1. Background
Appendicitis is the most common cause of acute abdominal pain, which requires surgery, and appendectomy is the most frequent surgical procedure performed around the world (1, 2). Traditionally, open appendectomy has been the standard treatment for appendicitis, which is usually performed through classic incision at McBurney’s point or through Rockey-Davis transverse incision at the right lower quadrant (3). Nevertheless, with time, it has been learnt that standard incision has its own drawbacks, such as large scars, hernia, and postoperative pain (4-6).
Over the decades, techniques for appendectomy have evolved towards less invasive procedures. Recently, laparoscopic appendectomy has widely become accepted, yet there is controversy over the best method for appendectomy (7, 8). Many surgeons have been encouraged to use a variety of incisions for abdominal visceral surgery that are hidden from exposure and have tried to introduce cosmetically better incision for open appendectomy (7, 9-13). Malik et al. introduced a new small access incision lateral to McBurney’s point and showed that appendectomy using this method is feasible in children (14).
2. Objectives
This randomized controlled trial aimed at studying the safety and feasibility of open appendectomy using small access incision in pediatric and adult patients and comparing this method with the classic McBurney’s incision.
3. Methods
3.1. Patient Selection
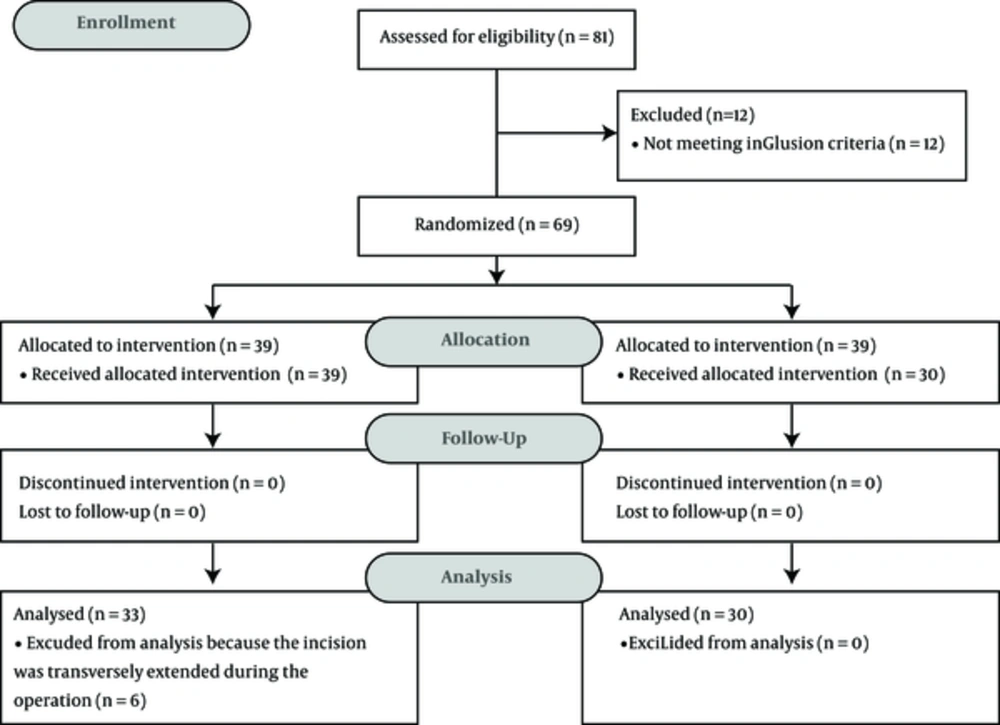
This study was a single center, randomized controlled clinical trial. Eighty-one patients with the diagnosis of acute appendicitis, who entered the emergency department of Besat hospital, Hamadan University of Medical Sciences, Iran, during year of 2016, were enrolled in the study. Inclusion criteria included patients in whom appendicitis was documented clinically or with the help of computed tomography scan results plus Alvarado score of more than five (15, 16). Patients, who revealed no signs of appendicitis at surgery and patients with signs and symptoms of perforation peritonitis and its complications, including abdominal guarding, diffuse abdominal rigidity, development of ileus paralyticus, shock, acute renal failure, peritoneal abscess, and sepsis, in addition to patients with marked overweightness defined as body mass index of more than 25, were excluded from the study (n = 12). Sixty-nine patients were randomly allocated to 2 groups, using the simple randomization method with a random number table. Patients, who underwent open appendectomy using small access incision, were considered as the case group (n = 39) and the others, who underwent open appendectomy using classic McBurney’s incision, were considered as the control group (n = 30). The CONSORT flow diagram showing the process of patient selection is depicted in Figure 1.
