1. Background
The importance of proper nutrition in preventing and managing diseases is widely recognized, leading to a growing emphasis on clinical nutrition science across various levels of care, including primary health care, outpatient care, and acute hospital care (1). Beyond addressing diseases linked to micronutrient and macronutrient deficiencies or excesses, appropriate nutrition plays a vital role in preventing a wide range of conditions by enhancing the immune system (2, 3). Furthermore, incorporating nutritional interventions into clinical therapies can slow disease progression, limit its spread and adverse effects, and contribute to improved health outcomes, increased patient satisfaction, and reduced healthcare costs (4, 5).
Medical universities worldwide have established programs to train professionals in nutrition sciences across diverse disciplines and levels. These graduates provide essential healthcare services, conduct research, and carry out educational and therapeutic responsibilities (6). Nutrition science, as an applied field, demands that nutrition experts possess not only accurate knowledge and a positive attitude but also the necessary clinical skills. As integral members of the healthcare team, nutritionists must undergo well-structured internship courses designed to equip them with practical and purpose-driven training (7, 8).
A review of scientific evidence published in academic journals indicates that universities of medical sciences in Iran have largely overlooked the evaluation and enhancement of training courses and internships in the field of nutrition sciences. They have also failed to adequately assess the performance and satisfaction levels of students, who are the primary beneficiaries of the educational system. The educational process fundamentally involves assessing educational needs, establishing objectives, devising plans, determining content, selecting appropriate learning and teaching methods, and implementing effective evaluation tools and strategies. In contrast, other fields of medical education in Iran, such as general medicine, dentistry, healthcare administration, public health, nursing, midwifery, and laboratory sciences, have systematically evaluated their internship programs. These evaluations have led to the identification and rectification of challenges and deficiencies through targeted interventions, with continuous measurement and improvement of outcomes (9-11).
Several investigations conducted within the nutrition training department at Semnan University of Medical Sciences (SEMUMS) have focused on the experiences of both students and faculty members. These studies have highlighted numerous areas for improvement in the execution of internship courses. Enhancing the effectiveness of internships requires addressing critical factors, such as conducting accurate and evidence-based needs assessments, setting clear and targeted goals that align with the needs of stakeholders, and transparently communicating expectations to students. Furthermore, integrating portfolios to enhance the learning process, strengthening coordination with healthcare sectors to provide high-quality training, establishing a scientific and equitable basis for student evaluations, and utilizing objective tools for assessment are essential steps. Emphasizing the development of students' knowledge and skills upon completing internship courses would further contribute to their overall educational and professional success.
It is crucial to design and implement targeted improvement interventions after identifying and analyzing the root causes of deficiencies. The aim is to address these deficiencies effectively and ensure that the interventions are evaluated accurately and in a timely manner (12). Employing scientific methodologies, such as educational scholarship, can facilitate the identification of shortcomings within the educational process across various domains. Subsequently, designing and implementing improvement measures based on these findings, followed by a thorough evaluation, can yield significant benefits (13-16).
2. Objectives
This study aimed to enhance the hospital internship course for nutrition students by employing a comprehensive checklist for nutritional assessment and patient treatment at SEMUMS.
3. Methods
This study, conducted from 2019 to 2024, employed a mixed-methods approach, including qualitative analysis of expert opinions, tool design and psychometrics, pre- and post-intervention cross-sectional evaluations, and promotional interventions. The "comprehensive checklist for evaluating and providing nutritional treatments to patients" was developed and standardized based on expert advice as a foundation for improvement interventions in internship provision.
A meeting with ten clinical nutrition experts was convened to establish the educational expectations for nutrition students participating in hospital internship courses, covering knowledge, attitudes, and skills. These expectations were translated into essential steps for students, forming the basis for developing the checklist, which was then used to evaluate students' performance during the internship.
Additionally, a supplementary questionnaire was designed to assess student satisfaction with the internship process and its various aspects. This questionnaire was developed through a thorough review of relevant literature and consultation with subject matter experts. Rigorous psychometric evaluation was performed on the tool, incorporating feedback from ten experts in medical education.
