1. Background
Mental and physical health of an individual is affected by interaction of the mind and body through the central and peripheral nervous system (1). Executive function is the neurocognitive process of the brain for problem-solving and decision-making, which involves multiple neural networks, such as the thalamus, basal ganglia, and prefrontal cortex (2). It is posited to be highly associated with mentally-stimulating activities, which declines with age (3). Some studies have proven increased hyperintense regions in the subcortical white matter in Magnetic Resonance Imaging (MRI) as an index of impaired memory performance and executive function (4).
The executive function is impaired in several physical, neurologic, and neuro-psychopathologic diseases, such as hypoperfusion-related cerebral lesions (5), gait disorders (6), cardiovascular and atherosclerotic disease (7), Parkinson (8), Attention Deficit Hyperactivity Disorder (ADHD) (9), delirium (10), autism (11), and suicidal attempts (12).
Executive function refers to a network of top-down mental processes, sometimes known as an umbrella for various complex cognitive processes, which are critically dependent on the frontal cortex. This ability involves complex cognitions, such as working memory, inhibition, emotional control, and mental flexibility (1, 2, 4). Therefore, assessment of executive function requires validated tools. Nevertheless, there seems to be a variety of tests, which have their own advantages and disadvantages; Delis-Kaplan Executive Function System has been introduced as an appropriate tool for frontal-lobe functions (13). Kettle test was introduced as the shortest post-stroke measurement tool of executive function, while it falls short in assessment of executive function in other neuro-psychologic diseases (14). As hypothesized, the target population plays a significant role in selection of the appropriate tool (15). Hence, validation of a tool that could be used for the general population seems necessary.
A more feasible tool for evaluating the everyday behavioral manifestations of executive dysfunction is the Behavior Rating Inventory of Executive Function (BRIEF), designed for children aged 5 to 18 years (16), which is completed by parents or teachers (17). The adult version, named Behavior Rating Inventory of Executive Function-Adult version (BRIEF-A), with two forms of self-report and informant-report, was developed in 2005 by Roth and colleagues (18).
A few studies have introduced BRIEF as the most sensitive measure of executive function, each on a different target populations, including obese patients suffering from binge eating disorder (19), patients with substance use disorder (20), neuropsychiatric patients (21), and schizophrenia (22). However, studies evaluating BRIEF-A have declared complexity in assessment of executive function and have suggested that feasibility of BRIEF-A has to be evaluated for different cultures and target populations (20, 21).
Since a validated and reliable Persian version (Iranian native language) of this questionnaire does not exist, the present study aimed at determining the validity and reliability of the Persian version of BRIEF-A.
2. Materials and Methods
2.1. Study Population
The study population consisted of all employees, staff, and students of Shiraz University of Medical Sciences and teachers and staff of the Education Department of Juyom, Larestan, Fars province. The sample was calculated as three-times the BRIEF-A’s number of items, which was 225, according to the study’s statistician; thus, 318 cases with the inclusion criteria were randomly selected from the study population, to increase the reliability of the results. The inclusion criteria included age of between 18 and 65 years, agreement to complete the test, self- report of having no sign of psychiatric problems and any medical condition, which might have negative effects on cognition, and General Health Questionnaire (GHQ) score of less than 6. All the participants completed the following tools.
2.2. Measurement Tools
The general health questionnaire-28 (GHQ-28), designed by Goldberg (23), is an indicator of mental health that evaluates psychiatric morbidity in 4 subscales, including somatization, anxiety, social dysfunction, and depression. Based on how the person felt recently, each item could be answered using a 4-point Likert scale. The questionnaire could be completed in 10 to 12 minutes and GHQ-28 scores higher than 6 indicated severe psychiatric disorder. Iranian studies have also determined a high reliability (Cronbach’s alpha of 0.87 to 0.97) for the Persian version (24-26).