3.2. Surgery
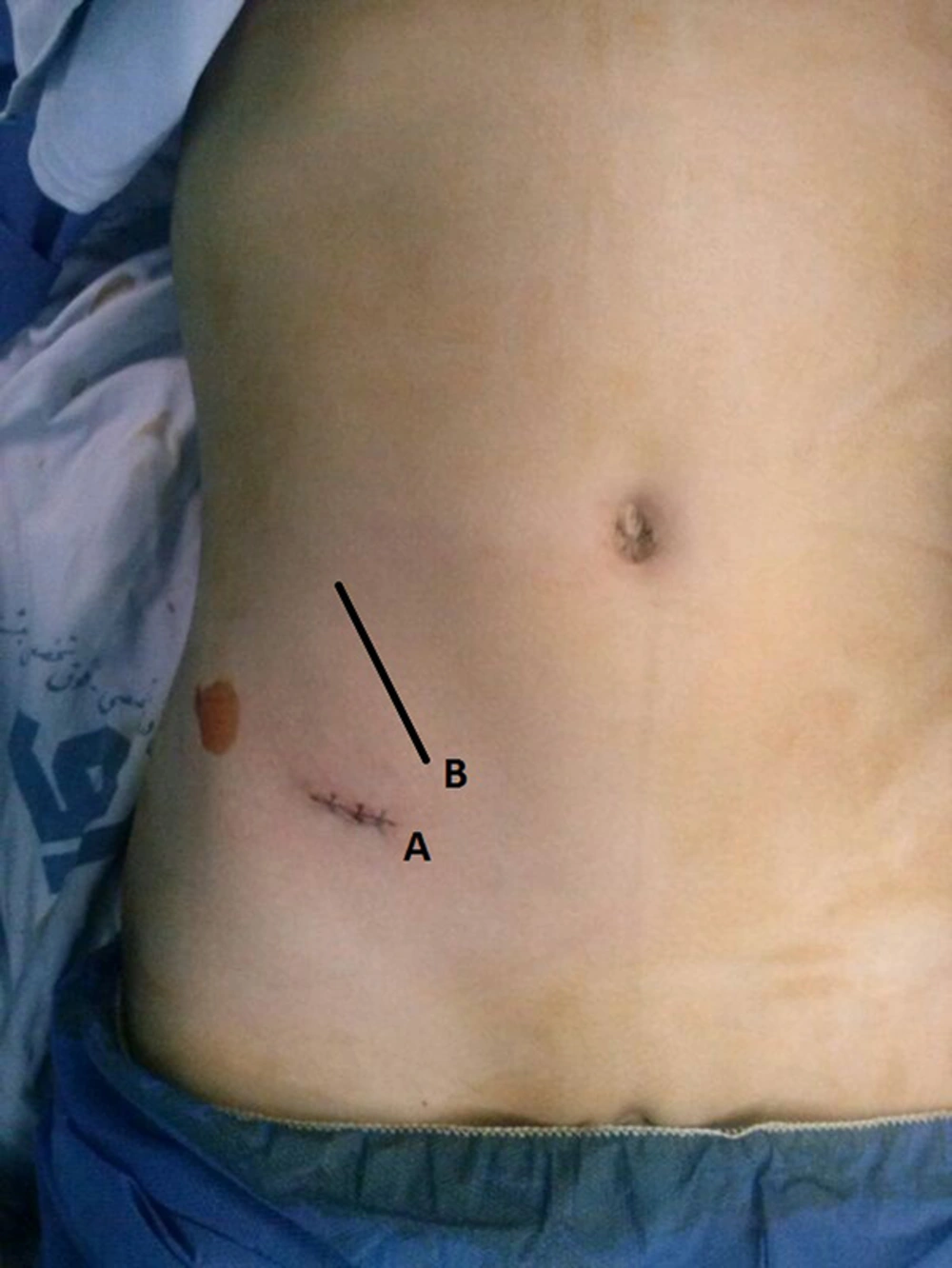
The researchers introduced an incision by deriving and modifying the formerly limited open incisions in the literature (10, 11, 13, 14, 17). Thirty-nine patients underwent open appendectomy using a small access incision. A skin crease incision of 2 centimeters long was made at 2 centimeters medial and 2 centimeters below the anterior superior iliac spine. External oblique fibers were cut and the internal oblique and the transverse muscle fibers were split in the direction of the fibers. Two Langenbeck retractors were used to retract the fibers. Peritoneum approached, is picked up with hemostats and cut in the line of the skin incision. A taenia was recognized by pulling on to the caecum, and was held with a Babcock’s forceps. The appendix was pulled into the wound with the use of 2 Babcock’s forceps, walking down the taenia to the base of the appendix. A window was made in the meso-appendix and ties were applied. Thirty patients underwent open appendectomy using classic McBurney’s incision as an oblique incision made in the right lower quadrant of the abdomen, placed at the junction of lateral one-third and medial two-third of the spinoumbilical line (3). The locations of the 2 incisions are depicted in Figure 2. All appendectomy surgeries in both groups were performed by the same surgeon with only the use of instruments and without inserting hands in the abdominal cavity.
3.3. Study Protocol
Informed consent was obtained from each patient after explaining the probable advantages and disadvantages of appendectomy, using small access or classic McBurney’s methods. The study was approved by the ethics committee of Hamadan University of Medical Sciences and Iranian registry of clinical trials with registration number of IRCT201411288729N7.
During the hospital stay and after the operation, all patients were visited every 6 hours by the surgeon and the data of the patients, including demographics, operative time, days of hospitalization, and analgesic consumption during the hospital stay were recorded in a separate questionnaire for each patient. The operative time was considered from performing the incision of skin to the last suture. Each operative time was measured by 2 different