The study tools underwent a rigorous psychometric evaluation and standardization process, which included assessing their content and face validity based on feedback from 10 subject matter experts. Experts evaluated the primary questionnaire questions using four indicators: Necessity, relevance, transparency, and simplicity. Content validity was determined by calculating the content validity ratio (CVR) and the content validity index (CVI) (17). Specifically, the CVR was calculated based on the necessity criterion, and once the question was confirmed, the CVI was computed using scores from the other three criteria: Relevance, transparency, and simplicity. The CVI was calculated using the following formula, where nE represents the number of experts who selected the two positive spectrum options and N represents the total number of experts (18):
The acceptance score of 0.62 was used as the threshold for approving or rejecting the questionnaire questions, given the involvement of 10 experts in this phase. Face validity was assessed by obtaining qualitative feedback from experts regarding the phrasing and clarity of the questions, as well as alignment with the relevant literature (18).
The "comprehensive checklist for evaluating and providing nutritional treatment to patients" and the "questionnaire for measuring students' satisfaction with the internship process" achieved high validity scores of 0.98 and 0.89, respectively. The CVR and CVI for these tools were calculated as 0.92 and 0.86, respectively.
The comprehensive checklist for assessing and administering nutritional therapies consists of two primary domains: "Patient assessment" and "patient treatment." The "patient assessment" domain includes sections such as evaluating demographic and background characteristics of patients, assessing patients’ lifestyles, reviewing diagnostic documents, and understanding the history of diseases and prior care, among others. It comprises 13 specific sections or inquiries. The "patient treatment" domain encompasses areas like calculating macronutrients and micronutrients, converting them into food units, creating dietary plans and lists of food substitutes, and offering tailored dietary recommendations, covering 8 sections or inquiries.
The tool used to assess student satisfaction includes three primary domains: "Educational planning," "learning-teaching methods," and "educational evaluation." The "educational planning" domain includes areas such as conducting educational needs assessments, setting objectives, providing appropriate educational content, and ensuring suitable timing for the internship process. It comprises 7 questions or satisfaction components. The "learning-teaching methods" domain includes elements such as aligning instructional approaches, the quality of the educational process, teacher expertise, involving participants in the internship process, and rationally enhancing students' competencies. This domain consists of 12 questions or components. Lastly, the "educational evaluation" domain encompasses aspects like objectivity and fairness in evaluations, developing critical thinking skills to assess system performance, students assisting healthcare workers, and using evaluation results for program enhancement, with 11 questions or satisfaction components.
The reliability (internal consistency) of the study tools was assessed using the test-retest method and validated with a Cronbach’s alpha score of 0.895.
The study employed a census method, involving the participation of 28 students (all students from two different classes). The performance of 14 students who underwent the traditional internship evaluation method was analyzed based on their written reports submitted at the end of the academic semester. Additionally, their satisfaction with the internship process was assessed using the designed tools, and the survey results served as the basis for analysis.
Subsequently, a novel approach for conducting internships in the healthcare sector was implemented. This included training and orientation programs for academic personnel, students, and hospital nutrition specialists. In the following academic year, the internship program was conducted using this new approach. The performance and satisfaction levels of an additional 14 students were then evaluated.
The inclusion criteria for the study were being an 8th-semester nutrition student, while the exclusion criteria included having previously failed the internship. Based on these criteria, all eligible students were included in the study, and none were excluded.
The performance questionnaire was completed by the educational department for each student, while the Satisfaction Questionnaire was distributed to students in paper format. The impact of the implemented interventions was evaluated by comparing the results obtained before and after their execution. Quantitative variables were expressed as frequencies with corresponding percentages, and qualitative variables were reported as means and standard deviations. A t-test was used to compare students' performance and satisfaction levels between the pre- and post-intervention stages.