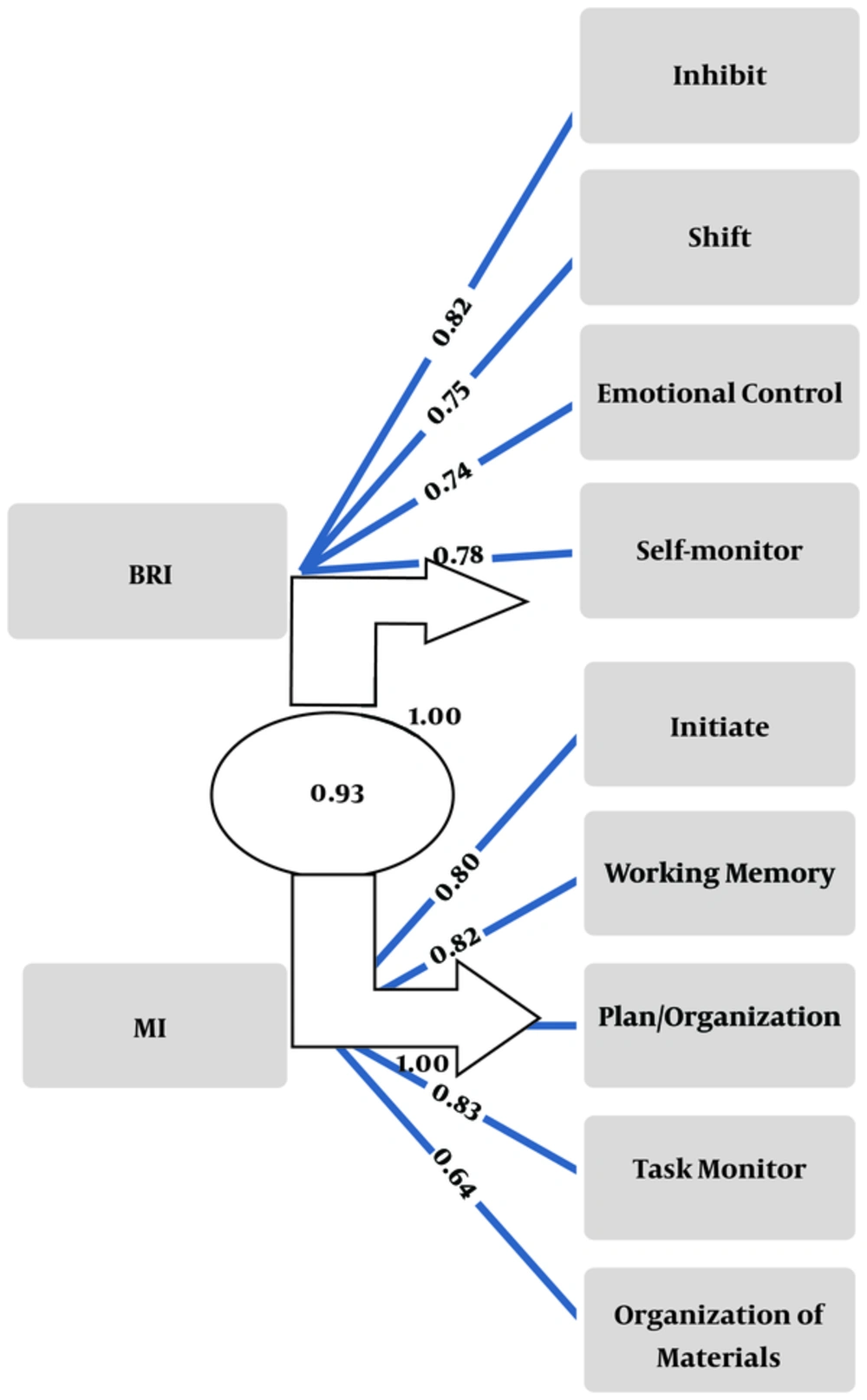
Behavior Rating Inventory of Executive Function-Adult version (BRIEF-A), designed by Roth et al. (18), evaluates the everyday behavioral manifestations of executive dysfunction. The self-report form of BRIEF-A is composed of 75 items in 9 different clinical scales, including 2 aspects of the Behavioral Regulation Index (BRI), composed of inhibit (8 questions), shift (6 questions), emotional control (10 questions), and self-monitor (6 questions) and meta-cognitive index (MI), composed of initiate (6 questions), working memory (8 questions), plan/organize (10 questions), task monitor (6 questions), and organization of material (8 questions), which are scored using 3 options (never, sometimes, and often). Sum of the total scores represents Global Executive Composite (GEC). In the scoring system, more than 14 unanswered questions were considered unreliable results and scores of the subscales were not calculated when more than one item in the “shift, self-monitor, and task monitor” and more than two in the rest of subscales were unanswered. If the scale is measurable, the unanswered items receive a score of 1. It also has three validity scales, including negativity, infrequency, and inconsistency, scored separately. Each form of BRIEF-A takes about 15 minutes.
2.3. Study Design
Test Preparation: Before providing BRIEF-A to the participants, the original questionnaire (English version) was separately translated to Persian by 2 psychiatrists and 3 psychologists and changed to a uniform translation after being discussed in an expert meeting. Then, it was edited and reviewed by a Farsi literature expert. Finally, the final version was rechecked with the original English text (back translation) for validity. A sample of 20 non-psychiatric patients, who referred to Imam Reza clinic (during 6 days) were selected, who completed the questionnaire under the researcher’s observation. All comments of these participants or any change in this phase was consulted with the experts. An observer was present when participants were completing the forms, in order to answer their questions. Finally, if the participant could not complete the questions, the scoring system (mentioned above) was used. It should be mentioned that this validation sample (20 participants) was not included in the final analysis.