individuals and the average was recorded as the operative time. Surgical site pain was scored from 0 to 10 by the patients and patients with a pain score of more than 5 were administered meperidine intramuscularly with a dose of 1.5 mg/kg. Patients were discharged based on having a good general condition, no fever, no nausea/vomiting, and peritonitis. All patients were visited by the same surgeon 1 week after the operation for surgical wound infection, hematoma and seroma, and 6 months after the operation for assessment of satisfaction with the scar appearance and incisional hernia.
3.4. Statistical Analyses
Statistical analyses were performed using the SPSS statistical software (IBM SPSS Statistics for Windows, Version 20.0, IBM Corp., Armonk, NY, USA). The Fischer’s exact test was used for analysis of qualitative data and the independent t test was used for comparison of quantitative data between the 2 groups. P values of less than 0.05 were considered statistically significant.
4. Results
During the study period, 69 patients with a diagnosis of acute appendicitis, having no signs and/or symptoms of peritonitis and its complications were enrolled in the study. Thirty-nine patients underwent appendectomy using Small Access incision (SA group) and the others underwent classic McBurney’s appendectomy (CA group). In 6 patients in the SA group (15%), the incision was transversely extended during the operation.
The overall mean age was 19.3 ± 10.4 years (range = 5 to 47), including 45 males (65%). The SA group included 29 males (74.3%) with a mean age of 20.2 ± 11.3 years (range = 5 - 47), and the CA group included 16 males (53.3%) with a mean age of 18.2 ± 9.3 years (range = 6 - 37), without any significant difference between the 2 groups (P values being 0.41 and 0.8 for SA and CA group, respectively). The number of patients with an age of under 15, was 15 in the SA group compared to 14 in the control group (P value = 1). The mean age of the patients in whom the small access incision was transversely extended during the operation was 33.8 ± 8.6 years old, which was significantly higher than patients in whom the appendectomy was successfully performed through the small access incision with a mean age of 17.8 ± 10 years old (P value = 0.001).
