults, patients with the age of less than 18 years were excluded from the study.
In this study, demographic factors, clinical examination results, laboratory tests, and complications of uveitis in patients were discussed. The data in the patients’ files were extracted and recorded in a separate checklist regarding the patients’ gender, age, types of uveitis (anterior, intermediate, posterior, and panuveitis), disease course (acute, chronic, and recurrent), and complications of the disease. The Standardization of Uveitis Nomenclature (SUN) criteria were used to classify the disease (7). Based on this, anatomical location of involvement classified in 4 types as following: Anterior, intermediate, posterior and pan-uveitis (Table 1), and in Course’s view, uveitis classified too acute, recurrent and chronic. Incomplete data in some patients’ documents was one of the limitations of the present study. In this case, the patients were called for further information, and they were excluded from the study if their information was still incomplete.
| Category and Descriptor | Comment |
|---|---|
| Anatomical location of involvement | |
| Anterior uveitis | Anterior chamber is the primary site of inflammation. Including: Iritis, Iridocyclitis, and Anterior cyclitis. |
| Intermediate uveitis | Vitreous body is the primary site of inflammation. Including: Pars planitis, Posterior cyclitis, and Hyalitis. |
| Posterior uveitis | Retina or choroid is the primary site of inflammation. Including: Choroiditis (focal, multifocal, or diffuse), Chorioretinitis, Retinochoroiditis, Retinitis, and Neuroretinitis. |
| Panuveitis | Anterior chamber, vitreous body, and retina or choroid involved simultaneously. |
| Course | |
| Acute | Episode characterized by sudden onset and limited duration |
| Recurrent | Repeated episodes separated by periods of inactivity without treatment > 3 months in duration |
| Chronic | Persistent uveitis with relapse in < 3 months after discontinuing treatmen |
The collected data was analyzed using SPSS Version 25 and the results were expressed as mean ± standard deviation. The test of normality or Kolmogorov-Smirnov test was used to check the normal or non-normal distribution of the data. Paired t-test was used to compare the BCVA of patients before-after treatment. Between-group comparisons were performed using one-way analysis of variance (ANOVA) and chi-squared test. The level of statistical significance was set at P < 0.05.
3. Results
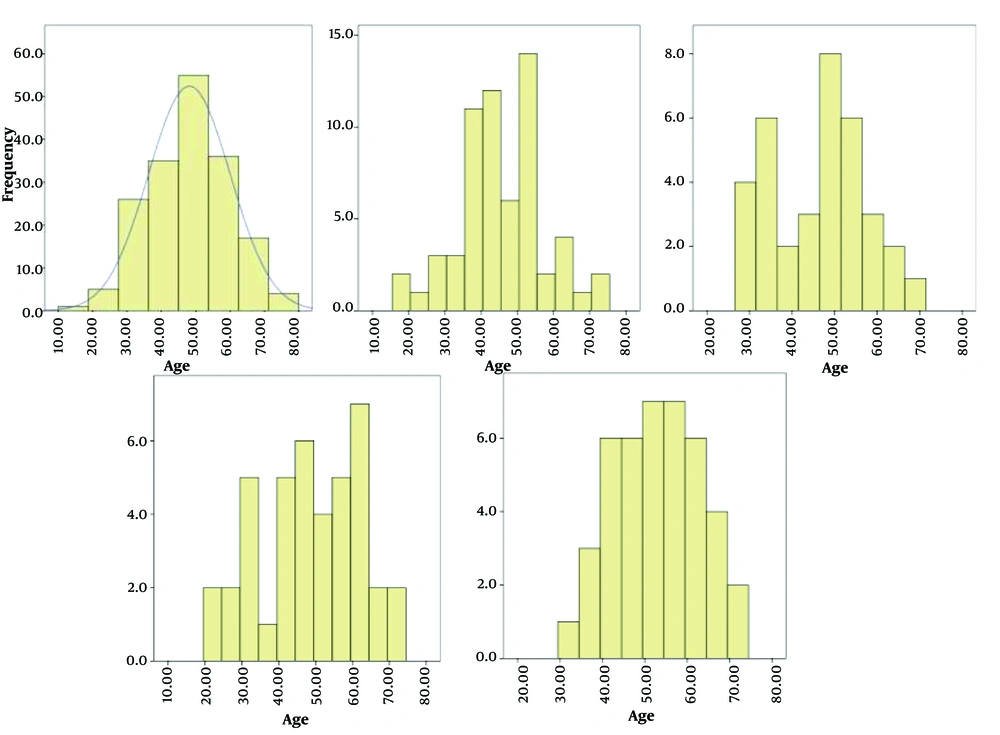
