1. Context
Human sexual function is influenced by a complex interplay of biological and psychological mechanisms. These mechanisms encompass physiological responses like libido, arousal, orgasm, and ejaculation, and in females, hormonal regulation through the menstrual cycle. A breakdown in these areas may lead to sexual dysfunction (1). This problem is also commonly observed following treatment with antipsychotics; however, the extent of the effect varies considerably depending on the specific medication used (2). This medication-induced side effect disrupts various physiological processes essential for sexual function, encompassing desire (libido), arousal (lubrication/erection), and orgasm (3). Evaluation of this dysfunction can be challenging due to its sensitive nature and patients' reluctance to disclose it, often leading to missed diagnoses by healthcare providers.
Atypical antipsychotic treatment is the main component of mental disorders treatment (4). Antipsychotic-induced sexual dysfunction likely arises from a convergence of mechanisms. These include elevated prolactin levels (hyperprolactinemia), sedative effects of the medications, and their ability to block the activity of specific neurotransmitter receptors in the brain (α-adrenergic, dopaminergic, histaminic, and muscarinic). Atypical antipsychotics (AAP) may cause sexual dysfunction by blocking dopamine D2 receptors in the pituitary gland, leading to increased prolactin release. Despite this, a clear link between elevated prolactin levels and the severity of sexual side effects has not been established. Impaired sexual function in individuals receiving treatment for mental illnesses can negatively impact their quality of life, including mood, self-esteem, medication adherence, and overall treatment success (4).
Dopamine agonists are well-established to induce compulsive behaviors. Atypical antipsychotics, including aripiprazole, olanzapine, quetiapine, and risperidone, have also been associated with the emergence of pathological gambling, hypersexuality, compulsive eating, and shopping, potentially leading to significant social and familial disruptions. Notably, these compulsive behaviors often improve or resolve entirely with discontinuation or replacement of the medication. Given these potential side effects, it is crucial to inform patients about them and monitor for any behavioral changes. Management strategies may involve dose reduction, discontinuation, or switching to a different antipsychotic if these compulsive behaviors arise (5).
2. Objectives
The present study reported hypersexuality symptoms in a schizoaffective (bipolar type) female patient who received quetiapine and experienced increased sexual frequency and preoccupation. Moreover, hypersexual cases taking quetiapine were systematically searched to review the relationship between quetiapine and hypersexuality.
3. Case Report
Written informed consent was obtained from the patient to publish this case report. The following data were extracted from the patient’s medical documents.
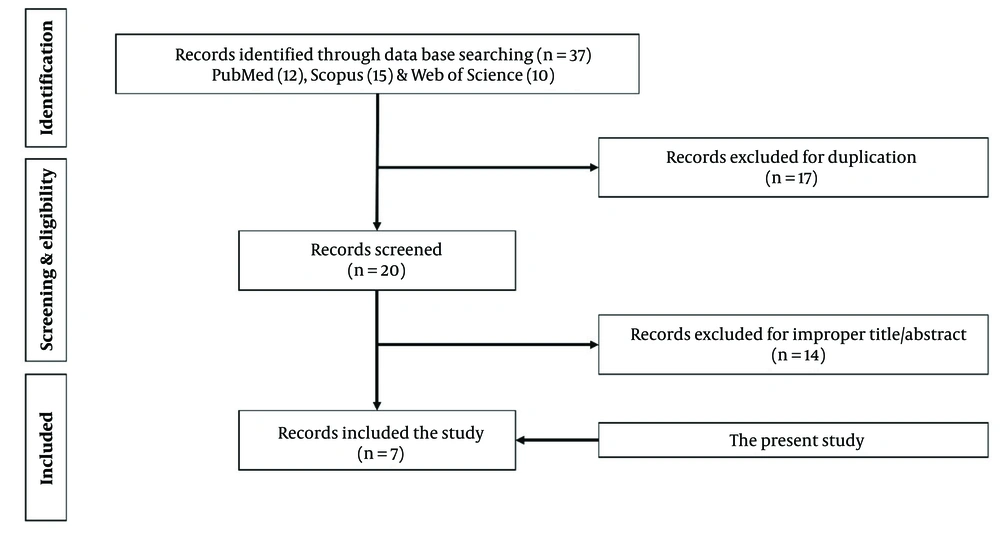
Cases of hypersexuality after taking quetiapine were identified through a systematic review of the literature according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guideline. The search was performed without time restriction until November 16, 2022. The terms "Compulsive sexual behavior", "Hypersexuality", "Sexual addiction", "Libido", "Compulsive sexual disorder", "Sexual compulsivity", "Hypersexual", and "Quetiapine" were searched in PubMed, Scopus, and ISI Web of Knowledge databases. All case reports and case series were included, and secondary studies, animal studies, in vitro studies, editorials, clinical trials, and letters to the editor were excluded. The references of publications were reviewed to identify additional cases. Extracted data include authors, year, age, sex, underlying diseases, medication types, medication dose, the effect of medication, and treatment trends.