Content validity: According to the BRIEF-A manual and executive function theory, the scale content was confirmed by the researchers.
Face validity: Five separate psychiatrists besides the researchers checked and confirmed the final version of the test.
Besides, as mentioned previously, the final version of the test was administered on a normal sample to confirm its content and face validity.
In the beginning, participants were asked to complete (GHQ-28) and only participants, who obtained a score of less than 6 were included in the study. The 318 participants answered the Farsi version of the BRIEF-A.
2.4. Ethical Considerations
The protocol of the study was approved by Shiraz University of Medical Sciences. The design and objectives of the study were explained to all participants and verbal informed consent was obtained from those, who were willing to participate in the study and they were ensured about confidentiality of their information.
2.5. Statistical Analysis
Results were presented as mean ± Standard Deviation (SD) for quantitative variables. For the statistical analysis, with a significance level of 0.05, the SPSS statistical software version 21.0 for windows (SPSS Inc., Chicago, IL) was used. Analysis of variance was used to compare mean differences among groups and the LSD test was used for group comparisons of post hoc test, and correlation coefficients were used for assessing the relationship of variables. Internal consistency was evaluated by Cronbach’s alpha and reliability was determined in a random sample of 60 participants of the staff of Shiraz University Medical Sciences during one month by dependent binary tests with significant level of 0.95. For calculating the validity, the LISREL software version 8.8 was used though factor analysis with Varimax, by which the fitness of domains were determined.
3. Results
Among 318 participants, 30% were males and 70% were females. Mean ± SD of participants’ age was 31.89 ± 8.4 years and nearly half of the participants (45.9%) were in the age group of 18 to 29 years, 35.2% in 30 to 39 years, 15.4% in 40 to 49 years, and 3.5% in 50 to 59 years age group. Considering the educational level, 12.3% of participants were high school graduates, 7.2% had associate degrees, 60.7% had a bachelor’s degree, 16.7% had a master’s degree, and 3.1% had doctorate.
The scores in different subscales between male and female participants, as demonstrated in Table 1, shows that the only significant difference between male and female participants were related to shift and emotional control, in which females obtained a significantly higher score. Also, a significant decrease in subscale scores associated with increase in age categories was observed in inhibit, initiate, plan/organization, task monitor, MI, and GEC (Table 1). The results of LSD post-hoc test showed that significant differences were found mostly between the participants in the first and third decade of life.
The percentage of scores based on the age category and gender is demonstrated in Table 2, which means that, for example, a participant aged 35 with an inhibit score of 7.5 had obtained a score, which is lower than 95% of the participants in the same age range.
Cronbach’s alpha was used to estimate internal consistency for BRIEF-A subscales, and the scores were as follows: inhibit α = 0.693, shift α = 0.774, emotional control α = 0.838, self-monitor α = 0.704, and initiate α = 0.717, working memory α = 0.775, plan/organize α = 0.795, task monitor α = 0.650, and organization of material α = 0.781. Test-retest reliability was determined in a random sample of 60 participants during one month, the results showed that there were no significant differences between the two evaluations (P = 0.78); besides, the Pearson correlation coefficients between first and second (one month later) BRIEF were significant in all dimensions (P < 0.001). This means that the scale was reliable during the time and these two evaluations had no significant differences and were significantly the same.
The correlation matrix between the subscales and total scale scores of BRIEF-A are demonstrated in Table 3.
Results of factor analysis by using LISREL to compute factor components of fitness evaluation of the BRIEF-A model factors showed comparative and non-normed fit index of 0.095, standardized root mean of 0.064, and root mean square error of approximation square residual of 0.051 for 9 areas (75 questions) with a p-value of 0.01, and was calculated separately for BRI/MI, which resulted in 0.98, 0.034, and 0.088, respectively with a p-value of 0.001. Table 4 shows items in each factor and Figure 1 represents the model of goodness of fit of the BRIEF-A in Persian.