In this study, 552 files of patients with uveitis referring to the specialized retina-uveitis clinic of the …, Iran and specialized clinics affiliated with the … were investigated from April 2016 to October 2022. Among these patients, 194 patients with pediatric uveitis were excluded from the study, and 358 patients’ files were assessed, of whom 170 were female (47.48%) and 188 were male (52.51%). The uveitis patients’ mean age at the diagnosis time was 48.14 years (18 - 72 years) (SD: 11.91); the patients with anterior uveitis had the lowest mean age (45.4 years), and the patients with panuveitis had the highest mean age (52.9 years) at the diagnosis time (Table 2). In general, the involvement in the fifth decade of life was at a maximum level (Figure 1).
| Variables | Ant. Uveitis | Int. Uveitis | Post. Uveitis | Panuveitis | Overall |
|---|---|---|---|---|---|
| Number of Patients | 122 (34) | 70 (20) | 82 (23) | 84 (23) | 358 (100) |
| Female/Male | 62 (51)/60 (49) | 39 (56)/31 (44) | 33 (40)/49 (60) | 35 (42)/49 (58) | 170 (47.48)/188 (52.51) |
| Age | 45.47 ± 11.54 (18 - 72) | 46.28 ± 11.03 (29 - 67) | 48.82 ± 13.60 (22 - 72) | 52.90 ± 10.14 (32 - 72) | 48.14 ± 11.91 (18 - 72) |
| Binocular | 55 (45 | 64 (91) | 42 (51) | 51 (61) | 212 (60) |
| Monocular involvement | 67 (55) | 6 (9) | 40 (49) | 33 (39) | 146 (40) |
| Non-granolomatousis/granulomatousis | 122 (100)/0 (0) | 68 (97)/2 (3) | 74 (90)/8 (10) | 77 (92)/7 (8) | 341 (95)/17 (5) |
| Infectious/Non-infectious | 32 (26.22)/90 (73.77) | 0 (0)/70 (100) | 36 (43.91)/46 (56.09) | 22 (26.19)/62 (73.81) | 90 (25.13)/268 (74.86) |
| Primary BCVA | 0.73 ± 0.53 (0 - 1.85) | 0.68 ± 0.58 (0 - 1.85) | 0.89 ± 0.56 (0 - 1.85) | 0.77 ± 0.63 (0.02 - 2.30) | 0.76 ± 0.58 (0 - 2.3) |
| Last BCVA | 0.24 ± 0.40 (0 - 1.85) | 0.42 ± 0.60 (0 - 2.30) | 0.55 ± 0.70 (0 - 2.30) | 0.63 ± 0.58 (0 - 1.85) | 0.44 ± 0.58 (0 - 2.3) |
Abbreviation: Ant. Uveitis, anterior uveitis; Int. Uveitis, intermediate uveitis; Post. Uveitis, posterior uveitis; SD, standard deviation; BCVA, best corrected visual acuity.
a Values are expressed as No. (%) or mean ± SD (range).
The prevalence of the disease was 53% in males and 47% in females, respectively, which were highly close to each other, and no significant difference was observed between anatomical pattern these two groups (P = 0.129). Although anterior uveitis and intermediate uveitis were slightly more common in females, posterior uveitis and panuveitis significantly involved males.
