1. Background
Laparoscopic cholecystectomy (LC) is widely regarded as the most effective and safe treatment for symptomatic cholelithiasis, making it the preferred surgical option. Among individuals with symptomatic gallstones (GS), approximately 10% develop acute cholecystitis (AC), accounting for about 750,000 cases annually. Laparoscopic cholecystectomy provides notable advantages over conventional cholecystectomy, including reduced postoperative pain, faster recovery, quicker restoration of bowel function, and shorter hospital stays. Despite its widespread use, certain cases of LC may require conversion to open cholecystectomy (OC) due to various intraoperative challenges. Conversion ensures safe completion of the procedure but can prolong the expected surgical duration. Existing literature reports a conversion rate ranging from approximately 2% to 10% (1-6). The primary goal of LC is to achieve symptom relief and survival without impairment. However, adverse outcomes following LC can significantly impact these objectives. These complications range from minor issues, such as surgical site infections, to more severe outcomes like bile duct injury (BDI) and even mortality (7). Persistent postoperative pain remains a considerable issue, often leading to extended hospital stays or additional medical visits. Due to significant variability in pain management protocols, a standardized approach is needed to ensure effective interventions for pain reduction (8).
During the early stages of laparoscopic surgery, AC was considered a relative contraindication for LC. However, subsequent research has challenged this notion, advocating for early surgical intervention in AC cases. Laparoscopic cholecystectomy performed within 72 hours of symptom onset is now endorsed for its benefits, including shorter hospital stays, reduced healthcare costs, and lower readmission rates. Despite these advantages, many general surgeons still prefer a non-operative approach for initial AC management, followed by delayed LC. Arguments against early LC often cite increased technical difficulty, higher conversion rates (6 - 35% in some studies), and greater risks of biliary complications, such as bile leaks and common bile duct (CBD) injuries, when operating on inflamed gallbladders with swollen tissues and distorted anatomy.
The timing of LC in cases of AC remains a contentious issue. Studies conducted in Europe, Japan, and the United States reveal significant disparities in practices, with early LC rates ranging from 11% to 89% among surgeons (9-11). Numerous studies have compared the outcomes and complications of elective versus emergent cholecystectomy (12-14), reinforcing a general belief that emergent LC may result in higher rates of intraoperative and postoperative complications (15, 16).
2. Objectives
Consequently, this study aims to compare the intraoperative and postoperative outcomes and complications of LC in patients undergoing emergent versus elective procedures.
3. Methods
3.1. Study Design
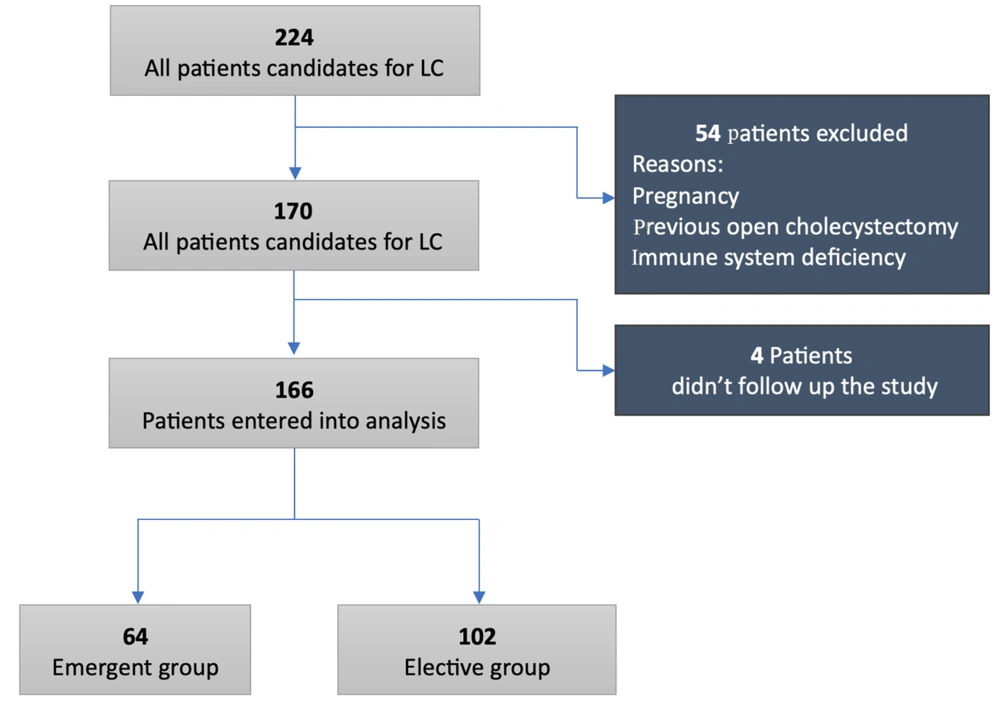
This case-control study was conducted in the Surgery Department of Baqiyatallah Hospital, Tehran, Iran, from January 2021 to December 2022. The final data analysis was completed in June 2023. Patients who presented to the department with clinical symptoms and were confirmed to have GS with cholelithiasis and scheduled for surgery were included in the study. Patients who were pregnant, had a history of previous OC, or had immune system deficiencies were excluded from the study.