4. Results
4.1. Case Presentation
The patient was a 33-year-old schizoaffective, bipolar-type female. She suffered from auditory hallucinations, persecutory delusions, insomnia, decreased appetite, and suicidal ideas, and in some episodes, hyper-religious thought and function and grandiosity delusion were seen in her. Her disorder began 14 years ago when she was 19 years old. In her illness from 14 years ago, she was admitted twice to the educational psychiatric ward and received three outpatients electroconvulsive therapy (ECT). She had been prescribed carbamazepine, lithium, fluoxetine, and perphenazine before.
Last time, she came to the clinic with persecutory delusion, agitation, and auditory hallucination and received risperidone 12 mg/day, trihexyphenidyl 4 mg/day, and lithium 1200 mg/day for six months. Due to not influencing to reduce symptoms, her medication was changed to 100 mg/day of quetiapine, and after three days, to 200 mg/day. After this medication change, her sexual urges and activities increased. Her libido increased within five days after the initiation of the drug. Her husband reported her hypersexuality by the demand three times per day for sexual intercourse. She had never exhibited these behaviors before her disorder and had two times weekly intercourse with her husband before that time. Clinical assessment and laboratory evaluations revealed no deviations from expected findings. To the best of our knowledge, the patient reported no use of over-the-counter medications during the treatment period. The patient did not have another drug consumption with quetiapine and had no gynecology problem or hypersexuality history during her disease.
Regarding her hypersexuality, the dose of medication did not increase. After one month, because of this problem, quetiapine was discontinued, and upon cessation of quetiapine, her high libido level subsided to her baseline after two weeks. After that, she was treated with prescribed haloperidol 20 mg/day, propranolol 60 mg/day, clonazepam 2 mg/day, and trihexyphenidyl 6 mg/day. After three months, the patient’s symptoms were under control, and she showed good function and had no complications.
After one year, quetiapine 25 was again added to the treatment regimen, and after one week, hypersexuality symptoms appeared. After stopping the drug, the symptoms disappeared after two weeks.
4.2. Review on Published Cases of Hypersexuality After Taking Quetiapine
A literature search identified 37 records (detailed in Figure 1). After removing 17 duplicates, the titles of the remaining 20 articles were screened for relevance. Finally, in addition to the present study, six case-report studies presented the relationship between hypersexuality and quetiapine was further investigated.
The selected studies included eight cases, six males and two females aged between 17 and 70. The study characteristics are shown in Table 1.