| Participants’ Gender | Participants’ Age Category | |||||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | P-Value | 18 - 29 Years | 30 - 39 Years | 40 - 49 Years | 50 - 59 Years | P-Value | |
| Inhibit | 12.77 ± 3.05 | 12.65 ± 2.65 | 0.72 | 13.24 ± 2.85 | 12.45 ± 2.73 | 11.83 ± 2.34 | 11.54 ± 2.65 | 0.004 |
| Shift | 9.52 ± 2.31 | 10.21 ± 2.55 | 0.021 | 10.29 ± 2.62 | 9.75 ± 2.38 | 9.73 ± 2.15 | 9.81 ± 3.28 | 0.300 |
| Emotional control | 16.20 ± 3.88 | 17.35 ± 4.00 | 0.018 | 17.21 ± 4.23 | 17.01 ± 3.81 | 16.81 ± 3.74 | 14.81 ± 3.48 | 0.285 |
| Self-monitor | 9.25 ± 2.24 | 9.46 ± 2.20 | 0.440 | 9.63 ± 2.22 | 9.33 ± 2.32 | 8.93 ± 1.90 | 8.90 ± 2.16 | 0.221 |
| Initiate | 12.73 ± 2.69 | 12.64 ± 2.98 | 0.790 | 13.08 ± 3.02 | 12.63 ± 2.81 | 11.79 ± 2.47 | 11.36 ± 2.61 | 0.020 |
| Working memory | 12.19 ± 2.92 | 12.28 ± 2.96 | 0.797 | 12.71 ± 2.94 | 11.97 ± 3.03 | 11.55 ± 2.56 | 12.27 ± 3.22 | 0.062 |
| plan/organize | 14.69 ± 3.65 | 14.92 ± 3.42 | 0.590 | 15.43 ± 3.70 | 14.69 ± 3.31 | 13.65 ± 2.86 | 14.09 ± 3.67 | 0.014 |
| Task monitor | 9.63 ± 2.12 | 9.70 ± 2.70 | 0.791 | 10.16 ± 2.08 | 9.43 ± 2.07 | 8.89 ± 1.74 | 9.18 ± 2.27 | 0.001 |
| Organization of material | 12.28 ± 3.15 | 11.81 ± 2.82 | 0.190 | 12.25 ± 3.05 | 12.04 ± 2.99 | 11.22 ± 2.44 | 10.54 ± 1.86 | 0.065 |
| BRI | 47.75 ± 9.46 | 49.69 ± 9.68 | 0.098 | 50.39 ± 10.12 | 48.57 ± 9.39 | 47.32 ± 8.10 | 45.09 ± 10.30 | 0.089 |
| MI | 61.54 ± 12.38 | 61.38 ± 11.91 | 0.906 | 63.65 ± 12.41 | 60.78 ± 11.89 | 57.12 ± 9.87 | 57.54 ± 11.70 | 0.005 |
| GEC | 109.29 ± 21.02 | 111.05 ± 20.40 | 0.481 | 114.04 ± 21.51 | 109.35 ± 19.97 | 104.44 ± 16.96 | 102.54 ± 21.37 | 0.014 |
| Percentile → | 5 | 10 | 25 | 50 | 75 | 90 | 95 | |
|---|---|---|---|---|---|---|---|---|
| Age and sex category↓ | ||||||||
| Inhibit | 18 - 29 years | 8.35 | 9.00 | 11.00 | 13.00 | 15.00 | 17.00 | 18.00 |
| 30 - 39 years | 8.00 | 9.00 | 10.00 | 12.00 | 14.00 | 16.00 | 17.00 | |
| 40 - 49 years | 9.00 | 9.00 | 10.00 | 11.00 | 13.00 | 15.00 | 16.00 | |
| 50 - 59 years | 8.00 | 8.00 | 10.00 | 10.00 | 14.00 | 14.00 | ||
| Male | 8.00 | 9.00 | 10.00 | 12.50 | 15.00 | 17.00 | 19.00 | |
| Female | 8.00 | 9.00 | 11.00 | 13.00 | 15.00 | 16.00 | 17.00 | |
| Shift | 18 - 29 years | 6.00 | 7.00 | 8.00 | 10.00 | 12.00 | 14.00 | 15.00 |
| 30 - 39 years | 6.00 | 7.00 | 8.00 | 10.00 | 11.00 | 12.00 | 14.00 | |
| 40 - 49 years | 6.00 | 7.00 | 8.00 | 9.00 | 11.00 | 13.00 | 14.00 | |
| 50 - 59 years | 6.00 | 6.00 | 7.00 | 10.00 | 12.00 | 15.00 | ||
| Male | 6.00 | 7.00 | 8.00 | 9.00 | 11.00 | 13.00 | 14.05 | |
| Female | 6.00 | 7.00 | 8.00 | 10.00 | 12.00 | 13.00 | 14.00 | |
| Emotional control | 18 - 29 years | 11.00 | 17.00 | 14.00 | 17.00 | 20.00 | 23.00 | 24.00 |
| 30 - 39 years | 10.00 | 12.00 | 14.00 | 17.00 | 20.00 | 22.00 | 23.00 | |
| 40 - 49 years | 10.00 | 12.00 | 14.00 | 17.00 | 19.00 | 22.00 | 23.00 | |
| 50 - 59 years | 10.00 | 10.20 | 12.00 | 15.00 | 17.00 | 20.00 | ||
| Male | 10.00 | 11.00 | 13.75 | 16.00 | 19.00 | 22.00 | 23.05 | |
| Female | 11.00 | 12.00 | 14.00 | 17.00 | 20.00 | 22.00 | 24.00 | |
| Self-monitor | 18 - 29 years | 9.00 | 9.00 | 10.75 | 13.00 | 15.00 | 17.00 | 18.65 |
| 30 - 39 years | 8.00 | 9.00 | 10.00 | 12.00 | 15.00 | 16.00 | 18.00 | |
| 40 - 49 years | 8.00 | 9.00 | 10.00 | 11.00 | 13.00 | 16.00 | 16.50 | |
| 50 - 59 years | 8.00 | 8.00 | 10.00 | 10.00 | 13.00 | 16.00 | ||
| Male | 6.00 | 6.00 | 7.00 | 9.00 | 11.00 | 12.00 | 13.00 | |
| Female | 6.00 | 7.00 | 8.00 | 9.00 | 11.00 | 12.00 | 13.00 | |
| Initiate | 18 - 29 years | 9.00 | 9.00 | 10.75 | 13.00 | 15.00 | 17.00 | 18.65 |