The early and late postoperative data of the patients in the SA group, including 6 patients in whom the small access incision was transversely extended, and the CA group are shown in Table 1. Moreover, the per-protocol analysis and the early and late postoperative data of the patients in the SA group, excluding the 6 patients in whom the small access incision was transversely extended, and the CA group are shown in Table 2. Expectedly, when the 6 patients in whom the small access incision was transversely extended were included in the analysis, the operative time was significantly longer than the CA group, which was not applied after excluding these 6 patients from the analysis. However, the other comparisons were not different between the 2 analyses.
| Variables | Total (N = 69) | SA Group (N = 36) | CA Group (N = 30) | P Value |
|---|---|---|---|---|
| Operative time, min | 28.7 ± 11a | 31.3 ± 11.3 | 25 ± 9.5 | 0.023 |
| Hospital stay, hrs | 40.4 ± 17.2 | 38.3 ± 17.4 | 43 ± 16.9 | 0.26 |
| Pain medication during hospital stay, mg | 122.1 ± 31.7 | 112.8 ± 30.3 | 134 ± 29.7 | 0.005 |
| Surgical complications | ||||
| Early | ||||
| Wound infection, No. (%) | 3 (4) | 2 (5) | 1 (3) | 0.5 |
| Hematoma | 0 | 0 | 0 | |
| Seroma | 0 | 0 | 0 | |
| Late | ||||
| Incisional hernia | 0 | 0 | 0 | |
| Hypoesthesia of proximal of right thigh | 0 | 0 | 0 |
Abbreviations: CA, Classic McBurney’s Appendectomy; SA, Small Access.
aMean ± standard deviation.
| Variables | Total (N = 63) | SA Group (N = 33) | CA Group (N = 30) | P Value |
|---|---|---|---|---|
| Operative time, min | 27.5 ± 10a | 30 ± 10 | 25 ± 9.5 | 0.07 |
| Hospital stay, hrs | 41.2 ± 17 | 39.6 ± 17.3 | 43 ± 16.9 | 0.42 |
| Pain medication during hospital stay, mg | 121.4 ± 31.7 | 110 ± 29.2 | 134 ± 29.7 | 0.002 |
| Surgical complications | ||||
| Early | ||||
| Wound infection, No. (%) | 3 (5) | 2 (6) | 1 (3) | 0.41 |
| Hematoma | 0 | 0 | 0 | |
| Seroma | 0 | 0 | 0 | |
| Late | ||||
| Incisional hernia | 0 | 0 | 0 | |
| Hypoesthesia of proximal of right thigh | 0 | 0 | 0 |
Abbreviations: CA, Classic McBurney’s Appendectomy; SA, Small Access.
aMean ± standard deviation
In the SA group, 22 patients (67%) received general anesthesia, which was not significantly different compared to the 19 patients in the CA group (63%). The others received spinal anesthesia. The number of patients, who had seen the appendectomy scar of others were 19 (57.6%) in the SA group, compared to 18 (60%) in the CA group, which was not significantly different (P value = 1). The amount of pain medication administered during the hospital stay in the SA group was significantly lower than the CA group (110 ± 29.2 mg vs. 134 ± 29.7 mg and P = 0.002). The median satisfaction score of patients with their appendectomy scars was 5 out of 5 in the SA group, being significantly higher than the CA group, with the median satisfaction score of 3 out of 5 (P value < 0.001). The data of 6 patients in the SA group, in whom the incision was transversely extended during the operation, is shown in Table 3.
