1. Context
HIV/AIDS (acquired immunodeficiency syndrome) is a life-threatening condition (1) and a significant global public health challenge (2, 3). According to 2022 statistics by UNAIDS, approximately 39 million people globally are living with HIV (4), with 86% aware of their status (3). Additionally, 630,000 individuals died from HIV-related causes, and there were 1.3 million new infections in 2022 (3). The term transgender encompasses individuals whose gender identity, expression, or behavior does not conform to the sex assigned to them at birth (5). Often, transgender people encounter numerous obstacles, including stigma, discrimination, and social exclusion based on their gender identity and expression (6, 7), as well as heightened risks of mental health issues, physical violence, and economic challenges (7). This group is particularly susceptible to HIV (8), with a study in the United States from 2009 to 2014 showing that 11% of transgender adults were receiving HIV medical care (9). In a systematic review and meta-analysis by Stutterheim et al., examining 98 studies, the laboratory-confirmed HIV prevalence was found to be 14.1% among transgender women and 3.2% among transgender men (10). This review also highlighted that the overall standardized HIV prevalence throughout the epidemic, adjusted for country and year, was 19.9% among trans-feminine individuals and 2.56% among trans-masculine individuals (10). Another study indicated that transgender women are over 48 times more likely to contract HIV than the general adult population of reproductive age (11). Various studies have assessed the knowledge, attitudes, and practices of transgender people regarding HIV in different regions of the world (12). However, the aspect of risk perception, a key element of the health belief model (HBM) (13), which predicts health-related behaviors and informs interventions to modify HIV acquisition risks like substance use, alcohol consumption, and unprotected sex, has received comparatively less attention in the literature than other HBM components (14).
2. Objectives
This review aims to investigate the perceived risk, knowledge, attitudes, and practices concerning HIV/AIDS among the transgender population.
3. Methods
This study was a systematic review conducted from December 2, 2020, to December 15, 2021. It aimed to assess the knowledge, attitudes, practices, and risk perceptions towards HIV/AIDS among transgender populations, employing the HBM as a theoretical framework to understand the factors influencing HIV/AIDS-related behaviors and beliefs in this group.
3.1. Search Strategy
The research involved searching four online databases: Scopus, PubMed, Web of Science (ISI), and Google Scholar, using keywords such as ‘HIV’, ‘AIDS’, ‘knowledge’, ‘attitudes’, ‘practices’, ‘behavior’, ‘action’, ‘risk perception’, ‘perceived risk’, ‘risk susceptibility’, ‘severity perception’, ‘perceived self-efficacy’, ‘cues to action’, ‘benefit’, ‘barrier’, ‘health belief model’, ‘sexually transmitted disease’, ‘sexually transmitted infection’, ‘alcohol’, ‘drugs’, ‘amphetamine’, ‘opium’, ‘trans’, ‘transgender’, ‘transsexual’, ‘gender dysphoria’. An illustrative example of a search strategy in the PubMed database is provided for clarity:
(((HIV OR AIDS) AND (knowledge OR attitudes OR practices OR behavior OR action OR risk perception OR perceived risk OR risk susceptibility OR severity perception OR perceived self-efficacy OR cues to action OR benefit OR barrier OR health belief model)) AND (sexually transmitted disease OR sexually transmitted infection OR alcohol OR drugs OR amphetamine OR opium)) AND (trans OR transgender OR transsexual OR gender dysphoria).
Exclusion criteria included non-English papers and gray literature, which were not accessible or applicable to this study's researchers.
3.2. Screening
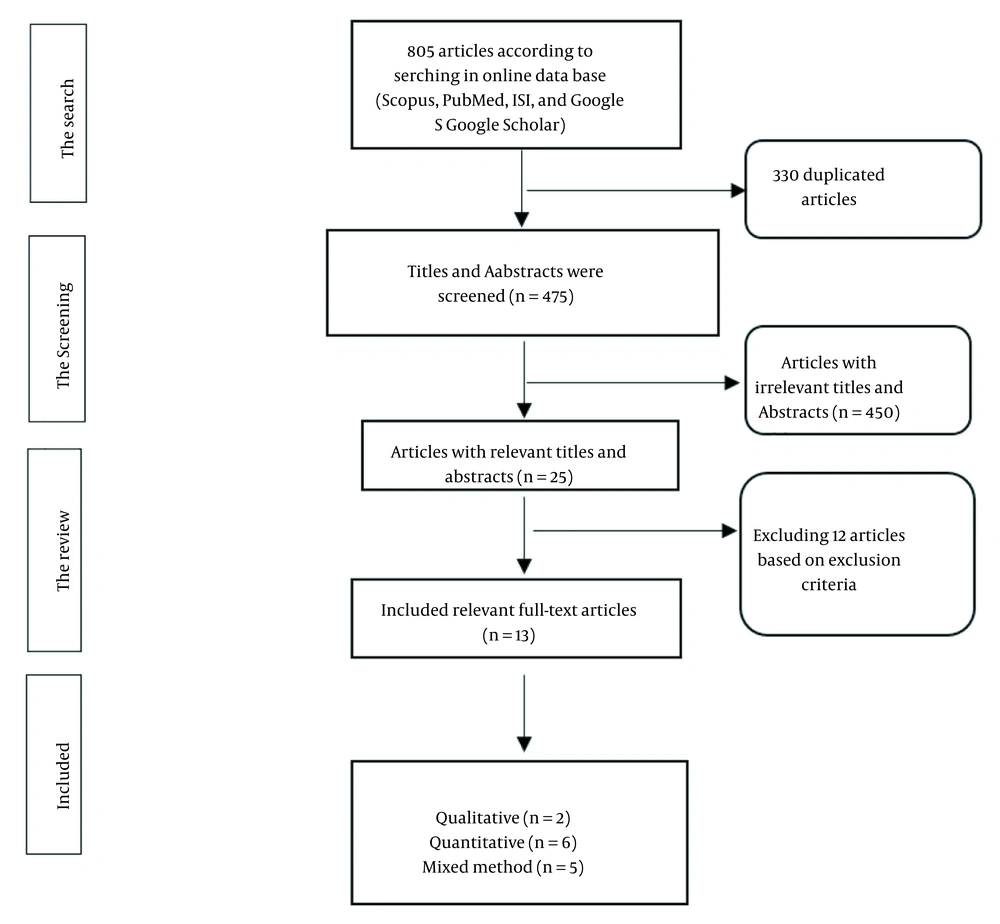
Screening was carried out by two independent authors, with a third author's opinion resolving any disagreements. The article selection process is depicted in Figure 1. Initially, the titles of all articles were reviewed to remove duplicates. Then, the abstracts of the remaining articles were examined for relevance to the study's subject. Lastly, full texts of studies deemed highly relevant were reviewed and considered for the quality assessment phase. It is important to note that the article selection was not restricted by publication date.