| 30 - 39 years | 8.00 | 9.00 | 10.00 | 12.00 | 15.00 | 16.00 | 18.00 | |
| 40 - 49 years | 8.00 | 9.00 | 10.00 | 11.00 | 13.00 | 16.00 | 16.5 | |
| 50 - 59 years | 8.00 | 8.00 | 10.00 | 10.00 | 13.00 | 16.00 | ||
| Male | 9.00 | 10.00 | 10.00 | 12.00 | 15.00 | 16.00 | 17.05 | |
| Female | 8.00 | 9.00 | 10.00 | 12.00 | 15.00 | 17.00 | 18.00 | |
| Working memory | 18 - 29 years | 8.00 | 9.00 | 10.00 | 12.50 | 15.00 | 16.00 | 18.00 |
| 30 - 39 years | 8.00 | 8.00 | 9.00 | 12.00 | 14.75 | 16.00 | 17.00 | |
| 40 - 49 years | 8.00 | 8.00 | 10.00 | 11.00 | 13.50 | 16.00 | 16.50 | |
| 50 - 59 years | 8.00 | 8.00 | 10.00 | 11.00 | 15.00 | 17.60 | ||
| Male | 9.00 | 10.00 | 10.00 | 12.00 | 15.00 | 16.00 | 17.05 | |
| Female | 8.00 | 9.00 | 10.00 | 12.00 | 15.00 | 17.00 | 18.00 | |
| Plan/organize | 18 - 29 years | 10.00 | 11.00 | 12.75 | 15.00 | 18.00 | 20.00 | 22.65 |
| 30 - 39 years | 10.00 | 11.00 | 12.00 | 14.00 | 17.00 | 20.00 | 21.00 | |
| 40 - 49 years | 10.00 | 11.00 | 11.00 | 13.00 | 16.00 | 18.00 | 19.50 | |
| 50 - 59 years | 10.00 | 10.20 | 11.00 | 13.00 | 16.00 | 21.80 | ||
| Male | 10.00 | 11.00 | 12.00 | 14.00 | 17.00 | 20.10 | 22.05 | |
| Female | 10.00 | 11.00 | 12.00 | 15.00 | 17.00 | 20.00 | 20.95 | |
| Task monitor | 18 - 29 years | 7.00 | 7.70 | 9.00 | 10.00 | 11.25 | 13.00 | 14.00 |
| 30 - 39 years | 6.00 | 7.00 | 8.00 | 9.00 | 11.00 | 12.00 | 13.00 | |
| 40 - 49 years | 6.50 | 7.00 | 8.00 | 8.00 | 10.00 | 11.00 | 12.50 | |
| 50 - 59 years | 6.00 | 6.20 | 8.00 | 8.00 | 12.00 | 12.80 | ||
| Male | 6.95 | 7.00 | 8.00 | 10.00 | 11.00 | 13.00 | 14.00 | |
| Female | 7.00 | 7.00 | 8.00 | 10.00 | 11.00 | 12.00 | 13.00 | |
| Organization of material | 18 - 29 years | 8.00 | 8.00 | 10.00 | 12.00 | 15.00 | 16.00 | 18.00 |
| 30 - 39 years | 8.00 | 9.00 | 9.00 | 12.00 | 14.00 | 16.00 | 17.00 | |
| 40 - 49 years | 8.00 | 9.00 | 9.00 | 11.00 | 13.00 | 15.00 | 16.00 | |
| 50 - 59 years | 8.00 | 8.20 | 9.00 | 10.00 | 12.00 | 13.80 | ||
| Male | 8.00 | 8.00 | 10.00 | 12.00 | 14.25 | 17.00 | 18.05 | |
| Female | 8.00 | 8.00 | 9.00 | 12.00 | 14.00 | 16.00 | 16.00 | |
| BRI | 18 - 29 years | 32.70 | 37.00 | 43.00 | 50.00 | 59.00 | 63.30 | 67.00 |
| 30 - 39 years | 33.65 | 35.00 | 42.00 | 48.00 | 55.75 | 61.00 | 65.35 | |
| 40 - 49 years | 34.00 | 37.00 | 42.00 | 46.00 | 54.50 | 60.00 | 61.50 | |
| 50 - 59 years | 30.00 | 30.20 | 37.00 | 45.00 | 52.00 | 59.00 | ||
| Male | 32.95 | 35.00 | 41.00 | 47.00 | 55.00 | 60.10 | 65.00 | |
| Female | 33.05 | 37.00 | 43.00 | 50.00 | 58.00 | 61.00 | 65.95 | |
| MI | 18 - 29 years | 44.35 | 47.00 | 56.00 | 63.00 | 72.25 | 80.30 | 85.65 |
| 30 - 39 years | 44.65 | 46.00 | 51.25 | 58.50 | 70.75 | 78.00 | 81.00 | |
| 40 - 49 years | 44.50 | 47.00 | 50.00 | 55.00 | 66.00 | 72.00 | 75.00 | |
| 50 - 59 years | 43.00 | 43.30 | 46.00 | 55.00 | 67.00 | 77.60 | ||
| Male | 45.00 | 47.00 | 51.00 | 60.00 | 70.25 | 79.00 | 84.20 | |
| Female | 44.00 | 46.00 | 52.00 | 60.00 | 71.00 | 78.00 | 81.95 | |
| GEC | 18 - 29 years | 79.40 | 85.00 | 98.00 | 113.50 | 129.00 | 143.00 | 149.00 |
| 30 - 39 years | 79.00 | 84.30 | 94.25 | 107.50 | 123.00 | 138.70 | 145.00 | |
| 40 - 49 years | 80.00 | 85.00 | 91.50 | 99.00 | 121.50 | 130.00 | 131.00 | |
| 50 - 59 years | 74.00 | 74.20 | 83.00 | 105.00 | 124.00 | 135.60 | ||
| Male | 78.95 | 84.90 | 91.75 | 106.50 | 124.00 | 139.10 | 147.05 | |
| Female | 78.05 | 85.00 | 92.25 | 110.00 | 126.75 | 138.90 | 144.00 |
| Inhibit | Shift | Emotional Control | Self-Monitor | Initiate | Working Memory | Plan/Organize | Task Monitor | Organization of Material | BRI | MI | GEC | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Inhibit | 10.00 | 0.557 | 0.624 | 0.655 | 0.607 | 0.634 | 0.643 | 0.646 | 0.521 | 0.842 | 0.726 | 0.819 |