| Author | Year | Sex | Age | Underlying Disease | Medication (s) | Manifestation | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|
| Cannas et al. (6) | 2006 | Male | 51 | Parkinson | Pergolide slowly increasing dose up to the established 1 mg/t.i.d. | Increase in libido, with hyper libidinous behaviors and demands for frequent sexual intercourse, or intimate contact | Reducing pergolide to 0.25 mg/t.i.d and adding quetiapine 25 mg in the morning and afternoon and 125 mg at night | Easily control sexual urges, and a mild degree of pathological jealousy indicating paranoid delusions. |
| Chae and Kang(7) | 2005 | Male | 63 | Stroke | Haloperidol titrated to 5 mg/day, bupropion100 mg/day, flunitrazepam titrated to 2 mg, carbamazepine titrated to 400 mg/day | Repeatedly demanded sexual intercourse and doubted his wife's chastity. | Quetiapine 50 mg twice a day and zolpidem 10 mg at bedtime | Remarkably decreased demanding sexual intercourse and expressing delusional jealousy two days after treatment. |
| Demir et al. (8) | 2012 | Male | 17 | Steroid-induced psychosis | Intravenously administered prednisolone 25 mg per day. | Abnormal sexual behavior towards female medical staff and wanting to engage in sexual intercourse | Quetiapine at an initial dosage of 300 mg/day and increasing to 900 mg/day | Improvement in the symptoms in the second week was resolved by the fourth. |
| Xu et al. (9) | 2022 | Male | 70 | Parkinson and Othello syndrome | Pramipexole 0.75 mg/day titrated up to 1.5 mg/day and selegiline 1 mg/day | Obvious increase in libido presenting as frequent masturbation | Reduction of pramipexole to 50%, and adding quetiapine 25 mg/day | Substantially alleviated OS and hypersexuality after two months. |
| Menon et al. (3) | 2006 | Male | 44 | Schizophrenia | Quetiapine is 200 mg daily, increased to 400 mg on day 2 and to 600 mg on day 4, and 750 mg exactly 1 month later. | Increased spontaneous ejaculations at night, increased need to have sex, especially with himself | - | decrease in the sexual symptoms after 4 - 6 weeks of taking quetiapine 750 mg/day at outpatient follow-up |
| Meyer et al. (10) | 2022 | Male | - | Bipolar disorder | Quetiapine 600 mg/day, lithium carbonate LP 400 mg/day, dulorazepam 1 mg and ½ tablet of zopiclone 7.5 mg | Libido | Reduction of the quetiapine dosage to 500, then 400 mg/day | Regressing symptomatology after a few months |
| 2022 | Female | - | Bipolar disorder | Quetiapine 250 mg/day, combined with oxazepam | Sexual activation | Olanzapine 10 mg/day | Rapid episode resolution in 7 days | |
| Current study | 2022 | Female | 33 | Schizoaffective, bipolar-type | 100 mg/day of quetiapine, and after three days, to 200 mg/day | Sexual activation and libido | Removing quetiapine and adding haloperidol 20 mg/day, propranolol 60 mg/day, clonazepam 2 mg/day, and trihexyphenidyl 6 mg/day | Control for three months without complications |
Among eight reported patients indicating hypersexuality, four male cases were treated by adding quetiapine to the treatment regimen in a range of 25 up to 900 mg per day. A case of Parkinson’s expressed libido and demands for frequent sexual intercourse or intimate contact following 1 mg/t.i.d that could control sexual urges after reduction of pergolide to 0.25 mg/t.i.d and adding quetiapine 25 mg in the morning and afternoon and 125 mg at night (final dose of 175 mg/day) (6). An increase in libido presenting as frequent masturbation was observed in a case of Parkinson’s and Othello syndrome treated with pramipexole 0.75 mg/day titrated up to 1.5 mg/day and selegiline 1 mg/day. The patient was managed by reducing pramipexole to 50% and adding quetiapine 25 mg/day, which substantially alleviated OS and hypersexuality (9). A subject of stroke presented repeatedly demanded sexual intercourse and doubted his wife’s chastity by receiving haloperidol titrated to 5 mg/day, bupropion 100 mg/day, flunitrazepam titrated to 2 mg, and carbamazepine titrated to 400 mg/day. Remarkably decreased demanding sexual intercourse and expressing delusional jealousy was achieved using quetiapine 50 mg twice daily and zolpidem 10 mg at bedtime (7). Moreover, steroid-induced psychosis and abnormal sexual behavior towards female medical staff and wanting to engage in sexual intercourse were observed in a 17-year-old teen, managed by quetiapine at an initial dosage of 300 mg/day and increasing to 900 mg/day (8).
On the other hand, four bipolar and schizophrenia cases (2 males and 2 females) indicated hypersexuality by quetiapine administration. In a schizophrenia patient, spontaneous ejaculations at night and the need for sex were observed by taking daily quetiapine up to 750 mg. However, at outpatient follow-up, these sexual symptoms returned to pre-morbid levels after 4 - 6 weeks of taking quetiapine 750 mg/day (3). Also, a hypersexual bipolar male consuming quetiapine 600 mg/day and lithium carbonate LP 400 mg/day regressed symptomatology after a few months following reduction of the quetiapine to 500 mg/day and then 400 mg/day. Another bipolar female subject presented sexual activation by quetiapine 250 mg/day, combined with lorazepam, treated using olanzapine 10 mg/day (10).