3.3. Quality Assessment
The quality of the selected studies was evaluated using two recognized checklists: The STROBE (strengthening the reporting of observational studies in epidemiology) checklist (15) and the COREQ (consolidated criteria for reporting qualitative research) (16). Although there is no universally accepted quality scoring system for grading articles based on various quality measures (17), we implemented a scoring system as follows: Each checklist item fulfilled by the selected articles was scored as 1, and those not fulfilled were scored as 0. Subsequently, we classified the studies' quality according to the following criteria: Over 70% of the checklist items met (level A), between 40% - 70% met (level B), and less than 40% met (level C). Articles from groups A and B were included in this study, while those in group C were excluded.
4. Results
An initial library of 805 articles was compiled using Endnote X7.1 software, comprising 114 papers from ISI, 107 from Scopus, 28 from PubMed, and 556 from Google Scholar. After identifying and removing 330 duplicates, 475 articles remained. Subsequent review of titles and abstracts led to the exclusion of 450 studies deemed irrelevant. Of the 25 articles that underwent full-text review, 12 were excluded based on the exclusion criteria, leaving 13 articles for inclusion in the review (Figure 1).
Among the 13 selected articles for this review, two were qualitative, six quantitative, and five utilized mixed methods. Of the quantitative studies, five were cross-sectional, and one was longitudinal.
4.1. Demographic Characteristics of Selected Papers
In total, the 13 articles encompassed studies of 3 271 individuals, averaging 251 participants per study, with the smallest and largest sample sizes being 11 and 1 270, respectively. The ages of the transgender participants studied were 18 years and older (Table 1).
| Author/ Year of Publication/ (Reference) | Title | Sample | Gender (m/f) | Mean Age, year | Place, Country | Ethnicity | Study Design |
|---|---|---|---|---|---|---|---|
| Andrinopoulos et al. 2015 (18) | Evidence of the negative effect of sexual minority stigma on HIV; testing among MSM1 and transgender women in San Salvador, El Salvador | 670; MSM = 506; TW = 164 | MSM/TF | Range: (18 - 24/25 - 65) | San Salvador, USA | ND | Cross-sectional |
| De Santis et al. 2017 (19) | HIV risk perception, HIV knowledge, and sexual risk behaviors among transgender women in South Florida | 50 | MTF | 38.44 | South Florida, USA | 18% Black, 36% Caucasian, 46% Hispanic/Latino | Cross-sectional |
| Fisher et al. 2018 (20) | Perceived barriers to HIV prevention services for transgender youth | Totally: 228; TM: 103; TF: 93; gender non binary: 32 | TF/TM | 17.86 | USA | 12.3% Hispanic, 87.7% White, 5.7% Black, 3.9% Asia/Pacific Islander, 4.8% American Indian/Alaskan | Cross-sectional |
| Golub et al. 2013 (21) | The Impact of anticipated HIV stigma on delays in HIV testing behaviors: Findings from a community-based sample of men who have sex with men and transgender women in New York City | 305 | MSM/TF | 33 | New York City, USA | 32.1%Black, 25.9% Latino, 34.4% White, 7.5% of other ethnicities | Cross-sectional |
| Hoagland et al. 2017 (22) | High pre-exposure prophylaxis uptake and early adherence among men who have sex with men and transgender women at risk for HIV Infection: The PrEP6 Brazil demonstration project | Total: 1270; 738 eligible | MSM/TF | Median: 30 | Rio de Janeiro and São Paulo, Brazil | 12.7% Black, 54% White, 32.2% Mix-black, and Asian (white, black, mixed-black, native, Asian) were categorized as white, black, and mixed | Prospective, longitudinal, open-label; demonstration study |