| Shift | 0.557 | 10.00 | 0.600 | 0.542 | 0.592 | 0.654 | 0.645 | 0.573 | 0.342 | 0.793 | 0.672 | 0.765 |
| Emotional control | 0.624 | 0.600 | 10.00 | 0.587 | 0.571 | 0.533 | 0.532 | 0.534 | 0.422 | 0.885 | 0.618 | 0.776 |
| Self-monitor | 0.655 | 0.542 | 0.587 | 10.00 | 0.540 | 0.584 | 0.647 | 0.618 | 0.511 | 0.803 | 0.692 | 0.781 |
| Initiate | 0.607 | 0.592 | 0.571 | 0.540 | 10.00 | 0.689 | 0.683 | 0.639 | 0.536 | 0.689 | 0.848 | 0.819 |
| Working memory | 0.634 | 0.654 | 0.533 | 0.584 | 0.689 | 10.00 | 0.699 | 0.692 | 0.462 | 0.708 | 0.846 | 0.827 |
| Plan/organize | 0.643 | 0.645 | 0.532 | 0.647 | 0.683 | 0.699 | 10.00 | 0.725 | 0.608 | 0.722 | 0.899 | 0.865 |
| Task monitor | 0.646 | 0.573 | 0.534 | 0.618 | 0.639 | 0.692 | 0.725 | 10.00 | 0.524 | 0.698 | 0.8340. | 0.815 |
aCorrelation is significant at 0.01 (2-tailed)
| Question Number | The Question | Coefficient Correlation With the Scale | P-Value | |
|---|---|---|---|---|
| Inhibit | 5 | I tap my fingers or bounce my legs | 0.513 | 0.001 |
| 16 | I have trouble sitting still | 0.555 | 0.001 | |
| 29 | I have problems waiting my turn | 0.640 | 0.001 | |
| 36 | I make inappropriate sexual comments | 0.385 | 0.001 | |
| 43 | I make decisions that get me into trouble (legally, financially, socially) | 0.630 | 0.001 | |
| 55 | People say that I am easily distracted | 0.575 | 0.001 | |
| 58 | I rush throw things | 0.581 | 0.001 | |
| 73 | I am impulsive | 0.616 | 0.001 | |
| Shift | 8 | I have trouble changing from one activity or task to another | 0.576 | 0.001 |
| 22 | I have trouble accepting different ways to solve problems with work, friends or tasks | 0.662 | 0.001 | |
| 32 | I have trouble thinking of the different way to solve a problem when stuck | 0.692 | 0.001 | |
| 44 | I am bothered by having to deal with changes | 0.749 | 0.001 | |
| 61 | I get disturbed by unexpected changes in my daily routine | 0.702 | 0.001 | |
| 67 | After having a problem, I don’t get over it easily | 0.729 | 0.001 | |
| Emotional control | 1 | I have angry outbursts. | 0.466 | 0.001 |
| 12 | I overreact emotionally | 0.617 | 0.001 | |
| 19 | I have emotional outburst for little reason | 0.711 | 0.001 | |
| 28 | I react more emotionally to situation than my friend | 0.627 | 0.001 | |
| 33 | I overreact to small problems | 0.711 | 0.001 | |
| 42 | I get emotionally upset easily | 0.627 | 0.001 | |
| 51 | My anger is intense but ends quickly | 0.710 | 0.001 | |
| 57 | People say that I am too emotional | 0.599 | 0.001 | |
| 69 | My mood changes frequently | 0.678 | 0.001 | |
| 72 | I get upset quickly or easily over little things | 0.723 | 0.001 | |
| Self-monitor | 13 | I don’t notice when I cause others to feel bad or get mad until it is too late | 0.600 | 0.001 |
| 23 | I talk at the wrong time | 0.654 | 0.001 | |
| 37 | When people seem upset with me I don’t understand why | 0.555 | 0.001 | |
| 50 | I say things without thinking | 0.723 | 0.001 | |
| 64 | People say that I don’t think before acting | 0.644 | 0.001 | |
| 70 | I don’t think about consequences before doing something | 0.650 | 0.001 | |
| Initiate | 6 | I need to be reminded to begin a task even when I am willing | 0.496 | 0.001 |
| 14 | I have trouble getting ready for the day | 0.647 | 0.001 | |
| 20 | I lie around the house a lot | 0.444 | 0.001 | |
| 25 | I have problems getting started on my own | 0.682 | 0.001 | |
| 45 | I have difficulty getting excited about things | 0.515 | 0.001 | |