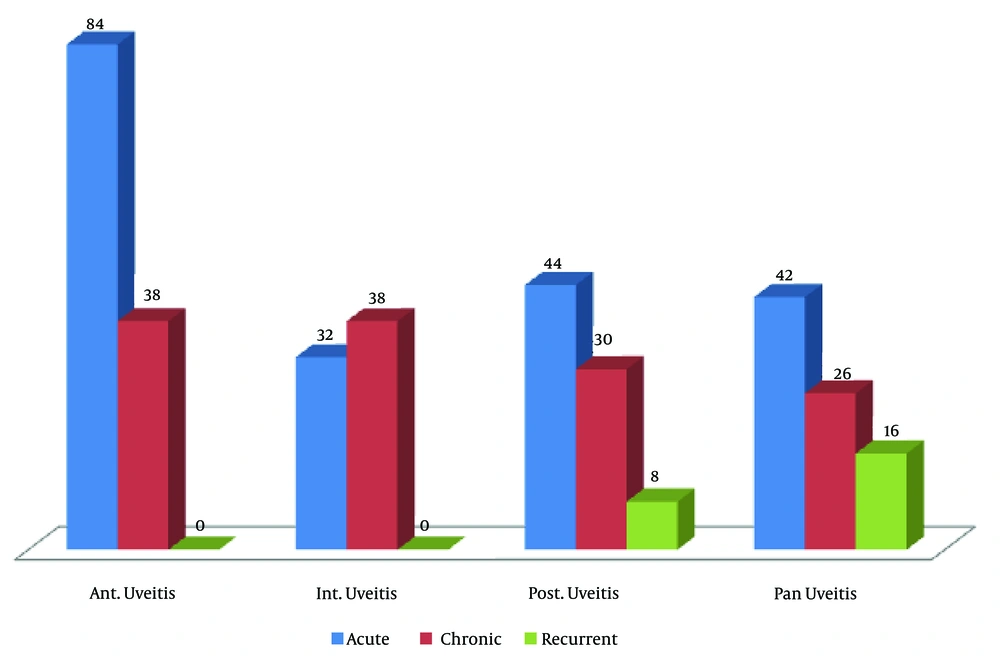
The findings indicated that the most common anatomical pattern of involvement in the west of the country was anterior uveitis (34%), followed by other similar types of uveitis, including panuveitis (23.4%), posterior uveitis (22.9%), and intermediate uveitis (19.5%) (Table 2). In general, most patients with uveitis experienced binocular involvement and difference was significant (P < 0.001) (60% binocular involvement vs. 40% monocular involvement); however, involvement in anterior uveitis was often observed as monocular (55% monocular involvement vs. 45% binocular involvement). On the other hand, monocular involvement in intermediate uveitis scarcely observed in only 9% of the patients (Table 2). Between clinical course and types of uveitis significant difference was observed (P < 0.001). Concerning the clinical course, acute uveitis is generally the most common type of involvement in different types of anterior uveitis (68.85%), posterior uveitis (53.65%), and panuveitis (50%); however, intermediate uveitis involvement is often observed as chronic (54.28%) (Figure 2). Ocular involvement is mainly non-granulomatous, involving 100% of anterior uveitis, 97% of intermediate uveitis, 90% of posterior uveitis, and 92% of panuveitis (P = 0.004) (Table 2). Among 70 patients with intermediate uveitis, only two patients diagnosed with sarcoidosis had granulomatous involvement, and in posterior uveitis, four patients diagnosed with sarcoidosis and four patients diagnosed with tuberculosis (TB) had granulomatous uveitis. Moreover, in panuveitis, five patients out of 84 persons had TB, and two people had sarcoidosis. In all anatomical involvements of uveitis, non-infectious causes were more common than infectious. There was no infectious cause in intermediate uveitis; and posterior uveitis had the most cases of infectious etiology (44%).
Figure 2 clinical course of uveitis in different anatomical types of involvement (Ant. Uveitis: Anterior uveitis, Int. Uveitis: Intermediate uveitis, Post. Uveitis: Posterior uveitis).