| Kenagy et al. 2005 (23) | The risk less known: Female-to-male transgender persons’ vulnerability to HIV infection | 184; MTF: 122; FTM: 762 | MTF/FTM | 32.46 | Philadelphia, USA | 56.2%African American, 33.3% Caucasian, 35.0% of other ethnicities | A qualitative study |
| Poteat, et al. 2019 (24) | A gap between willingness and uptake: Findings from mixed methods research on HIV prevention among black and latina transgender women | 201 | TF (BLTW) | 38.2 (range: 19 - 82) | Baltimore, MD Washington, DC, USA | 125 participants were Black/African American, 35 were multi-racial, and 22 the other races (Indigenous, Latina/Hispanic) | Mixed methods study |
| Reisner et al. 2009 (25) | HIV risk and social networks among male-to-female transgender sex workers in Boston, Massachusetts | 11 | MTF | 34.6 | Boston, USA | 36.4% participants were Hispanic/Latina, 27.3% Black/African American, 36.4% White/Caucasian | Mixed methods study |
| Reisner et al. 2017 (26) | Perceived barriers and facilitators to integrating HIV prevention and treatment with cross-sex hormone therapy for transgender women in Lima, Peru | 48 TW | TF/Male and female | HP9: 39.1; TSW: 29.1 | Lima, Peru | Almost half of all TW participants were born in Lima, Peru | Mixed methods study |
| Rodriguez-Madera and Toro-Alfonso 2005 (27) | Gender as an obstacle in HIV/AIDS prevention: Considerations for the development of HIV/AIDS prevention efforts for male-to-female transgenders | 50 | MTF | 27 | Puerto Rico | 50 MTF Puerto Rican transgenders participated, and they lived in the metropolitan area of San Juan. | Mixed methods study |
| Scheim and Travers 2017 (28) | Barriers and facilitators to HIV and sexually transmitted infections testing for gay, bisexual, and other transgender men who have sex with men | 40 | Trans “MSM” | Age: 18 and above | Ontario, Canada | Ten participants were Aboriginal/ Indigenous, 33 of them Racialized, non-aboriginal, 58 of them White, and 70 of them lived in Toronto. | A qualitative study |
| Sevelius 2009 (29) | ''there's no pamphlet for the kind of Sex I have'': HIV-related risk factors and protective behaviors among transgender men who have sex with no transgender men | 45 | Trans “MSM” | 18 - 60 | USA | 82.2% of White, 11.1% Latino, 2.2% African American, 2.2% American Indian, 2.2% multiracial. | Mixed methods study |
| Setia et al. 2006 (30) | Men who have sex with men and transgender in Mumbai, India: An emerging risk group for STIs10 and HIV | Totally: 150; MSM: 122; TS: 28 | MSM/TS | TS: 25.3; MSM: 23.6 | Mumbai, India | Mumbai, India | Cross-sectional |
Abbreviations: MSM, men who have sex with men; TW, trans woman; ND, Non-determined; TF, trans feminine; MTF, male -to- female; TM, trans masculine; PrEP, pre-exposure prophylaxis; FTM, female-to-male; BLTW, black and Latina transgender women; HP, healthcare professional; STIs, sexually transmitted infections.
Five papers (30%) focused on trans females (TFs), female-to-male (FTMs), or transgender women (TW), three papers (23%) targeted male to female (MTFs), and two studies (15.4%) were conducted among trans men who have sex with men (MSMs). The rest of the studies included a mix of MTFs, FTMs, transsexuals (TSs), or trans males/females (TF/TMs). Eight of the studies (61.5%) were conducted in the United States, with the remaining taking place in Rio de Janeiro and Sao Paulo (Brazil), Lima (Peru), Puerto Rico, Ontario (Canada), and Mumbai (India) (Table 1). Regarding the ethnicity of the target populations, the majority were identified as black, African, or mixed black groups, with a smaller representation of Alaskan, Peruvian, and Puerto Rican groups (Table 1).
4.2. Findings Based on HBM Components
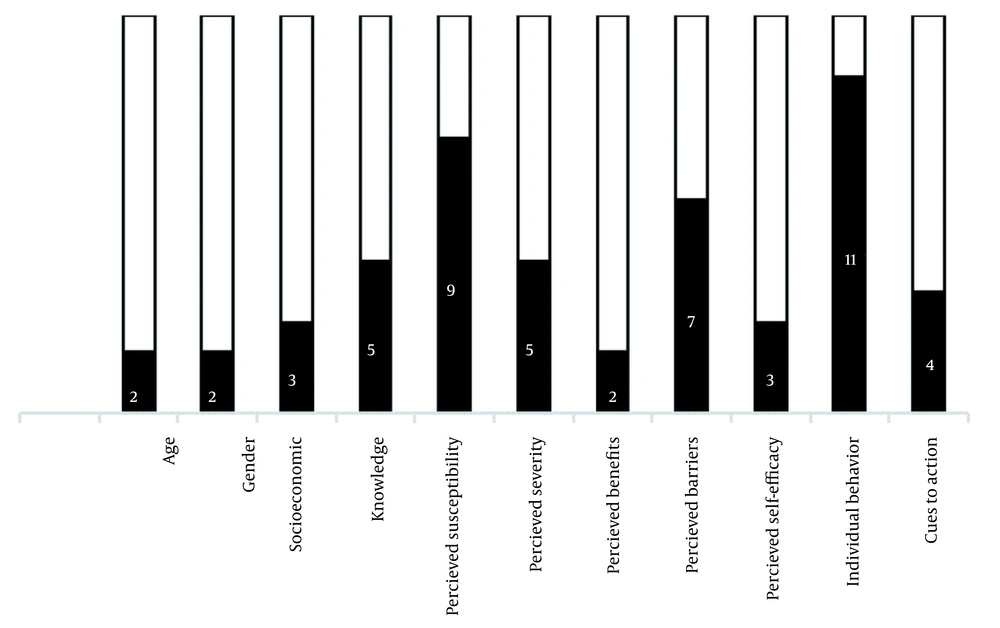
Findings based on HBM components was shown in Figure 2.