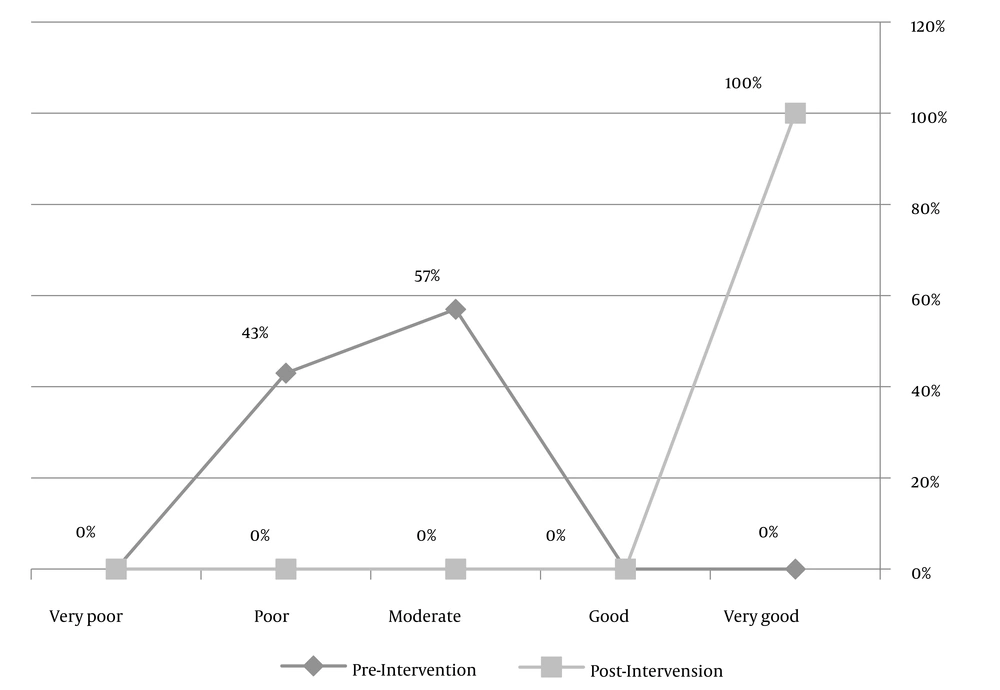
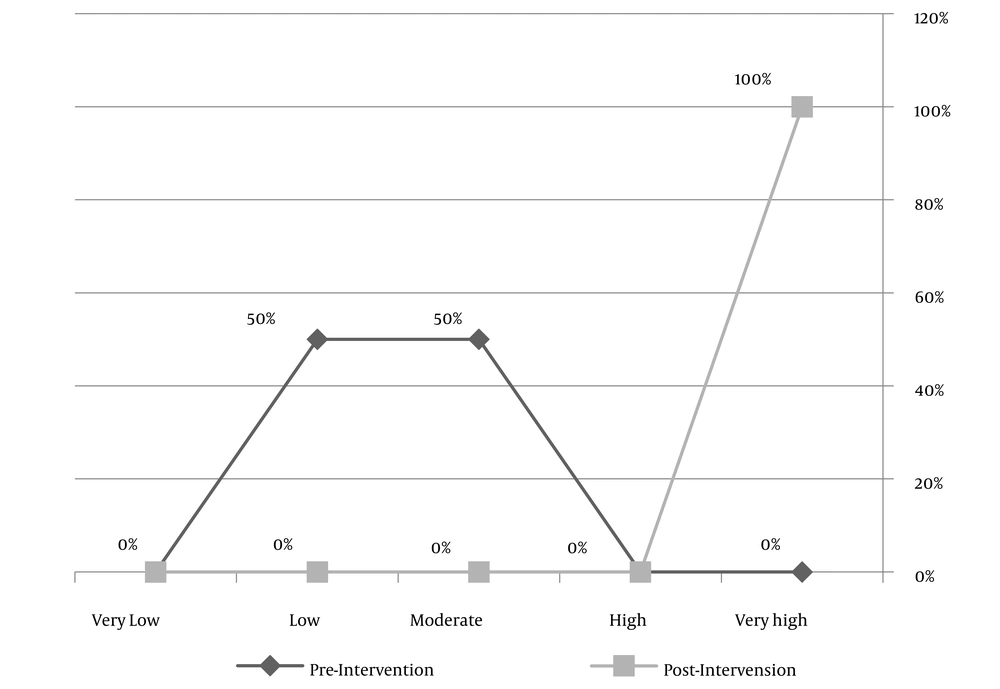
Statistical cut-off points were established to assess performance and satisfaction levels. Scores were categorized into the following ranges: Zero to zero point two (very poor), 0.201 - 0.4 (poor), 0.401 - 0.6 (moderate), 0.601 - 0.8 (good), and 0.801 - 1 (very good).