The study population was divided into two groups: (1) The emergent group, and (2) the elective group. Patients admitted in acute and emergency conditions who underwent surgery within 24 hours of symptom onset were categorized into the emergent group (n = 64). Conversely, patients scheduled for LC as part of a planned procedure were categorized into the elective group (n = 102). The study design is illustrated in Figure 1.
The surgeries for both groups were performed by surgeons following a standardized procedure. Laparoscopic cholecystectomy surgery commenced with the patient positioned in the Trendelenburg position, typically utilizing three ports. If necessary, a fourth port was added. This setup allowed for the insertion of long surgical instruments and a surgical video camera. The surgeon observed the gallbladder (GB) and surrounding organs on a monitor connected to the camera, controlling the telescopic instruments externally while monitoring the procedure on the display.
The surgery began with the elevation of the GB fundus. Dissection using diathermy proceeded in Calot's triangle to expose the cystic artery and cystic duct. An intraoperative cholangiogram was performed at the surgeon's discretion. The cystic duct and artery were clipped and divided, and the GB was removed from the liver bed in a retrograde manner. The GB was extracted through either the umbilical or epigastric port using an endoscopic retrieval bag.
The umbilical fascia and skin were closed with sutures, and a local anesthetic was administered at the surgical wound sites. Postoperatively, participants in both groups were followed up until suture removal at the port site (one week after surgery) and monitored for complications up to three months post-surgery.
3.2. Data Collection
All patient-related details, including medical history, general and detailed physical examinations, comorbidities, any history of prior abdominal surgeries, blood investigations, abdominal sonography, and endosonographic findings, were meticulously documented. Intraoperative complications, surgical findings, and postoperative recovery parameters were also recorded.
Postoperatively, data on the duration of hospital stay, post-surgery pain levels, and any conversions to OC were gathered. Additionally, all patients were followed up for three months after surgery to monitor outcomes and ensure comprehensive assessment.
3.3. Ethical Consideration
This study received approval from the Research Ethics Committee of Baqiyatallah University of Medical Sciences, under the ethical code IR.BMSU.REC.1397.034, and was conducted in accordance with the principles outlined in the Declaration of Helsinki (1975). All participants provided written informed consent to participate in the study.
3.4. Statistics
The default alpha error was set at 0.05, and the beta error was set at 0.2. To calculate the sample size, post-surgery hospitalization days were considered the main variable. According to a similar study conducted by Marwah et al., the post-surgery hospitalization duration was 2.76 ± 0.663 days in the acute biliary pancreatitis group and 2.34 ± 0.861 days in the acute cholecystitis group (P = 0.037) (17). Using a 1: 3 ratio for the emergent to elective groups, the sample size was calculated based on the post-surgery hospitalization days variable using G*Power software. The required sample size was determined to be 134 patients, with 34 patients allocated to the emergent group and 100 to the elective group. To account for the possibility of discontinuation by patients in the emergent group, the sample size for this group was increased from 34 to 40 participants.
Data were analyzed using SPSS software (v. 29). The chi-square test was used to compare qualitative variables, while independent sample t-tests were used to compare mean values between the two groups for normally distributed quantitative parameters. A P-value of < 0.05 was considered statistically significant. Pre- and post-operative pain levels were measured using the Visual Analog Scale (VAS).