The patients’ mean visual acuity at the referral time was 0.76 (SD: 0.58) (0 - 2.3) in general, 0.73 (SD: 0.53) (0 - 1.85) in the anterior uveitis, 0.68 (SD: 0.58) (0 - 1.85) in the intermediate uveitis, 0.89 (SD: 0.56) (0 - 1.85) in posterior uveitis, and 0.77 (SD: 0.63) (0.02 - 2.30) in panuveitis. Furthermore, the patients’ visual acuity at the last referral (after treatment measures) was 0.44 (SD: 0.58) (0 - 2.3) in general and 0.24 (SD: 0.40) (0 - 1.85) in anterior uveitis, 0.42 (SD: 0.60) (0 - 2.30) in intermediate uveitis, 0.55 (SD: 0.70) (0 - 2.30) in posterior uveitis, and 0.63 (SD: 0.58) (0 - 1.85) in panuveitis. After treatment, the patients experienced an overall improvement in visual acuity of 0.32 (P < 0.001, SD: 0.73), and in the subgroup analysis, those patients with anterior and posterior uveitis had an improvement in visual acuity by 0.49 (P < 0.001, SD: 0.67) and 0.34 (P = 0.003, SD: 0.69), respectively. The difference between these two groups was statistically significant; however, despite improvement in visual acuity in intermediate uveitis by 0.26 (P = 0.053, SD: 0.77) and in panuveitis by 0.13 (P = 0.265, SD: 0.76), no statistically significant difference was noticed between them. Accordingly, the best post-treatment visual prognosis belonged to patients with anterior uveitis, and the worst prognosis was for panuveitis.
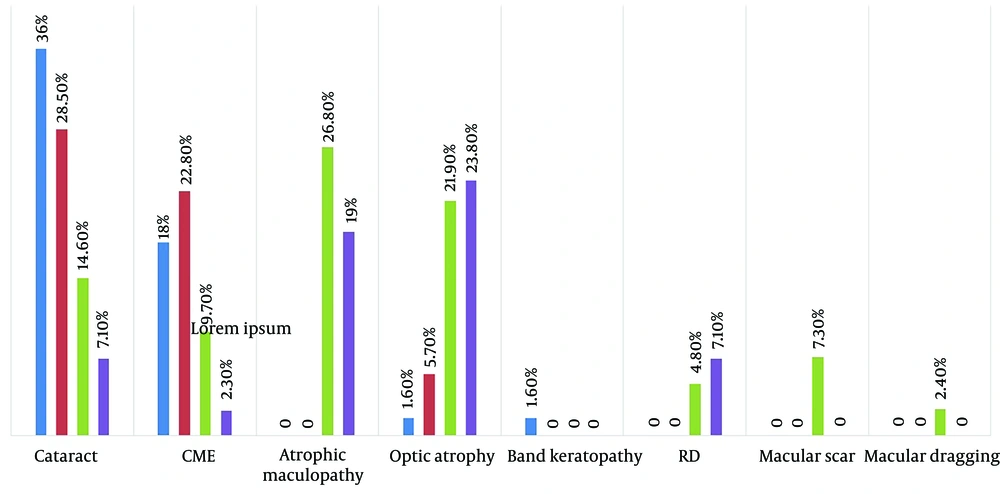
The most common complications of this disease were the cataract formation (in 36% of patients with anterior uveitis and 28.5% of those with intermediate uveitis) and cystoid macular edema (in 22.8% of intermediate uveitis and 18% of anterior uveitis). However, atrophic maculopathy and optic atrophy were more common in posterior uveitis and panuveitis (Figure 3). The rhegmatogenous retinal detachment (RRD) complication was observed only in patients with posterior uveitis and panuveitis and not in those with anterior and intermediate uveitis. This complication was observed in four patients with posterior uveitis (4.87%), two patients with acute retinal necrosis (ARN), two patients with Eales disease, and also six patients with panuveitis (7.14%); all six patients had ARN. Furthermore, two patients with ARN had manifestations of posterior uveitis and got RRD; 10 patients with panuveitis had ARN etiology, of whom six patients got RRD (60%). In general, the risk of RRD in ARN was 66%. Those patients with RRD experienced the worst visual prognosis, and optic atrophy and atrophic maculopathy were then the worst prognosis symptoms, respectively.