The study ensured the participation of all relevant stakeholders, including experts and process owners, with the option to decline involvement. Informed consent was obtained from all participants before their inclusion in the study. Participants were assured that their responses would remain completely anonymous and that the data collected would be used exclusively for research purposes. Measures were taken to uphold the privacy and confidentiality of all participants, adhering to ethical standards established by the SEMUMS ethics committee. The research team secured an ethics approval code prior to initiating the study.
4. Results
The majority of students participating in the study were female (64%), with an average age of 22.7 years. Only 7% of participants were natives of the provincial capital, and all resided in student dormitories. Evaluations conducted by relevant professors on students' performance during their internships revealed significant deficiencies before implementing the new internship approach. Specifically, compliance rates with established standards were as follows: Assessing behavioral risks related to nutrition, evaluating pregnancy records, examining current physical conditions, and identifying potential digestive problems—all at a low rate of 4%. However, students demonstrated relatively satisfactory performance in determining necessary macronutrients and micronutrients and converting them into food units, with compliance rates of 82%, 79%, and 86%, respectively.
After the introduction of the new strategy, student performance improved markedly across all major areas. Analysis of the primary domains of student performance within the internship curriculum showed significant enhancement. Performance in the "patient assessment" domain increased from 29% to 95%, while the "patient treatment" domain improved from 59% to 100%. Overall, student performance rose substantially from 40% to 97% following the implementation of the new approach. While improvements in patient evaluation were particularly notable, all changes in the primary functional areas and overall performance status were statistically significant (P < 0.001) (Table 1).
| Dimensions and Items | Pre-test | Post-test | P-Value |
|---|---|---|---|
| Patient assessment | |||
| Demographic data collection | 0.39 ± 0.213 | 0.96 ± 0.134 | < 0.001 |
| Nutritional behavioral risks | 0.04 ± 0.134 | 0.93 ± 0.182 | < 0.001 |
| Female pregnancy records | 0.04 ± 0.134 | 0.89 ± 0.213 | < 0.001 |
| Assessing physical activity | 0.04 ± 0.134 | 0.93 ± 0.182 | < 0.001 |
| Assessing anthropometry | 0.39 ± 0.213 | 1.00 ± 0.000 | < 0.001 |
| Initial complaint investigation | 0.68 ± 0.317 | 0.96 ± 0.134 | 0.021 |
| Medical history | 0.46 ± 0.237 | 0.93 ± 0.182 | 0.001 |
| Checking digestion | 0.04 ± 0.134 | 1.00 ± 0.000 | < 0.001 |
| Drug history | 0.46 ± 0.134 | 0.93 ± 0.182 | 0.001 |
| Dietary supplement evaluation | 0.29 ± 0.257 | 1.00 ± 0.000 | < 0.001 |
| Lab data analysis | 0.43 ± 0.182 | 0.96 ± 0.134 | < 0.001 |
| Doctor's final diagnosis | 0.29 ± 0.257 | 0.93 ± 0.182 | < 0.001 |
| Diet evaluation | 0.29 ± 0.257 | 0.96 ± 0.134 | < 0.001 |
| Dimension score | 0.29 ± 0.071 | 0.953 ± 0.050 | < 0.001 |
| Patient treatment | |||
| Basic computations | 0.75 ± 0.259 | 1.00 ± 0.000 | 0.002 |
| Calculating the amount of macronutrients | 0.82 ± 0.249 | 1.00 ± 0.000 | 0.011 |
| Calculating the amount of micronutrients | 0.79 ± 0.257 | 1.00 ± 0.000 | < 0.001 |
| Food unit conversion of macronutrient and micronutrient quantities | 0.86 ± 0.234 | 1.00 ± 0.000 | < 0.001 |
| Creating a diet based on daily servings | 0.11 ± 0.213 | 1.00 ± 0.000 | < 0.001 |
| Creating a list of food substitutes | 0.61 ± 0.289 | 1.00 ± 0.000 | 0.002 |