| 49 | I have trouble getting started on tasks | 0.739 | 0.001 | |
| 53 | I start things at the last minute (such as assignments, chores, tasks) | 0.635 | 0.001 | |
| 62 | I have trouble coming up with ideas for what to do with my free time | 0.515 | 0.001 | |
| Working memory | 4 | I have trouble concentrating on tasks(such as chores, reading, or work) | 0.640 | 0.001 |
| 11 | I have trouble with jobs or tasks that have more than one step | 0.626 | 0.001 | |
| 17 | I forget what I am doing in the middle of things | 0.559 | 0.001 | |
| 26 | I have trouble staying on the same topic when talking | 0.641 | 0.001 | |
| 35 | I have a short attention span | 0.657 | 0.001 | |
| 46 | I forget instructions easily | 0.679 | 0.001 | |
| 56 | I have trouble remembering things, even for a few minutes(such as directions, phone numbers) | 0.572 | 0.001 | |
| 68 | I have trouble doing more than one thing at a time | 0.619 | 0.001 | |
| Plan/organization | 9 | I get overwhelmed by large tasks | 0.487 | 0.001 |
| 15 | I have trouble prioritizing activities | 0.676 | 0.001 | |
| 21 | I start tasks (such as cooking, projects) without the right materials | 0.418 | 0.001 | |
| 34 | I don’t plan ahead for future activities | 0.642 | 0.001 | |
| 39 | I have unrealistic goals | 0.516 | 0.001 | |
| 47 | I have good ideas but cannot get them on paper | 0.500 | 0.001 | |
| 54 | I have difficulty finishing a task on my own | 0.671 | 0.001 | |
| 63 | I don’t plan ahead for tasks | 0.640 | 0.001 | |
| 66 | I have problems organizing activities | 0.711 | 0.001 | |
| 71 | I have trouble organizing work | 0.669 | 0.001 | |
| Task monitor | 2 | I make careless errors when completing tasks. | 0.474 | 0.001 |
| 18 | I don’t check my work for mistakes | 0.448 | 0.001 | |
| 24 | I misjudge how difficult or easy tasks will be | 0.600 | 0.001 | |
| 41 | I make careless mistakes | 0.621 | 0.001 | |
| 52 | I have trouble finishing tasks (such as chores, work) | 0.742 | 0.001 | |
| 75 | I have problems completing my work | 0.748 | 0.001 | |
| Organization of material | 3 | I am disorganized. | 0.675 | 0.001 |
| 7 | I have a messy closet | 0.656 | 0.001 | |
| 30 | People say that I am disorganized | 0.689 | 0.001 | |
| 31 | I lose things (such as keys, money, wallet, homework, etc) | 0.638 | 0.001 | |
| 40 | I leave the bathroom a mess | 0.466 | 0.001 | |
| 60 | I leave my room or home a mess | 0.697 | 0.001 | |
| 65 | I have trouble finding things in my room, closet or desk | 0.712 | 0.001 | |
| 74 | I don’t pick up after myself | 0.494 | 0.001 |
4. Discussion
The present study indicated that the BRIEF-A is a reliable and valid scale in the Persian language. Its reliability was evaluated by test-retest and Cronbach’s alpha methods, which confirmed this psychometric characteristic, according to acceptable coefficients ranging between 0.65 and 0.84. Validity characteristics were confirmed according to different methods, content and face validity were evaluated at the first step of the research as scale preparation, and factor analysis method was used to confirm factors of the scale in the Persian version.
Different studies have validated the BRIEF-A inventory in different target populations, including patients suffering from binge eating disorder (19, 27), patients with substance use disorder (20), neuropsychiatric patients (21), and schizophrenia (22), and have suggested that the BRIEF-A inventory is an appropriate tool in measuring different aspects of executive function, including emotional impairments and social functioning (20). Further studies have confirmed that BRIEF-A is sensitive to mild cognitive impairment (28). In addition, studies have suggested that BRIEF-A is a standard tool for treatment response in patients with ADHD and Parkinson’s disease (29, 30).