5. Conclusions
Sexual side effects are highly prevalent; however, hypersexuality has been underreported in patients under antipsychotic medications. Based on patients' self-report and physician documentation, sexual adverse effects are about 14% and 58%, respectively (11). A growing body of case reports has suggested that hypersexuality is part of the side-effect profile of atypical neuroleptics or antipsychotics, including aripiprazole, olanzapine, quetiapine, and risperidone (11-13)
On the other hand, sexual dysfunction is also a common side-effect of antipsychotics and AAPs (14). Atypical antipsychotics-induced sexual dysfunction likely arises from a combination of the central nervous system (CNS) and peripheral mechanisms. Central nervous system effects include blockade of dopamine receptors, leading to decreased libido and erectile dysfunction. Additionally, hyperprolactinemia secondary to dopamine blockade may further contribute to these issues. Furthermore, AAPs can exert non-specific CNS depressant effects that may also dampen sexual function (3, 6).
Quetiapine, an antipsychotic medication indicated for the treatment of schizophrenia and acute bipolar mania, and as an adjunctive therapy for major depressive disorder by the U.S. Food and Drug Administration (FDA), is an antagonist for D2 and 5-HT2 receptors and a relatively minor blockade of D2 receptors (15). Quetiapine treatment is not associated with hyperprolactinemia, which may be an advantage. Although some evidence confirmed sexual dysfunction following quetiapine taking (16), some investigations indicated a lower frequency of sexual dysfunction events, such as libido and impaired arousal, with quetiapine than with haloperidol, olanzapine or risperidone (17-19). Meanwhile, several potential pharmacological mechanisms for altered sexual drive involve hypersexuality and libido. In animal models, activation of 5-HT2A receptors enhances sexual behavior, while activation of 5-HT2C receptors may inhibit it. This suggests that the impact of quetiapine and other AAP on sexual function might be determined by their relative binding affinity to these receptors. Quetiapine exerts antagonist effects at 5-HT7 receptors. Preclinical data suggests a potential mechanism for quetiapine's differential effect on sexual function compared to other AAP. 5-HT7 receptor antagonism by quetiapine might counteract the inhibitory effects of serotonin on sexual behavior, as observed with 5-HT7 agonists in female rodents. Furthermore, unlike other AAP, quetiapine and clozapine antagonize α2-adrenergic receptors. This is noteworthy because α2-adrenergic agonists, like clonidine, have been shown to suppress sexual receptivity and proceptivity in animal models. This observation suggests an additional mechanism by which quetiapine may increase sexual drive (3). According to controversial reports, quetiapine's ultimate impact appears to be heavily influenced by the balance between its interaction with central versus peripheral target receptors, and the complex interplay of its effects on various modulatory receptors (4). Furthermore, other factors such as underlying disease, chronic stress, baseline hormonal levels, the cross-activity of medications, and dosage can be responsible for sexual dysfunction. Since the evaluation of adverse drug reactions based on the Naranjo algorithm (20) in the present case in this study and review of the previous cases taking quetiapine confirmed the definite ADR for this medication, quetiapine administration during treatment planning should be done with caution and consideration of possible side effects.
5.1. Conclusions
The present study reported the dual role of quetiapine in hypersexuality in place of four cases indicated it following quetiapine consumption, and four hypersexual cases were treated with medication shifting to quetiapine. As an interesting finding, bipolar and schizophrenia patients presented sexual activation by quetiapine, suggesting a possible involvement of quetiapine signaling pathways in psychological disorders' medication. Although limited case reports have documented hypersexuality associated with AAP, including risperidone, increased sexual drive resulting from quetiapine has been less frequently documented. Some evidence reported improvement in hypersexuality following quetiapine consumption. These findings may present the dual role of quetiapine in sexual functioning. Inadequate patient reporting of side effects, especially sexual dysfunction, can hinder medication evaluation and optimization during treatment. As patients facing adverse effects caused by AAP may have problems with compliance during treatment, it is suggested that clinicians take hypersexuality into consideration, as quetiapine-induced sexual dysfunction poses a potential risk factor for marital discord and patient distress due to misunderstandings by both clinicians and patients.