4. Results
A total of 170 candidates for LC surgery were initially selected for inclusion in the study. Four patients were excluded as they did not wish to continue participating after surgery, leaving 166 patients who completed the study. The demographic and clinical characteristics of the patients (Table 1) revealed significant differences in several areas. A significant difference was observed in the sex distribution of participants between the groups (P = 0.02). Patients were monitored for conditions such as diabetes, hypertension, and renal, cardiovascular, and respiratory diseases. The prevalence of cardiovascular disease was significantly higher in the emergent group (10.9%) compared to the elective group (1%) (P = 0.006). In the emergent group, 57.8% of patients had an ASA score of 1, 28.1% had an ASA score of 2, and 14.1% had an ASA score of 3. Conversely, in the elective group, 55.9% of patients had an ASA score of 1, 41.2% had an ASA score of 2, and only 2.9% had an ASA score of 3. The differences between the groups were significant (P = 0.01). Patients in the emergent group reported significantly higher pain levels before surgery compared to the elective group (P < 0.001). All emergent group patients were symptomatic, while 58.8% of elective group participants were asymptomatic, a significant difference (P < 0.001). Significant differences were noted in sonographic findings (P < 0.001). In the emergent group, 53.1% of patients had GS, 43.8% had GS with increased GB wall thickness, and 3.1% had extrahepatic bile duct dilation. In contrast, in the elective group, 91.2% of patients had GS, 2% had GS with increased GB wall thickness, and six patients (5.8%) had GB polyps. Significant differences were observed between the groups in the mean values of white blood cell (WBC) count (P < 0.001), total bilirubin (P < 0.001), and alkaline phosphatase (ALP) levels (P < 0.001).
| Variables | Groups | P-Value | |
|---|---|---|---|
| Emergent | Elective | ||
| Age | 52.75 ± 14.15 | 48.4 ± 13.99 | 0.054 |
| Gender (M: F) | 36 (56.2): 28 (43.8) | 39 (38.2): 63 (61.8) | 0.023 |
| BMI | 64 (27.73 ± 4.39) | 1.2 (27.67 ± 4.56) | 0.189 |
| ASH | 0.717 | ||
| N/A | 54 (84.4) | 80 (78.4 | |
| UA | 0 | 1 (1) | |
| LA | 10 (15.6) | 21 (20.6) | |
| Comorbidity | |||
| Diabetes | 10 (15) | 13 (12) | 0.601 |
| Hypertension | 9 (14.1) | 25 (24) | 0.105 |
| Renal | 0 | 1 (1) | 0.999 |
| Cardiovascular | 7 (10.9) | 1 (1) | 0.006 |
| Respiratory | 1 (1.6) | 0 | 0.386 |
| ASA score | 0.014 | ||
| 1 | 37 (57.8) | 57 (55.9) | |
| 2 | 18 (28.1) | 42 (41.2) | |
| 3 | 9 (14.1) | 3 (2.9) | |
| Pre-surgery pain | 4.53 ± 1.88 | 1.90 ± 1.89 | < 0.001 |
| Physical examination | < 0.001 | ||
| Asymptomatic | 0 | 60 (58.8) | |
| Tenderness | 23 (35.9) | 39 (38.2) | |
| Tenderness and rebound | 0 | 1 (1.0) | |
| Tenderness and Murphy | 41 (64.1) | 2 (2.0) | |
| Sonography findings | < 0.001 | ||
| GS | 34 (53.1) | 93 (91.2) | |
| Thickness increase & GS | 28 (43.8) | 2 (2) | |
| EBDD | 0 | 1 (1) | |
| GB polyp | 0 | 6 (5.9) | |
| Increase GBWT g & EBDD | 2 (3.1) | 0 | |
| Blood investigation | |||
| WBC | 11.49 ± 4.07 | 6.63 ± 2.11 | < 0.001 |
| BILLT | 1.72 ± 1.31 | 1.08 ± 0.81 | < 0.001 |
| ALP | 320.5 ± 209.68 | 215.04 ± 110.94 | < 0.001 |
| Endosonography findings | 0.999 | ||
| Have duct stone | 8 (40) | 3 (37.5) | |
| No duct stone | 12 (60) | 5 (62.5) | |
According to the results, 57.8% of surgeries were completed using a three-trocar technique (77.5% of elective group patients), while 42.2% required the use of a fourth trocar (22.5% of elective group patients). This difference was statistically significant (P = 0.007) (Table 2). In one patient from the emergent group, the surgery was converted to OC due to unclear anatomy and suspicion of gallbladder cancer. However, the difference in conversion rates between the groups was not statistically significant (P = 0.38). Additionally, 35 patients (55.5%) in the emergent group required the insertion of a drain, compared to 25 patients (24.5%) in the elective group, a difference that was statistically significant (P = 0.003).