According to the findings, the leading causes of uveitis in this center were idiopathic (37.4%) in general, followed by traumatic etiologies (9.49%), Behçet’s disease (9.49%), toxoplasmosis retinochoroiditis (7.82%), Fuchs’ heterochromic iridocyclitis (FHI) (5.58%), and sarcoidosis (3.91%). In this regard, most of ocular involvements had non-infectious etiologies (74.86%). Table 3 presents and describes types of underlying etiologies in detail.
| Type of Uveitis | Ant. Uveitis | Int. Uveitis | Post. Uveitis | Panuveitis |
|---|---|---|---|---|
| Etiologies (%) | Idiopathic (40.98) > traumatic (22.95) > FHI (16.39) > herpetic (9.83) > Behcet’s disease (6.55) > seronegative S.A.= posner-schlossman (1.63) | Idiopathic (60) > MS (11.42) > traumatic = Behcet’s disease (8.57) > sarcoidosis = seronegative SA (5.71) | Toxoplasma chorioretinitis (34.14) > idiopathic (17.07) > serpiginous chorioretinitis (12.19) > sarcoidosis (7.31) > presumed tuberculosis = APMPPE = Behcets’ Syn. (4.87) > SLE = VKH = sympathetic Ophthalmia = ARN = CMV = Eales disease (2.43) | Idiopathic (33.33) > Behcets’ disease (19.04) > ARN (11.90) > VKH (9.52) > endogenous endophthalmitis (7.14) > presumed tuberculosis = sarcoidosis = MCP (4.76) > sympathetic ophthalmia = syphilis (2.38) |
Abbreviation: Ant. Uveitis, anterior uveitis; Int. Uveitis, intermediate uveitis; Post. Uveitis, posterior uveitis; FHI, Fuchs’ heterochromic iridocyclitis; Seronegative S.A., seronegative spondylo arthropathy; MS, multiple sclerosis; APMPPE, acute posterior multifocal placoid pigment choroiditis; SLE, systemic lupus erythematosus; VKH, vogt-koyanagi-harada; ARN, acute retinal necrosis; CMV, cytomegalo virus; MCP, multifocal choroiditis and panuveitis.
The assessment of the anatomical types of involvement revealed the following findings: Idiopathic etiology (40.98%), followed by traumatic (22.95%) and FHI (16.39%) are the most common causes in anterior uveitis ; idiopathic etiology (60%), followed by multiple sclerosis (MS) (11.42%) and traumatic/Behçet’s disease (8.57%), are the most common causes in intermediate uveitis; toxoplasmic chorioretinitis (34.14%), followed by idiopathic (17.07%) and serpiginous chorioretinitis (12.19%), are the most common causes of posterior uveitis; and idiopathic etiology (33.33%), followed by Behçet’s disease (19.04%) and ARN (11.90%), are the most common causes in panuveitis (Table 3).
4. Discussion
As a potential vision-threatening disease, uveitis is considered a diagnostic-therapeutic challenge for ophthalmologists and even uveitis specialists. Epidemiological studies have considerably contributed the literature by revealing involvement patterns and the etiology of the disease in the clinical diagnosis, management, and treatment of these patients. On the other hand, national epidemiological studies can help plan for the future by assessing the disease burden on the community’s health systems. However, there has been limited research on the incidence and prevalence of uveitis in Iran, particularly in the west of the country (6). The clinical pattern of uveitis may change over time because of many reasons, including emerging diseases, new surgical methods inducing uveitis as a surgical complication, and also new laboratory equipment resulting in the better recognition of diseases, their etiology, and better diagnosis in some cases (8-10), as limited diagnostic laboratory equipment in many unprivileged regions can cause diagnostic problems and place some cases of uveitis with specific diagnoses in the idiopathic category (6, 11). This implies that the epidemiological pattern of the disease differs in different societies and may also change over time. This critical issue has been epidemiologically studied in different societies, and the repetition of these studies over time is even important (12). A comparison of their findings not only can help recognize predisposing factors in different societies but also create a new attitude toward the physiopathology of the disease and can direct future studies.