| Determining and offering dietary recommendations | 0.61 ± 0.213 | 1.00 ± 0.000 | 0.010 |
| Identifying the nutritional supplements | 0.25 ± 0.259 | 1.00 ± 0.000 | 0.010 |
| Dimension score | 0.598 ± 0.083 | 1.00 ± 0.000 | < 0.001 |
| Total score | 0.409 ± 0.043 | 0.971 ± 0.031 | < 0.001 |
Student Performance in the Old and New Approaches
An analysis of overall student performance based on the established statistical cut-off points before and after implementing the new internship approach revealed the following: Prior to the change, 42.9% and 57.1% of students demonstrated poor and moderate performance levels, respectively, with no students achieving very poor, good, or very good performance levels. In contrast, after the new approach was implemented, all students exhibited an outstanding level of performance (Figure 1).
An analysis of student satisfaction levels with the internship course delivery method before and after implementing the revised approach highlights notable differences. Under the conventional approach, several deficiencies were identified in educational planning. These included the absence of a needs assessment to design the internship framework, the lack of educational goals derived from the needs assessment, and the absence of clearly defined expectations for students based on identified educational goals.
The inadequacies in the learning and teaching methodologies were related to issues such as insufficiently targeted education during internships, unclear scope and depth of the educational content, and a lack of proportional enhancement of students' knowledge, attitude, and skills. Deficiencies in educational evaluation included the use of inadequate tools, misalignment between educational assessment and planning/methods, and a lack of impartial and unbiased assessments.
Following the implementation of promotional interventions, no inadequacies were observed in any aspect of the internship program. The analysis of student satisfaction levels after implementing the new approach revealed significant improvements across multiple dimensions. Satisfaction with educational planning increased from 42% to 85%, satisfaction with the learning-teaching methodology rose from 38% to 88%, and satisfaction with educational evaluation improved from 38% to 92%. Overall satisfaction increased substantially from 39% to 89%.
While the most pronounced positive changes were observed in the realm of educational evaluation, statistically significant improvements were evident across all dimensions and overall satisfaction (Table 2).
| Dimensions and Items | Pre-test | Post-test | P-Value |
|---|---|---|---|
| Educational planning | |||
| Designing an internship framework based on student and stakeholder needs assessments | 0.41 ± 0.158 | 0.93 ± 0.117 | < 0.001 |
| Developing educational objectives based on a needs assessment | 0.39 ± 0.213 | 0.84 ± 0.186 | < 0.001 |
| Developing student expectations based on instructional objectives | 0.34 ± 0.186 | 0.75 ± 0.219 | 0.012 |
| Compilation of appropriate educational content based on the objectives | 0.45 ± 0.223 | 0.95 ± 0.106 | < 0.001 |
| Making necessary arrangements with healthcare facilities | 0.46 ± 0.257 | 0.77 ± 0.183 | 0.023 |
| Appropriate timing of the internship process and clinical rotation in health centers | 0.46 ± 0.237 | 0.84 ± 0.158 | <0.001 |
| Informing students about the internship before they begin working | 0.43 ± 0.182 | 0.95 ± 0.106 | < 0.001 |
| Dimension score | 0.420 ± 0.064 | 0.859 ± 0.079 | < 0.001 |
| Learning-teaching method | |||
| Aligning instructional approaches with educational objectives and content | 0.46 ± 0.193 | 0.95 ± 0.106 | < 0.001 |