4.2.1. Modifying Factors
4.2.1.1. Age
In two studies (15.4%), the willingness to undergo HIV testing was associated with age (18, 21). Andrinopoulos et al. identified a direct correlation between age and HIV testing (18), whereas another study observed an inverse relationship (21).
4.2.1.2. Gender
A positive correlation was found between undergoing HIV testing and identifying as a TW (18). Additionally, a significant association was noted between gender identity and HIV infection risk among participants (23).
4.2.1.3. Socioeconomic Status
Three studies discussed factors related to socioeconomic status (18, 25, 27). Andrinopoulos et al. reported a positive association between HIV testing and earning over $251 per month (18). A common reason for engaging in sex work, as reported in most participant responses, was financial necessity (25). Rodríguez-Madera and Toro-Alfonso noted that 74% of MTFs were involved in the sex industry as a source of income (27) (Table 2).
| Author/Year of Publication/(Reference) | Findings | Conclusions and Recommendations |
|---|---|---|
| Andrinopoulos et al. 2015 (18) | Experience of sexual assault, older age, knowing a PLHIV, and perceiving that most social acquaintances had tested were positively associated with ever testing. Homelessness and ever testing had a negative association. | More researches among TWs are needed. Social networks could be an effective way to engage TW and MSM in interventions and HIV-testing centers. |
| De Santis et al. 2017 (19) | Low HIV-perceived risk and low knowledge regarding HIV risk/transmission were reported in TWs. High-risk sexual behaviors were detected in some individuals. Prognostic factors of sexual risk behaviors were identified. | For studying the connected factors of sexual risk behaviors among TW, widespread research is needed. Determination of HIV perceived risk and HIV knowledge and establishment of relevant education to TW was recommended for nurses to decrease sexual risk. |
| Fisher et al. 2018 (20) | Because of the expected GSM stigma and fright of being "outed” to parents, TG youth may not share their GSM identity or sexual health issues with PCPs. | PCPs should care about transgender-inclusive training to target youths’ sexual health needs and personal concerns thoughtfully. |
| Golub et al. 2013 (21) | 32% of individuals had not ever tested for HIV. Anticipated stigma and risk perception were negatively associated. Anticipated stigma, risk perception, and younger age were the significant predictors of HIV testing. | The potential of a significant influence of the social norms around HIV testing and PrEP may be identified as an anti-HIV stigma action addressing HIV-negative participants for a different attitude toward HIV prevention. |
| Hoagland et al. 2017 (22) | The eligible but not enrolled individuals were younger and less awarded for PrEP and had lower HIV perceived risk. Unprotected receptive anal sex and higher drug levels were positively associated. | PrEP interventions were successful for MSM6 and TGW. The need for strategies to promote perceived risk and PrEP knowledge among the younger and less educated ones is highlighted. |
| Kenagy et al. 2005 (23) | Compared to MTFs, FTMs had significantly more likeliness for engagement in recent high-risk sexual behaviors. Even after controlling for demographic variables, AIDS knowledge, perceived AIDS knowledge, perceived effectiveness of condom usage, perceived susceptibility to AIDS, and self-esteem, the gender difference existed. | HIV-related education is necessary to select sexual activities in FTMs carefully. The need for counseling on safe sex behaviors is highlighted, and they should be encouraged to be tested for HIV. Understanding TG’s lives is required to design effective HIV prevention strategies. More qualitative studies are necessary to design quantitative instruments for assessing HIV risk among TG. |
| Poteat et al. 2019 (24) | HIV-positive was among 56% of BLTW, and PrEP was heard by them. Only 18% who had heard of PrEP had ever taken it. The willingness to take PrEP was in 75% of the 72 self-reported HIV-negative or status-unknown BLTW who had never taken PrEP. A positive association was found between the history of exchange sex and willingness to take PrEP. The likelihood of willingness to take PrEP was negatively associated with more excellent HIV knowledge and TG pride. The most significant barrier to taking PrEP was the concern about "drug interactions" with "hormone therapy." | Further studies and interventions should target PrEP engagement and structural barriers that limit access and give the insurance of community-led, empowering, and affirming approaches. |
| Reisner et al. 2009 (25) | The prevalence of HIV-infected participants was 33%. | Results show that interventions with MTF sex workers must be at multiple levels and address the psychosocial and environmental contexts in which sexual risk behavior occurs. Research on HIV and AIDS should be based on recognizing at-risk groups and personal and social influencing factors on risky behaviors. |
| Reisner et al. 2017 (26) | A high perceived acceptability of the integrated care model was found among TW and healthcare professionals alike. Stigma, lack of provider training or Peruvian guidelines regarding optimal TW care, and service delivery obstacles were included as barriers. | The hiring of TW staff was identified as a critical facilitator for engagement in health care. Future research should identify factors that foster positive and trusting relationships between TW and their healthcare providers. Detection of perceived barriers and facilitators toward getting HIV/AIDS is healthful for upcoming interventions for ignoring the care of TWs in Peru. |
| Rodriguez-Madera and Toro-Alfonso 2005 (27) | Composing of the young unemployed and uneducated population was a qualitative analysis. The need for essential health and social services and alienation from social networks was reported. | The obstacles to HIV prevention efforts among these communities are social vulnerability, institutional exclusion, and gender construction issues. Important elements related to social vulnerability among TS, such as lack of social and institutional support, cannot be overlooked. Furthermore, greater attention is given to gender construction issues and their role in HIV prevention efforts designed for the MTF community. |