| Variables | Groups | P-Value | |
|---|---|---|---|
| Emergent | Elective | ||
| First trocar entry method | 0.43 | ||
| Veress needle | 3 (4.7) | 10 (9.8) | |
| Open method | 23 (35.9) | 31 (30.4) | |
| Use of trocar | 38 (59.4) | 61 (59.8) | |
| Converting surgery from 3 to 4 trocar | 0.007 | ||
| Three trocar | 37 (57.8) | 79 (77.5) | |
| Four trocar | 27 (42.2) | 23 (22.5) | |
| Conversion to OC | 1 (1.6) | 0 | 0.386 |
| Intraoperative Complication | 0.145 | ||
| N/A | 43 (68.3) | 80 (78.4) | |
| Duct injury | 0 | 0 | |
| Bleeding | 0 | 0 | |
| Other organ injury | 0 | 0 | |
| GB perforation | 20 (31.7) | 22 (21.6) | |
| Drain insertion | 0.003 | ||
| Inserted | 35 (55.5) | 25 (24.5) | |
| Not inserted | 28 (44.5) | 77 (75.5) | |
| Fascia repair of the UT entry site | 0.570 | ||
| Repaired | 56 (87.5) | 86 (84.3) | |
| Not repaired | 8 (12.5) | 16 (15.7) | |
| DOS, n (mean ± SD) | 64 (70.39 ± 33.44) | 102 (72.89 ± 35.91) | 0.65 |
The post-surgical complications investigation (Table 3) showed no significant differences in local (P = 0.77) or systemic (P = 0.37) complications between the emergent and elective groups. Regarding pain levels, one day after surgery, patients in the emergent group reported a mean pain score of 1.76 ± 1.03, compared to 1.02 ± 0.80 in the elective group, a statistically significant difference (P < 0.001). Similarly, one-week post-surgery, the mean pain score was 0.49 ± 0.66 in the emergent group and 0.14 ± 0.43 in the elective group, again showing a significant difference (P < 0.001). By three months post-surgery, all patients reported no pain.
| Variables | Groups | P-Value | |
|---|---|---|---|
| Emergent | Elective | ||
| Local complications post-surgery | 0.773 | ||
| N/A | 60 (96.8) | 99 (97.1) | |
| Bleeding | 0 | 0 | |
| Local infection | 2 (3.2) | 2 (2) | |
| Trocar site hernia | 0 | 1 (1) | |
| Systemic complications post-surgery | 0.378 | ||
| N/A | 61 (98.4) | 102 (100) | |
| Pulmonary embolism | 0 | 0 | |
| Cardiovascular complications | 0 | 0 | |
| Respiratory complications | 1 (1.6) | 0 | |
| Post-surgery pain | < 0.001 | ||
| First-day post-surgery | 1.76 ± 1.03 | 1.02 ± 0.80 | |
| First-week post-surgery | 0.49 ± 0.66 | 0.14 ± 0.43 | |
| Post-surgery hospitalization | 63 (1.55 ± 0.79) | 102 (1.19 ± 0.50) | 0.002 |
| Duration of return to daily activity, n (mean ± SD) days | 62 (4.82 ± 2.52) | 101 (3.77 ± 1.21) | 0.003 |
In analyzing the correlation between pain levels one day post-surgery and drain insertion, patients without a drain (n = 104, 1.14 ± 0.86) experienced significantly less pain (P = 0.002). A significant difference in post-operative hospital stay was also observed between the two groups (P = 0.002). The mean recovery time to resume routine activities was 4.82 ± 2.52 days in the emergent group, compared to 3.77 ± 1.21 days in the elective group, a statistically significant difference (P = 0.003). Additionally, patients without a drain had significantly shorter hospital stays than those with a drain (P < 0.001).