| The level of training obtained during the internship | 0.32 ± 0.183 | 0.86 ± 0.162 | < 0.001 |
| The scope of training obtained during the internship | 0.32 ± 0.153 | 0.75 ± 0.196 | 0.001 |
| Focus on evidence-based education (following clinical standards) | 0.55 ± 0.223 | 0.96 ± 0.091 | < 0.001 |
| Internship compatibility with local and available facilities and technology | 0.39 ± 0.189 | 0.80 ± 0.200 | < 0.001 |
| Including participants in the internship process | 0.39 ± 0.189 | 0.80 ± 0.145 | < 0.001 |
| Student's active learning effort | 0.37 ± 0.214 | 0.96 ± 0.091 | < 0.001 |
| Providing focused internship training | 0.30 ± 0.175 | 0.95 ± 0.106 | < 0.001 |
| Rational enhancement of students' knowledge, attitudes, and abilities | 0.32 ± 0.182 | 0.95 ± 0.106 | < 0.001 |
| Appropriate care and strong cooperation between health center officials and students | 0.39 ± 0.162 | 0.89 ± 0.162 | < 0.001 |
| Adherence to the internship schedule | 0.41 ± 0.186 | 0.88 ± 0.163 | < 0.001 |
| Optimal use of internship time | 0.39 ± 0.162 | 0.88 ± 0.214 | < 0.001 |
| Dimension score | 0.386 ± 0.044 | 0.885 ± 0.052 | < 0.001 |
| Educational evaluation | |||
| Educational evaluation conformity with educational planning and methodologies | 0.30 ± 0.200 | 0.96 ± 0.091 | < 0.001 |
| Evaluation objectivity | 0.41 ± 0.186 | 0.95 ± 0.106 | < 0.001 |
| The availability of relevant evaluation tools | 0.21 ± 0.275 | 0.96 ± 0.091 | < 0.001 |
| A fair and objective review | 0.30 ± 0.223 | 0.95 ± 0.106 | < 0.001 |
| Students achieving high grades | 0.41 ± 0.186 | 0.84 ± 0.158 | < 0.001 |
| The consistency with which grades are assigned to students | 0.39 ± 0.162 | 0.96 ± 0.091 | < 0.001 |
| Expensive and time-consuming internship evaluation | 0.55 ± 0.223 | 0.86 ± 0.162 | 0.014 |
| Optimal utilization of available resources | 0.39 ± 0.189 | 0.82 ± 0.153 | < 0.001 |
| Developing critical thinking skills in order to evaluate system performance | 0.41 ± 0.186 | 0.96 ± 0.091 | < 0.001 |
| Students assist healthcare workers | 0.46 ± 0.091 | 0.93 ± 0.117 | < 0.001 |
| The evaluation's coverage of knowledge, attitude, and skill | 0.34 ± 0.210 | 0.98 ± 0.067 | < 0.001 |
| Dimension score | 0.381 ± 0.063 | 0.925 ± 0.022 | < 0.001 |
| Total score | 0.392 ± 0.029 | 0.894 ± 0.036 | <0.001 |
Student Satisfaction from the Old and New Approaches
The analysis of student satisfaction levels, based on predetermined statistical cut-off points, reveals significant differences before and after implementing a new approach to internships. Prior to the intervention, 50% of students reported low satisfaction levels, while the remaining 50% indicated moderate satisfaction levels. Notably, no students reported very poor, good, or very good satisfaction levels. However, following the implementation of the new approach, all students reported very good satisfaction levels (Figure 2).
5. Discussion
This study aimed to enhance the hospital internship course for nutrition students by employing a comprehensive checklist for nutritional assessment and patient treatment. The initial evaluation of the internship approach highlighted numerous areas for improvement. Identified challenges in the design and execution of internships included inadequate and unscientific needs assessment, undefined and ambiguous goals stemming from a lack of beneficiary needs assessment, unclear student expectations, insufficient utilization of portfolio capabilities, poor coordination with healthcare sectors leading to suboptimal training quality, subjective and unscientific student evaluations, and the absence of objective evaluation tools. Furthermore, students often fail to attain the desired knowledge and skills after completing the internship course.