| Scheim and Travers 2017 (28) | Several barriers to HIV and other STI testing were described. Trans-specific and general difficulties in accessing sexual health services, lack of trans health knowledge among testing providers, and limited and a perceived gap between trans-inclusive policies and their implementation were included in practice. | Access to trusted and flexible testing providers and integration of testing with ongoing monitoring for hormone therapy were identified as two significant facilitators. Based on these findings, we recommend enhanced access to HIV and STI testing for this key population. |
| Sevelius 2009 (29) | HIV prevalence was found to be 2.2%. Barriers to sexual negotiation, such as unequal power dynamics, low self-esteem, and the need for gender identity affirmation, were included as risk factors. Meeting and negotiating with potential partners online were included as protective strategies. | Current risk behaviors could increase HIV prevalence rates among trans-MSM. Discrimination approaches in primary care services for white and non-white transgender people should be addressed in further research. More information is suggested about how best to meet the prevention and service needs of trans-MSM and their non-trans male partners. |
| Setia et al. 2006 (30) | 68% of the TGs were HIV infected. Consistent condom use during receptive anal sex in the past six months was only 27%. A positive association was found in HIV infection in TGs in univariate analysis. | A strong association was found between prior STI and HIV infection in MSM and TGs. These groups should be the reduction of risky sexual behavior and promotion of HIV counseling and testing. Intervention programs should be culturally sensitive and highlight the need to improve the knowledge and awareness about HIV and STIS in MSM and TGs. They should discuss the risks related to sexual acts, specifically anal sex, and address misconceptions related to condom use with men. |
Abbreviations: MSM, men who have sex with men; TW, trans woman; ND, Non-determined; TF, trans feminine; MTF, male -to- female; TM, trans masculine; PrEP, pre-exposure prophylaxis; FTM, female-to-male; BLTW, black and Latina transgender women; HP, healthcare professional; STIs, sexually transmitted infections.
4.2.2. Knowledge
4.2.2.1. General HIV Knowledge
Five studies assessed knowledge about HIV (18, 19, 23, 24, 27). Studies by Andrinopoulos et al., Rodriguez-Madera and Toro-Alfonso, and Poteat et al. indicated a high level of HIV knowledge among transgender individuals (18, 24, 27). Conversely, De Santis et al. and Kenagy and Hsieh found gaps in knowledge regarding HIV risk/transmission (19, 23).
4.2.2.2. Pre-Exposure Prophylaxis
Three studies (23%) investigated knowledge of PrEP among transgender individuals (22-24). Hoagland et al.’s study indicated lower pre-exposure prophylaxis (PrEP) awareness among younger, less educated, and mixed-race participants (22). Knowledge of HIV/AIDS was significantly linked to using protection during the most recent sexual encounter (23) and the willingness to use PrEP (24). Another study revealed that 57% of participants were aware of HIV transmission routes yet engaged in high-risk sexual behaviors (27). Sevelius discovered that condoms were only used by transgender people’s partners for anal intercourse (29) (Table 2).
4.2.2.3. Individual Beliefs (Attitudes)
4.2.2.3.1. Perceived Risks
Perceived susceptibility or risk among transgender individuals regarding HIV varied across studies, with three studies (18, 24, 29) reporting perceptions of risk between 53 - 75%. However, five studies (19, 20, 25, 27, 29) indicated a low perceived risk among 59 - 82% of transgender individuals. Fisher's study highlighted that 10 - 25% of participants estimated a 52.1% likelihood of contracting HIV in the following year (20). A significant correlation was observed between risk perception and the use of protection during the last sexual encounter (23), as well as the willingness to take PrEP (24). Four studies (18, 20, 21, 29) found positive relationships between risk perception and undergoing HIV testing, with two studies (18, 29) reporting high HIV testing rates of 75 - 96%, while another study noted that 24% of transgender individuals had never been tested for HIV (27). Scheim and Travers indicated that a sense of responsibility towards partners or recent risky behaviors motivated testing for HIV/STIs (28).
4.2.2.3.2. HIV-related Services
Two studies (18, 25) examined HIV-related services. In Andrinopoulos's research, 80.7% of transgender participants believed they had access to HIV care and treatment services if needed (18). Reisner et al.'s study emphasized the importance of accessible HIV testing and the necessity of making these services readily available for transgender women (25).
4.2.2.3.3. Perceived Severity
According to Andrinopoulos, 65.4% of participants, including trans MSMs and transgender women, intended to test for HIV within the next year (18). Poteat et al.'s research revealed a low uptake of PrEP, with 75% of HIV-negative individuals expressing interest in PrEP if it were accessible (24). Setia et al.'s study found that nearly 79% did not anticipate contracting HIV despite 64% being HIV-positive (30). Hoagland et al.'s research indicated that 27.3% of participants perceived a 50 - 100% chance of contracting HIV in the upcoming year (22). A mixed-method study by Reisner et al. revealed that four out of 11 HIV-positive participants (36.3%) believed their infection was a result of engaging in sex work (25).
4.2.2.3.4. Perceived Benefits
Poteat et al.'s study revealed that 85% of participants expressed willingness to receive an HIV vaccine (24). Sevelius mentioned that utilizing online platforms for dating with potential sexual partners was seen as a preventive strategy (29).