| No. | Gender | Age | Cause |
|---|---|---|---|
| 1 | Male | 21 | Failure to move bowel back |
| 2 | Male | 37 | Suspicious for intra-abdominal bleeding |
| 3 | Male | 29 | Adhesions |
| 4 | Female | 47 | Adhesions |
| 5 | Male | 34 | Adhesions |
| 6 | Male | 35 | Inaccessibility to the appendix |
5. Discussion
For many years, the procedure of open appendectomy has been developed toward a less invasive surgery. Although, laparoscopic appendectomy has widely been accepted, there is still no consensus over the best technique for appendectomy and yet laparoscopy is not the treatment of choice for appendicitis (1, 7, 18, 19). Some studies have shown that laparoscopic appendectomy is superior to traditional open surgery in terms of lower hospital stay, faster recovery, and less postoperative pain and infections (20-22). However, others failed to show the advantages of laparoscopic appendectomy and proposed that open appendectomy remains the most cost effective method for patients with acute appendicitis (19, 23, 24). Moreover, there are some disadvantages to laparoscopic appendectomy, such as longer operative time, higher rates of intra-abdominal abscess, and higher failure rates in patients with complicated appendicitis (25-28). Furthermore, laparoscopic facilities are not easily available in every center of developing countries.
Traditionally, open appendectomy is commonly performed through classical incision at McBurney’s point at the junction of the lateral and middle thirds of a line joining the right anterior superior iliac spine and the umbilicus (3). For many years, some modifications, such as using smaller incisions have been proposed in order to reduce incisional morbidity and improve cosmetic outcomes, compared to the classic method. Even so, very few authors have worked on this subject and the area of the most common emergency visceral surgery has remained without an established minimally invasive incision.
A new small access incision was introduced by Malik et al., in 2007, for children (14). The incision is 1.5 to 2 cm in length, located in the middle third of the lateral third of the spinoumbilical line, lateral to McBurney’s point. It has been shown that appendectomy using this method is feasible in children with advantages of less postoperative pain, shorter hospital stay, and better cosmesis (14). Delany et al. introduced bikini incision for appendectomy in the lateral low transverse position, located below the pubic hair line, which extends from approximately 2 to 3 cm below the anterior superior iliac spine, medially across the inguinal ligament to approximately 1 cm from the midline (10). Sanjay et al. introduced mini-appendectomy incision, which is started on the lateral border of rectus muscle and extend transversally 2.5 to 3.5 cm towards McBurney’s point (5, 13). O’Neill et al. introduced the modified Lanz incision, which provides cosmetic scar and better access to appendix in difficult cases (17). The incision starts 2 cm below and medial to the right anterior superior iliac spine and extends medially for 5 to 7 cm. In the current study, for cosmetic reasons, the small access incision was located 2 centimeters below the anterior superior iliac spine in lower abdominal skin crease, under the bikini line. Moreover, for safety reasons and in order to avoid entering the pre-peritoneal space, the incision was located 2 centimeters medial to the anterior superior iliac spine. The incision was small without much muscle/nerve derangements, hence the researchers could not encounter any case of incisional hernia in the 6-month follow up period. Compared to the CA group, using small access incision was feasible and safe in both pediatric and adult patients, which was associated with significant higher rate of satisfaction and lower rate of postoperative pain. It should also be noted that in the SA group, a large number of parents with a history of open appendectomy through the McBurney’s incision were very pleased with the scar of small access incision in their children. In contrast, the current study showed that there was no difference between the 2 groups, in terms of hospital stay and rates of early and late surgical complications. The advantages of small access incision are that it is cosmetically pleasing and well-hidden by most bikinis and since it is placed directly above the caecum, the surgeon has better access for recognition and delivery of the caecum and the appendix through the small incision. In the current study, similar to Malik’s work, the drawbacks of using the small access incision for appendectomy were inability of delivering back the bowel loops to the wound, and finding the retrocecal appendicitis and releasing the bowel adhesions in a few cases, in whom the incision was changed to classic McBurney’s.
In summary, open appendectomy using small access incision may be a safe, feasible, and very cosmetically pleasing method in adult and pediatric patients. However, it should be noted that this new incision may be more appropriate for young adult patients and is not a substitution for classic McBurney’s incision in all patients. Finally, establishment of a minimally invasive surgery for appendectomy needs further evaluation of small access incision for appendectomy, with respect to its comparison with laparoscopic approaches.