Heidari et al. identified similar issues in public health internships at Golestan University of Medical Sciences. Challenges highlighted in their study included deficiencies in the educational system, such as the insufficient knowledge of healthcare workers about internship training programs, a disconnect between theoretical coursework and practical internships, and a lack of confidence in non-clinical fields. Additional concerns included student-related issues, such as low self-confidence in administering care and a lack of enthusiasm for hands-on learning among some trainees. Challenges in the planning and preparation phase of internships were also noted, including inadequate skills training planning, insufficient pre-internship briefings, and unclear expectations for student performance (19).
Furthermore, there are issues with internship management, such as a weak connection between the educational field in the university and care areas, a reduction in the diversity of available internships, the elimination of certain visits, and a lack of communication between students in different fields within the group to exchange opinions and experiences. In addition, internship challenges may include inadequate facilities and equipment for student training, limited personnel cooperation due to workload, and a restricted number or diversity of clients in specific centers. The monitoring and evaluation of students, including the inadequacy of the design logbook and infrequent visits from students in care fields, have been identified as areas of concern (19).
Moghimi et al. conducted a study to identify obstacles in clinical education and suggest solutions to improve the quality of education for nursing students at Yasouj University of Medical Sciences. The study revealed several issues, including unclear educational goals, a lack of discipline among students, inadequate scheduling for internships, poor communication between students and staff, insufficient care and educational facilities in clinical fields, and weaknesses in student evaluation processes and tools (20). A study conducted by Abedini et al. aimed to identify internship problems among laboratory science students at Hormozgan University of Medical Sciences. The study utilized a qualitative approach and identified five main problem areas: Evaluation of internship headlines, expectations from internships, student motivation to participate in internships, student evaluation, and internship management and planning (21).
Sadegh Tabrizi et al. conducted a qualitative study titled "The Views of Public Health Services Management Students at Tabriz University of Medical Sciences Regarding Internships." The study aimed to investigate students' perspectives on the internship unit of health service management and family health. The study findings indicate significant challenges in the internships discussed, particularly in three key domains: Lesson planning (about planning, lesson plans, and educational resources), readiness for acquiring knowledge and skills (including briefing sessions, coordination between faculty and field, collaboration with healthcare professionals, field training, practical work, and the presence of a trainer), and internship evaluation (comprising final exams, work reports, attendance and absence, and satisfaction of officials and employees). Enhancing the educational curriculum in these fields was deemed necessary, particularly in internships and technical skill acquisition (22).
An analysis of students' academic achievement, as determined by the scores obtained from the evaluations administered before the aforementioned promotion, reveals that their proficiency levels in patient evaluation, treatment measures, and overall performance were 29%, 59%, and 40%, respectively. Additionally, the current levels of student satisfaction with educational planning, learning-teaching methodologies, educational evaluation, and overall satisfaction were 42%, 38%, 38%, and 39%, respectively. In comparative research, Rasouli and Afkhamzadeh's study reported 82% satisfaction among Iranian medical students with internships (9).
Investigations into the impact of the interventions on students' performance during internships indicate significant improvements. Specifically, students' performance in "patient assessment" increased from 29% to 95%, while their performance in "patient treatment" improved from 59% to 100%. Overall, students' performance increased from 40% to 97%. Furthermore, the investigation into the impact of the aforementioned interventions on student satisfaction reveals a significant increase in their satisfaction levels. Specifically, satisfaction with educational planning rose from 42% to 85%, satisfaction with the learning-teaching methodology dimension increased from 38% to 88%, satisfaction with the educational evaluation dimension improved from 38% to 92%, and overall satisfaction increased from 39% to 89%.
A study was conducted to enhance the quality of healthcare management internships in Tabriz, utilizing an action research approach and the Simmons model. The results indicated a statistically significant increase in overall satisfaction levels with the internship process, from 60% to 81%, reflecting a 21% increase (21). In a recent study, the objective was to compare the impact of two evaluation methods—electronic and conventional portfolios—on the satisfaction levels of operating room students at Qom University of Medical Sciences. The results indicated that the electronic portfolio method was more effective in enhancing student satisfaction across various dimensions, such as fairness of evaluation, relevance of topics to clinical experiences, motivation to learn, instructor mastery in evaluation implementation, feedback from the instructor, motivation to use scientific resources, attention to various evaluation dimensions, and identification and compensation of training deficiencies. The electronic portfolio method yielded a higher-than-average score of 11.5 compared to the usual score of 6.6, and this difference was statistically significant.