As posited, the 3 factorial model of BRIEF-A is considered an appropriate method by several studies (31, 32); Roth and colleagues performed a factor analysis on 524 healthy young adults, determining 14% fitness for metacognition factor, 19% for behavioral regulation factor (inhibit and self-monitor scales), and 24% for the emotional regulation factor (emotional control and shift scales) (32). In the present study, likewise, a high Cronbach’s alpha and fitness for MI and BRI were proven for the Persian version of BRIEF-A. Thus, due to the complexity of interpretation of the 9 subscales, evaluation of scores of MI, BRI, and GEC seem appropriate.
In the present study, in addition to confirming a high validity and reliability for the Persian version of BRIEF-A, the current research was able to categorize most scores according to participant’s age (Table 2), which identifies the score of one patient compared to other participants in the same age range, and could help better interpretation of the obtained score. According to this table, for example, a participant aged 35 with an inhibit score of 7.5 has obtained a score, which is lower than 95% of the participants in the same age range. This table could reduce the complexity of the scores’ interpretation and help clinicians explore the participants’ score faster and easier. In addition, this study calculated the coefficient correlation of each question, categorized by their included subscale, which gives the researchers a detailed view through reliability of each question in the Persian version.
The present study had several strengths, including a large sample of homogenous participants with a high educational level for validation of the Persian version of BRIEF-A, which limited the effect of confounding factors, like IQ level of participants that has been posited to impact BRIEF-A scores (33). In addition, only psychologically and physically healthy participants were enrolled in the study to prevent the confounding effect of diseases on the BRIEF-A subscales. On the other hand, the current study was not exempt from limitations. One of the limitations of the present study included the female dominancy of participants that could affect the results of the study. Moreover, it was not possible to compare the results with the informant-report form of BRIEF-A, even though, studies have determined low or moderate correlation between the self- and informant-report BRIEF-A and have posited less sensitivity of informant-report BRIEF-A in disorders (28). In addition, most studies focusing on BRIEF-A have utilized the self-report form (22, 30). Therefore, it seems that self-report BRIEF-A is sufficient, yet further studies are required to compare clinical differences in the self- and informant-report form of the Persian version of the BRIEF-A inventory.
In conclusion, the present study determined high validity and reliability for the Persian version of BRIEF-A and designed tables for a better interpretation of scores in different subscales of BRIEF-A inventory that could guide clinicians with using this questionnaire for assessment of executive function. Besides, by presenting the percentile scores, the clinician could estimate these cognitive function compared to their age group. More studies are necessary to evaluate BRIEF-A validity among psychiatric and neurologic patients.