4.1. Demographic Differences
In both developed and developing countries, uveitis is mostly reported in adults (35 - 45 years of age), and no significant difference is observed in terms of gender distribution as an equal distribution between males and females has been reported in most studies. However, sometimes in developing countries, the distribution of involvement is higher in males; however, the reason is unknown and may involve exposure patterns in agricultural societies or differences in inclination to seek medical care (13, 14).
4.2. Anatomical Distribution of Uveitis Involvement
Posterior uveitis is more common in developing countries, the high prevalence of which is associated with infectious factors such as toxoplasmosis (Brazil), TB (India), onchocerciasis (Africa), and the higher prevalence of non-infectious factors such as Behçet syndrome and Vogt-Koyanagi-Harada (VKH), which first involve the posterior segment (15-17). Moreover, given the continuation of the acquired immunodeficiency syndrome (AIDS) epidemic in developing countries and the patients’ longer life span with a decreased CD4 count, retinal cytomegalovirus (CMV) is more often observed (18).
4.3. Infectious Uveitis
Infectious uveitis is caused by many factors; however, infectious uveitis is more common in the developing world (30 - 50%). Furthermore, the prevalence of certain infectious factors such as TB and toxoplasmosis is higher in the developing world, whereas other factors such as leprosy, leptospirosis, and onchocerciasis are observed rarely. In developed countries, infectious factors account for 11 - 21% of uveitis cases, most of which are associated with toxoplasmosis and the herpes family, followed by TB, syphilis, and Lyme (19). Developed countries have endemic infectious factors not found in developing countries (e.g., histoplasmosis in the Mississippi River and Borrelia in the American and European regions) (20, 21). Socioeconomic conditions also play a critical role in the distribution of uveitis in developing countries, where poverty, large populations, and malnutrition can promote infection. Furthermore, cysticercosis, toxoplasmosis, and leptospirosis are associated with contaminated water, air, and soil (15, 22).
From another perspective, the spread of AIDS in a community directly affects the distribution of uveitis. Immune system suppression, infection promotion, and research on individuals with human immunodeficiency virus (HIV) suggest that such individuals are more frequently involved in retinal CMV and retinal toxoplasmosis (18). Also, in this context, the emergence of new infectious diseases that cause ocular inflammatory conflicts should also be considered (23).
4.4. Non-infectious Uveitis
The leading causes of non-infectious uveitis, including Fuchs Hetrochromic Iridoclitis and human leukocyte antigen (HLA)-B27-related uveitis, sarcoidosis, traumatic uveitis, VKH disease, lens-induced uveitis, multifocal choroiditis and panuveitis, serpiginous choroiditis, Behçet’s disease, idiopathic intermediate uveitis, and juvenile idiopathic arthritis, occur in both developed and developing countries (1, 24).
Of the highest prevalence of uveitis secondary to sarcoidosis has been reported in the United States, Japan, and the Netherlands (25).
Behçet’s disease is common along the Silk Road, the Far East, and the Mediterranean region, and it is more common in studies conducted in Turkey, China, Japan, Saudi Arabia, and Iran. Vogt-Koyanagi-Harada disease is more common in Asia and Eurasian countries, suggesting that Behçet’s and VKH diseases are uncommon in Western countries (26).
Birdshot chorioretinopathy is mostly common in Western countries and among European patients and has not been observed in studies conducted in China and other Asian countries (9). Researchers believe that this difference is associated with genetics. Several HLAs have been discovered, which are linked to specific diseases such as HLA-A29 to birdshot chorioretinopathy, HLA-B51 to Behçet’s disease, HLA-DR4 to VKH, sympathetic ophthalmia, HLA-B8, and HLA-B13 to sarcoidosis (27).
Lens-induced traumatic uveitis is mainly observed in developing countries and is more associated with socioeconomic factors and the quality of treatment (28, 29).
4.5. Middle East
According to research in Iran investigating 544 patients, the most common cause of uveitis is idiopathic intermediate uveitis (15%), uveitis secondary to diseases such as toxoplasmosis (10%), Behçet’s disease (9%), heterochromatic iridocyclitis (7%), VHK (4 %), and sarcoidosis (4%), Eale’s disease, and ocular toxocariasis are observed in 2% of the population (30).