4.2.2.3.5. Perceived Barriers
Two studies addressed maltreatment and sexual abuse (18, 26). Andrinopoulos found no correlation between a history of sexual abuse or maltreatment and undergoing HIV testing (18). However, HIV testing was positively linked to experiences of sexual assault and visiting a doctor in the past year (18). Mistreatment in healthcare settings significantly hindered TW’s access to HIV prevention, testing, and treatment (26). Discrimination in healthcare environments was experienced by 54% of HIV-positive TW, with reports of various forms of unfair treatment by healthcare providers (26). One study found no link between experiencing discrimination from healthcare providers and HIV testing (18). Rodriguez-Madera and Toro-Alfonso reported that 55% of MTFs experienced discrimination (27). Moreover, 42% of TWs faced a high level of stigma following HIV testing (18). Golub and Gamarel's research indicated that anticipated HIV stigma reduced the likelihood of HIV testing by 60% (21), with lower anticipated stigma scores among older, black, and less educated participants (21). Healthcare professionals demonstrated HIV-related stigma towards TWs irrespective of their HIV status (26). Concerns about hormone therapy side effects (47%) and reluctance to take a daily pill (41%) were significant reasons for 65% of transgender individuals not wanting to take PrEP (24). Reisner identified barriers such as inadequate training or guidelines for healthcare providers in integrating HIV services with gender-affirmative care (26). Scheim and Travers noted that HIV testing providers often lacked an understanding of transgender issues (28). Reisner et al. also highlighted a deficiency in long-term health-related resources for transgender individuals (26). Limited clinical capacity for meeting STI testing demands was reported as a barrier to HIV/STI testing among transgender people (28).
In Reisner et al.'s study, 50% of TW reported mistrust towards healthcare professionals as a significant issue (26). Similarly, transgender men expressed reluctance to seek preventative care due to mistrust (28). Additionally, low self-esteem was identified as a barrier to sexual negotiation, a risk factor for HIV (29).
Reisner et al. also noted that the fear of stigmatization and suspicion of being HIV-positive deterred individuals from entering HIV/AIDS care centers (26). Scheim and Travers highlighted the fear of a positive HIV test result and difficulties in accessing sexual healthcare as reasons for avoiding or delaying HIV testing (28). Moreover, gender construction was recognized as an obstacle to HIV prevention efforts (27).
4.2.2.3.6. Perceived Self-efficacy
Kenagy and Hsieh's research found that both MTF and FTM transgender individuals had high self-esteem scores, which correlated with protective measures during their last sexual encounter (23). Poteat et al. observed that high levels of pride among transgender individuals were linked to their willingness to take PrEP (24). Some transgender individuals took pride in themselves, leading to increased self-esteem and more proactive engagement in behaviors to prevent HIV (29). Conversely, 57.8% of participants felt their lives were less valuable than others; 51.1% of TWs had no interest in living, and 64.4% sometimes experienced self-hatred (29).
4.2.2.4. Action: Individual Behavior
Sevelius's research indicated that condom usage among participants was 8.9% for oral sex, 31.1% for vaginal sex, and 40% for anal sex (29), with condom use frequency varying among those with paying partners (29). Studies by Andrinopoulos et al. (18), Kenagy and Hsieh (23), and Poteat et al. (24) reported the prevalence of unprotected sex in the last six months among transgender individuals as 41.5%, 48%, and 50%, respectively, identifying it as the primary reason for considering PrEP (24). Reisner et al.'s study found that 45.5% of participants engaged in unprotected oral sex with ejaculation in the mouth, with the majority inconsistently using condoms (25). Setia et al.'s research highlighted that 50% of transgender individuals did not deem condom use necessary when engaging with seemingly healthy male partners (30). According to another study, female-to-male transgenders (FTMs) reported lower condom use (29%) in their last sexual encounter compared to male-to-female transgenders (MTFs) (59%), with a projected annual 6% decline in protection use during the last sexual contact among transgender people (23). Primary partners were identified as the main source of unprotected sexual contact among transgender individuals, more so than casual partners or clients (27). Unprotected anal sex was reported by 47% (24), 90.9% (25), and 54% of transgender participants (30), with 61.6% reporting at least one instance of unprotected anal sex with a casual male partner in the preceding month (21).
Hoagland et al.'s study linked unprotected anal intercourse to the consumption of higher drug doses (22). Crack and cocaine use in the last month was reported by 15.3% of transgender individuals (18), with 60.5% indicating binge drinking (18). Sexual activity while under the influence of alcohol or drugs was also a notable finding in this research (18). Another study highlighted that 29.9% of transgender individuals reported using some form of illicit drug in the preceding three months, with marijuana (28.4%) and stimulants (13.7%) being the most common (22). In Sao Paulo, 1.1% of transgender individuals were identified as injecting drug users (IDUs) (22). Reisner et al. found that in the last year, engaging in sexual activity while using substances like alcohol, marijuana (63.6%), crack (54.4%), and cocaine (36.4%) was reported, along with the use of crystal methamphetamine, downers, ecstasy, and sildenafil citrate (Viagra) (25). Lifetime drug use among transgender individuals was most frequently reported for marijuana (53.3%), ecstasy (20%), and poppers (17.8%) (29). Rodríguez-Madera and Toro-Alfonso noted high levels of alcohol and drug consumption among 56% of participants (27). Sevelius observed that using drugs and alcohol before sexual encounters often helped alleviate anxiety for many participants but led to impaired condom use (29). A negative correlation was identified between the risky sexual behaviors of MTFs and their age and education level, whereas no correlation was found with monthly income (19). Kenagy and Hsieh reported that 64% of transgender individuals engaged in risky sexual behaviors (23), with FTMs (81%) more likely to partake in risky sexual activities compared to MTFs (55%) (23).