5. Discussion
Gallstone disease is one of the most common gastrointestinal issues. While GS is typically asymptomatic, 2 - 4% of individuals with GS progress to painful cholecystitis, potentially leading to AC. Historically, OC was the standard treatment for cholecystectomy. However, LC has become the gold standard and the preferred surgical method for most surgeons. Despite its advantages, LC in emergent cases can present complications, such as acute inflammation, edema, and an increased risk of mortality. This study was designed to compare the risks and complications of emergent LC cases with elective cases.
The relationship between male gender and difficult cholecystectomy remains a topic of debate. Some studies suggest that male gender is a risk factor for difficult cholecystectomy, possibly because cholelithiasis is predominantly considered a female disease, leading to delayed diagnosis in males. This delay may result in significant adhesions from repeated inflammatory episodes before diagnosis. Nidoni et al. (as cited in Gupta et al.) (5) found that the conversion rate to OC was significantly higher in males compared to females (P = 0.03, 95% confidence interval).
The demographic data from this study indicated that cardiovascular disease was the only comorbidity significantly different between the emergent and elective groups (P = 0.006). This finding aligns with Abe et al. (18), who reported a significant prevalence of cardiovascular disease in patients with concomitant biliary infections. However, Abe et al. did not find a meaningful difference between urgent and semi-urgent groups (P = 0.04) (18). Additionally, a significant number of patients in both groups presented with abnormal alkaline phosphatase (ALP) levels (P = 0.01), an important indicator of bile duct issues. Singal et al. (19) evaluated liver function tests (LFTs) in patients undergoing LC or OC and found elevated serum levels in both groups. However, they did not observe any significant difference in ALP or total bilirubin levels between the groups prior to surgery (P = 0.09).
Our results revealed that patients in emergency situations experienced more pain before surgery than those in the elective group, which can be attributed to the acute condition of cholecystitis or the need for drain insertion. One-day post-operation assessments showed that although both groups reported significantly reduced pain compared to pre-surgery levels, there was still a significant difference between the groups. Furthermore, a week after surgery, monitoring again demonstrated lower pain levels in both groups; however, the emergent group continued to experience significantly higher pain compared to the elective group (P < 0.001). The monitoring extended to three months post-surgery, at which point none of the patients reported any pain. A plausible explanation for the observed pain could be the higher rate of drain insertion in the emergent group compared to the elective group, as indicated in Table 2. This aligns with the finding that patients in the emergent group reported more post-operative pain.
Hospital stays were also longer, and the time to return to routine life was extended in the emergent group. This could be due to the patients' acute conditions or higher disease severity, requiring additional recovery time post-surgery (20). Nonetheless, prior studies have consistently reported shorter hospital stays for LC patients compared to OC patients (21). Ferrarese et al. concluded that drain insertion might contribute to extended post-operative hospital stays in the emergent group (22). Other studies have corroborated our findings, showing that patients in emergency conditions tend to have longer hospital stays following LC surgery (10, 13, 23). In a cohort study (12) comparing emergency and elective LC, more drain insertions were reported in emergency LC patients than in elective LC patients (P < 0.001).
Historically, it has been presumed that cholecystectomy patients in emergency conditions would face more complications both during and after laparoscopic surgery, leading many surgeons to prefer OC over LC. However, our findings indicate no significant differences in most variables, suggesting that emergent LC can be as safe as elective LC in terms of both local and systemic complications. Various studies have similarly reported no major complications or significant differences between emergent and elective LCs (22, 24). One common complication during LC is the need to convert to OC. In our study, only one patient from the emergent group required conversion to OC (P = 0.38).
In a cohort study, Saeb-Parsy et al. compared the efficacy of elective and emergency LC in 423 patients and reported one conversion from LC to OC, which occurred in the elective group (P = 0.64) (24). Ferrarese et al. (22) investigated outcomes between elective and emergency LC in elderly patients and found a higher conversion rate to OC in the elective group, although the difference was not statistically significant (P = 0.38). Additionally, the duration of surgery was comparable between the emergent and elective groups, a finding consistent with Grass et al., who reported similar results in a related study (25).
5.1. Conclusions
Comprehensively, based on previous assumptions and reports, LC—particularly emergency LC—was perceived as less effective and associated with higher intra- and post-operative complications, leading to a lower preference among surgeons. However, the findings of this study contradict that initial hypothesis, demonstrating that emergency LC is both acceptable and justifiable in terms of its success rate and safety profile. It did not result in significant complications for patients. Therefore, LC can be considered a gold standard and low-risk option for patients in emergency situations.