Turkey has the highest prevalence of Behçet’s disease worldwide, and following idiopathic uveitis, Behçet uveitis is the most common cause of uveitis in Turkey, which is observed in 26 - 32% of the patients. Among other common causes of uveitis are rheumatic diseases (9%) and toxoplasmosis (7.3%) (31). A study in Saudi Arabia showed idiopathic acute anterior uveitis (29% - 32%) and herpetic uveitis (12% - 15%) as the most common types of uveitis. Moreover, uveitis secondary to TB was relatively common in 8 - 11% of the patients (31). In this study, the patients’ mean age was 48.14 years, with the higher involvement of males (52.51%). The most common anatomical pattern of involvement was anterior uveitis (34%), followed by panuveitis (23.4%), posterior uveitis (22.9%), and intermediate uveitis (19.5%). The most common clinical characteristics in the patients were binocular involvement (60%) (compared to monocular involvement), non-granulomatous uveitis (95.53%) (compared to granulomatous type), and non-infectious uveitis (compared to infectious type). In general, the most common etiology was idiopathic disease (37.4%), followed by traumatic (9.49%), Behçet’s disease (9.49%), toxoplasmosis retinochoroiditis (7.82%), and FHI (5.58%). Furthermore in the subgroup analysis, the most common etiologies in the cases of anterior uveitis were idiopathic (40.98%), traumatic (22.95%), FHI (16.39%), and herpes (9.83%); idiopathic (60%), MS (11.42%), Behçet’s disease (8.57%), and traumatic (8.57%) in the cases of intermediate uveitis (60%); toxoplasmosis retinochoroiditis (34.14%), idiopathic (17.07%) and serpiginous chorioretinitis (12.19%) in the cases of posterior uveitis; and idiopathic (33.33%), Behçet’s syndrome (19.04%), ARN (11.90%), and VKH (9.52%) in the cases of panuveitis (33.33%). All previous studies have investigated the uveitis pattern of involvement in ophthalmology referral centers; thus, so their findings may not be generalizable to the general population because of the obvious differences in the disease patterns among the third-level referral cases, general ophthalmology, and the general public (6).
In line with the present study, most global reports have indicated that anterior uveitis is the most common pattern of involvement in these patients, followed by panuveitis, posterior uveitis, and intermediate uveitis. In a similar vein, most studies were conducted in ophthalmology referral centers, and their findings cannot be generalized to the general population. Under such conditions (investigating referred patients), a higher prevalence of posterior uveitis and panuveitis and a lower proportion of anterior uveitis would be expected (31). Several epidemiological factors may influence the disease pattern, so these differences should be considered in making comparisons. Regional-based epidemiological studies would help not only in diagnosis but also in treatment guidance. This case is particularly essential for developing countries such as Iran due to limited resources on the one hand as well as the higher prevalence of certain specific etiologies of uveitis (compared to developed countries), and the higher complications of the disease and even blindness on the other hand (31).
The main limitation of the present study was to investigate the epidemiological pattern of the disease based on the findings in the ophthalmology referral center. To the best of our knowledge, this pattern is different from that of the general population and patients at lower referral levels. In contrast, the strength of this study was to examine the epidemiological pattern of the disease in the west of the country for the first time.
4.6. Conclusions
The predominant pattern of involvement in patients referring to the referral center in the west of the country was anterior uveitis, acute and non-granulomatous in terms of anatomical location, clinical course and pathology of involvement, respectively. This clinical view to evaluation in a referral center differs from the pattern expected to be observed in the general population and even in general ophthalmology centers.
According to an extensive search, no study has assessed the epidemiological pattern of uveitis in the general population of Iran yet. Moreover, no study has evaluated this issue at the general ophthalmology clinical level, and all reports have been associated with ophthalmology referral centers. Accordingly, future studies are suggested to evaluate the epidemiology of this disease at the community level and assess of the general ophthalmology activity. The results of these studies can differ from what we observed at high referral levels. It is also recommended to conduct complementary studies on the epidemiology and etiology of pediatric uveitis and investigate etiology-based treatment processes.