De Santis et al.'s study revealed that 40% of interviewees did not have sexual partners, while 18% reported having over 51 sexual partners within three months (19). Fisher et al.'s research found a positive correlation between age and the number of lifetime sexual partners (20). One study showed the median number of lifetime non-trans male sexual partners for transgender men was 25, with a median of three non-trans male sexual partners in the past year (29). According to Setia et al., the median number of male sexual partners for transgender individuals in the last six months was 50 (30). Hoagland et al. and Poteat et al. reported PrEP uptake rates of 60.9% and 17%, respectively (22, 24). Willingness to take PrEP was significantly linked with HIV knowledge, transgender pride, legal gender affirmation, a history of sex exchange, and HIV risk perception (24). No relationship was identified between PrEP uptake and factors such as age, city, Hispanic/Latina ethnicity, race, language, recent unprotected anal sex, and ongoing hormone therapy (24). 38% of PrEP users believed they were not at risk for HIV (24).
Hoagland et al.'s study observed that participants who did not take PrEP were less likely to report anal sex with partners of unknown HIV status compared to others (22). A majority (63.1%) of these respondents engaged in both receptive and insertive anal sex, while 44.7% reported unprotected receptive anal intercourse (22). Poteat et al.'s research found that 79% of black and Latina transgender women were sex workers (24). According to Sevelius, some viewed sex work as enjoyable and a means of making extra money or as a survival strategy (29). Setia et al. reported that 96% of participants had exchanged sex for money in the last six months (30). Reisner et al. highlighted the grave implications of HIV infection, particularly among transgender sex workers (25). HIV serostatus was assessed in about 38.5% of studies (24, 25, 27, 29, 30), with reported prevalence rates of 14% (27), 36.4% (25), 56% (24), and 68% (30), and 90% were aware of their positive status (24). Sevelius reported a self-reported HIV positivity rate of 2.2% (29). Poteat et al. noted that 25% of TFs were raped, often leading to the use of PEP (24). Rape during sex work was reported by 45.5% of transgender sex workers, and 18.2% had experienced trauma and abuse in childhood or adulthood (25). Sexual assault was reported by 20.8% of transgender individuals in Andrinopoulos's study (18).
4.2.2.5. Cues to Action
One study indicated that 62.1% of transgender individuals participated in at least one HIV educational session last year (18). The presence of a TGW among healthcare team members was cited by both TGWs and healthcare professionals as a motivation to engage in further educational programs (26). Scheim and Travers highlighted that the involvement of transgender individuals in delivering gender-affirming healthcare services has facilitated routine HIV testing, making it more prevalent among this population (28). According to Fisher et al., 25% of healthcare providers offered gender and sexual minorities (GSM) information about their sexual health needs. Interestingly, higher engagement levels were reported by youth who had received gender-affirming hormone therapy (GHT) and had disclosed their gender identity to their parents (20). Reisner et al.'s study identified peer health promoters as crucial support for the transgender woman community in accessing health services, as acknowledged by both healthcare professionals and TWs (83.4%) (26) (Table 2).
5. Discussion
This review analyzed 13 studies, each addressing one or more aspects of knowledge, attitudes (including perceived threats, benefits, barriers, and self-efficacy), and practices of the transgender population regarding HIV/AIDS. Variations in findings are attributed to the diversity in research settings among these studies.
5.1. Knowledge
Regarding knowledge about HIV/AIDS among transgender individuals, although a high level of knowledge was observed in 60% of the related studies, Hessou et al.'s research in Benin reported a 40% low knowledge level (19, 23, 31). The presence of an acceptable knowledge level in this group underscores the effectiveness of educational and prevention methods, which should be continuously enhanced and expanded (31). To improve transgender individuals' knowledge of HIV/AIDS, our study recommends the development of inclusive sex education, collaboration with transgender-led organizations, ensuring accessible healthcare, enhancing peer support networks, engaging with transgender influencers, tackling systemic barriers, crafting more efficient prevention strategies, and encouraging further research on these groups.
5.2. Risk Perception
Nearly 70% of the studies investigated the risk perception of transgender individuals regarding HIV, finding a wide range of perceived susceptibility or risk (52 - 82%) (18-20, 24, 25, 27-29). Three surveys indicated high risk perception (18, 24, 29), while it was low in five studies (19, 20, 25, 27, 28). Positive correlations were established between risk perception and behaviors such as previous HIV testing, use of sexual protection, willingness to take PrEP, and a high level of HIV/AIDS knowledge (18, 20, 21, 29). The HIV testing rate among transgender people was reported at 75 - 95% (18, 29), although Hamilton et al.'s study noted a lower rate in the Caribbean due to critical barriers such as stigma, discrimination, lack of confidentiality, testing site accessibility, poverty, and low HIV risk perception (32). Additionally, participants in one study believed they had a 50% higher chance of contracting HIV in the next year (20). To improve transgender individuals' understanding of HIV/AIDS risks, our study recommends increasing awareness through targeted campaigns, educating on transmission modes and prevention, combating stigma and discrimination, ensuring accessible testing and treatment, and empowering the transgender community with support networks and resources.