According to a study conducted by Tabrizi et al., an objective structured clinical exam was implemented to enhance the final evaluation of healthcare management students enrolled in the internship course at the Tabriz Faculty of Health and Nutrition. The results indicated that 74% of the students found this method effective in assessing their capabilities. At the start of the semester, 70% of the students demonstrated a strong understanding of the internship process and the associated educational expectations. Additionally, 58% of the students perceived the evaluation process, including the grades obtained, as equitable (23).
A study revealed that simulating Nutrition-Focused Physical Exam (NFPE) skills improved students' comfort with touching patients and their self-rated abilities to assess subcutaneous fat, muscle stores, fluid accumulation, and micronutrient deficiency in nutrition students (24). Another study indicated that incorporating simulated patients into clinical nutrition courses increases dietetics students' and interns' communication and nutrition-care competence (25). A qualitative study showed that a supervised practice program benefited nutrition students by bridging the gap between classroom didactic knowledge and practice, improving workplace self-confidence, and developing competencies such as critical thinking, communication, interviewing, and counseling skills in various multidisciplinary and multicultural settings (26).
A similar study confirmed that implementing appropriate nutritional education in residency and specialty training reduced morbidity and mortality. Malnutrition, including obesity, remains highly prevalent in hospitals and plays a major role in nearly every major chronic disease that affects patients (27). A study demonstrated that expanding a clinical nutrition curriculum in pre-clerkship courses significantly improved medical students' self-assessed knowledge regarding counseling patients, their comfort with completing a nutritional assessment, and their confidence in advising patients about nutrition (7).
Another study proposed an online module that medical students could use as a self-study activity to learn about key signs for diagnosing malnutrition and the nutrition interventions available in a hospital setting. In that study, there was a significant difference in mean scores between students who completed the module and post-module survey compared to the overall student population before having access to the module (28). The same study showed that adding nutrition education sessions for senior medical students led to statistically significant improvements in their confidence in the measured domains, as well as in their performance and knowledge scores (29). A similar study concluded that a nutrition curriculum for medical students improves students' confidence, knowledge, and skills related to nutrition counseling, even when controlling for personal nutrition-related behaviors (30).
According to the findings of this study, it may be beneficial to consider implementing a comprehensive checklist for evaluating and providing nutritional treatments in internship courses within hospitals and related fields. This approach has positively impacted disease assessment, patient treatment, and overall student performance. Furthermore, the tool has demonstrated significant and positive effects across various satisfaction domains, such as educational planning, learning-teaching methodology, educational evaluation, and overall satisfaction. One of the notable strengths of this study is its innovative approach to designing a comprehensive tool for evaluating and providing nutritional treatments. The tool was developed with input from a diverse group of experts, which helped ensure its effectiveness.
The study also included a tool for measuring student satisfaction with their internship experience. Additionally, it is worth noting that this study demonstrated excellent psychometric properties and content validity of the questionnaires, as evaluated by experts in the field. One potential limitation of this study is the limited availability of comparable studies, particularly in Iran, which could have provided valuable context for interpreting the results. It was observed that there is currently a lack of research on the evaluation and promotion of internships in the field of nutrition, highlighting the need for further investigation in this area.
5.1. Conclusions
The study emphasizes the importance of conducting a thorough needs assessment in educational fields, considering the perspective of beneficiaries, and analyzing the root causes of identified deficiencies. Additionally, implementing innovative and targeted promotional interventions can lead to improved student performance and satisfaction. It is suggested that other medical science universities consider utilizing the approach and tool presented, as clinical nutrition science has been shown to significantly impact the treatment of various diseases. This is particularly relevant given the practical nature of the theoretical knowledge acquired by students in clinical and care fields. The framework and approach used in this study may enhance internship courses for students in various fields of study.