5.3. Perceived Severity
One-third of the transgender participants reported perceptions of HIV/AIDS severity. A few studies highlighted the perceived benefits of HIV/AIDS prevention measures (24, 25), showing a strong inclination towards various preventive methods. Our study stresses the need to refine and enhance diverse educational programs on prevention.
5.4. Perceived Barriers
The following factors negatively impacted the willingness of transgender individuals to undergo HIV testing or receive appropriate care: Discrimination by approximately half of healthcare providers (18, 21, 26, 27), mistrust towards healthcare professionals (26), healthcare providers' limited knowledge (28), absence of relevant guidelines (26), challenges in accessing long-term health facilities (28), fear of HIV test positivity (28), treatment side effects (24), sexual abuse (18), and gender construction issues (27). A 2021 review study also underscored treatment side effects as a major concern for trans women and a significant barrier to accessing care (33). To address the perceived barriers faced by transgender individuals concerning HIV/AIDS, it is essential to offer culturally sensitive and accessible healthcare services, reduce stigma and discrimination, and create specific support programs for this vulnerable group.
5.5. Perceived Self-efficacy
The perceived self-efficacy of transgenders ranged from low to high. A high self-esteem score was associated with using sexual protection in the last sex (23), risky sexual activities (23), and willingness to take PrEP (24). Similarly, a study by Mizuno et al. demonstrated that depression and lower self-efficacy to take medication as prescribed were strongly associated with antiretroviral therapy adherence, and transgender people reported lower self-efficacy to integrate treatment plans (34). Also, many patients felt that their life was worthless or they were not interested in living anymore (29). In order to bolster the perceived self-efficacy and self-esteem of transgender individuals regarding HIV/AIDS, it is essential to design empowerment programs, providing skills-building workshops, cultivate supportive networks, and recognize and celebrate their resilience and achievements.
5.6. Action
According to actions, approximately two-thirds of transgenders engaged in sexually risky behaviors (23). In addition, 20% of respondents had 3 - 51 sexual partners (19, 29). A high rate of unprotected sex was also reported (18, 21, 23-25, 29, 30), which should be targeted to reduce condom stigma (35). Around 60% used to drink alcohol (18, 27) or take drugs (18, 22, 25, 27, 29). Moreover, 21 - 45% of transgender individuals were raped (18, 25). Finally, 14-68% were HIV-positive (18, 23, 24). Consistent with these findings, a study by Muzakkir et al. showed a 75% prevalence of risky behavior among transgender women (36). So, improving their knowledge and awareness about the consequences of risky behavior is necessary. To diminish risky behaviors among transgenders which can lead to being infected by HIV/AIDS, it is necessary to deliver comprehensive sexual education, provide strategies for harm reduction and condom usage, and address issues related to substance abuse for this specific group. Additionally, organizing outreach initiatives, and offering incentives to encourage preventive measures among this population are highly recommended.
5.7. Cues to Action
Also, in some studies, cues to action were reviewed. According to the evidence, training peer health advisers can improve HIV prevention and care in high-risk populations (37). Consistently, we found that the presence of a TW on a healthcare team has been identified as a motivator for additional educational efforts as a peer effect (26). The main role of peers in guiding transgender individuals toward health services was also shown (26). However, the role of social media as a cue to action was not studied in any of the selected articles. A study by Tanner et al. revealed that social media is an important tool for TW to help them with viral suppression, reduced transmission efficiency, and PrEP use (38). Furthermore, health science educators have an ethical duty to include gender-affirming health in health science curricula, which mentioned by de Vries et al. (39). In this regard, it is recommended to train peer health educators and advisers who are more trustable for Transgender population. Also, it is suggested to use social media and networks for increasing transgenders’ awareness regarding HIV/AIDS and sending them regular reminders for check-ups through social networks.
5.8. Strengths, Limitations, and Recommendations
This study's strengths include providing a comprehensive overview of the factors linked to the HBM components concerning HIV/AIDS in the transgender population. The use of the HBM offered a theoretical framework to comprehend the factors influencing HIV/AIDS-related behaviors and beliefs among transgender individuals. Moreover, this research specifically targets a marginalized and vulnerable group, highlighting unique challenges and experiences related to HIV/AIDS.
However, the systematic review faced limitations due to the availability and quality of the studies reviewed, particularly regarding some HBM components like perceived benefits, perceived self-efficacy, and cues to action. The inclusion criteria, limited to English-language publications, could introduce language bias. Additionally, the study did not encompass unpublished studies or gray literature.
5.9. Recommendations by Authors
Future research should evaluate the critical variables identified in this study. There is a lack of evidence on the perspectives of individuals, transgender individuals' families, policymakers, and healthcare providers regarding the transgender population. Besides the HBM, incorporating other theoretical frameworks could offer deeper insights into factors affecting HIV/AIDS-related behaviors and beliefs among transgender people. Longitudinal studies are necessary to monitor changes over time in knowledge, attitudes, practices, and risk perceptions and to assess the impact of interventions aimed at improving HIV/AIDS outcomes in transgender populations.
6. Conclusions
The transgender population remains underserved. Despite high levels of knowledge and varied perceptions of risk concerning HIV/AIDS, instances of risky and unprotected sexual behaviors and perceived barriers to accessing health services are prevalent. This study's findings should inform health policymakers to develop a long-term, effective surveillance system for this marginalized group. Additionally, creating evidence-based, culturally sensitive, and inclusive intervention programs is crucial for addressing the needs of these communities.