1. Background
The prison population has been growing in both urban and rural areas (1). Previous reports have indicated that over 87% of Asian countries have experienced an increasing population of prisoners (2). The median rate of prisoners in the world is 145/100 000. This rate has been reported about 229/100 000 in Iran that is more than 160 000 of total population. These rates put Iran among countries with the largest number of prisoners in the world (3). The Iranian correctional system has several features in common with other low-income countries, such as weakness in health care systems and high accumulation in small places (4). Mental health care for prisoners is very important because a current review found that offenders who had psychotic disorders, 40% more of those with nonmentally ill offenders probably committed further offences (5).
Earlier reports that investigated rates of psychiatric disorders in prisoners compared with the general population have been demonstrated a significant difference in the prevalence of psychosis, and depression between the prisoners and general population (6). Other studies showed that substance misuse, psychosis and major depressions are the predictive risk factors for committing suicide in prisoners (7).
Literature review of studies of mental disorders in different regions of our country showed extremely different prevalence rates, as a result of differences in the interview techniques, sampling methods, diagnostic classifications, and tools employed. Previous reports on the prevalence of mental disorders in Iran indicated a high prevalence of psychotic disorders in both male and female prisoners, with major depressive disorder occurring in 31% of male prisoners in Tehran (8) and in 56% of women prisoners in the Bushehr province (9).
To our knowledge, this study was a first review aimed to assess the psychotic disorders and major depression in Iranian prisoners. We also used meta-regression and subgroup analyses to explore sources of heterogeneity in final enrolled studies.
2. Methods
2.1. Search Strategy
We conducted a systematic search of all studies on the prevalence of major depression and other specific disorders in prisoners. We identified publications estimating the prevalence of psychotic disorders by searching in domestic databases such as IranMedex, SID, Medlib, and Magiran and outer databases including Scopus, ISI, PubMed, and Medline library. In this review, articles published between 1 January 1997 and 31 February 2015 were included. Iranian scientific databases were searched only using the keywords including “depression”, “psychotic disorders”, “prisoners” and “personality disorder” and a combination of these words. The search strategy was conducted in the titles of the articles; the following keywords were searched: psych, mental, prevalence, prison, disorder, inmate and Iran Mesh combined with the operator “OR” vs. “AND” and tags “TI” vs. “AD”. We followed the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines (10). This literature search was supplemented by reviewing relevant citations in the initial studies identified, and previous review articles examining similar outcomes.
2.2. Inclusion and Exclusion Criteria
The inclusion criteria were as follows: the subjects should be a representative sample of prison population; tools of diagnoses were made by a two-distinct way clinical examination or completed by expert interviews based on the valid criteria. We excluded studies examining prisoners where overlapping time intervals occurred within the sample collection from the same origin. We excluded prisoners whose STROBE (the Strengthening the Reporting of Observational Studies in Epidemiology) score was under 7.75. Finally, all duplicates and nonrelevant studies were excluded (11, 12).
2.3. Data Extraction
All identified papers and data extraction were performed by two researchers independently. All data appraisal was performed by a structured checklist. The main information includes the author, study population, year of publication, setting, sample selection method, type of study, clinical or interview diagnostic tool, and numbers of prisoners with major depression and psychotic disorders, and STROBE score. Final checklist forms were reviewed by the corresponding author, and the eligible studies enrolled in the final meta-analysis.
2.4. Statistical Analysis
In this study, we used a random effects model to combine the results and meta-regression analysis was also used to find sources of heterogeneity through the subgroup (11). According to this, I2 values above 75% were diagnosed with a significant heterogeneity. In these situations, random effects models are suggested because they produced final weights according to variation between primary studies. The potential publication bias was tested by the Egger’s test that showed a funnel plot in two symmetric or asymmetric (existence of a significant publication bias). Data were analyzed by the Stata statistical software, version 11.2.
3. Results
3.1. Study Characteristics
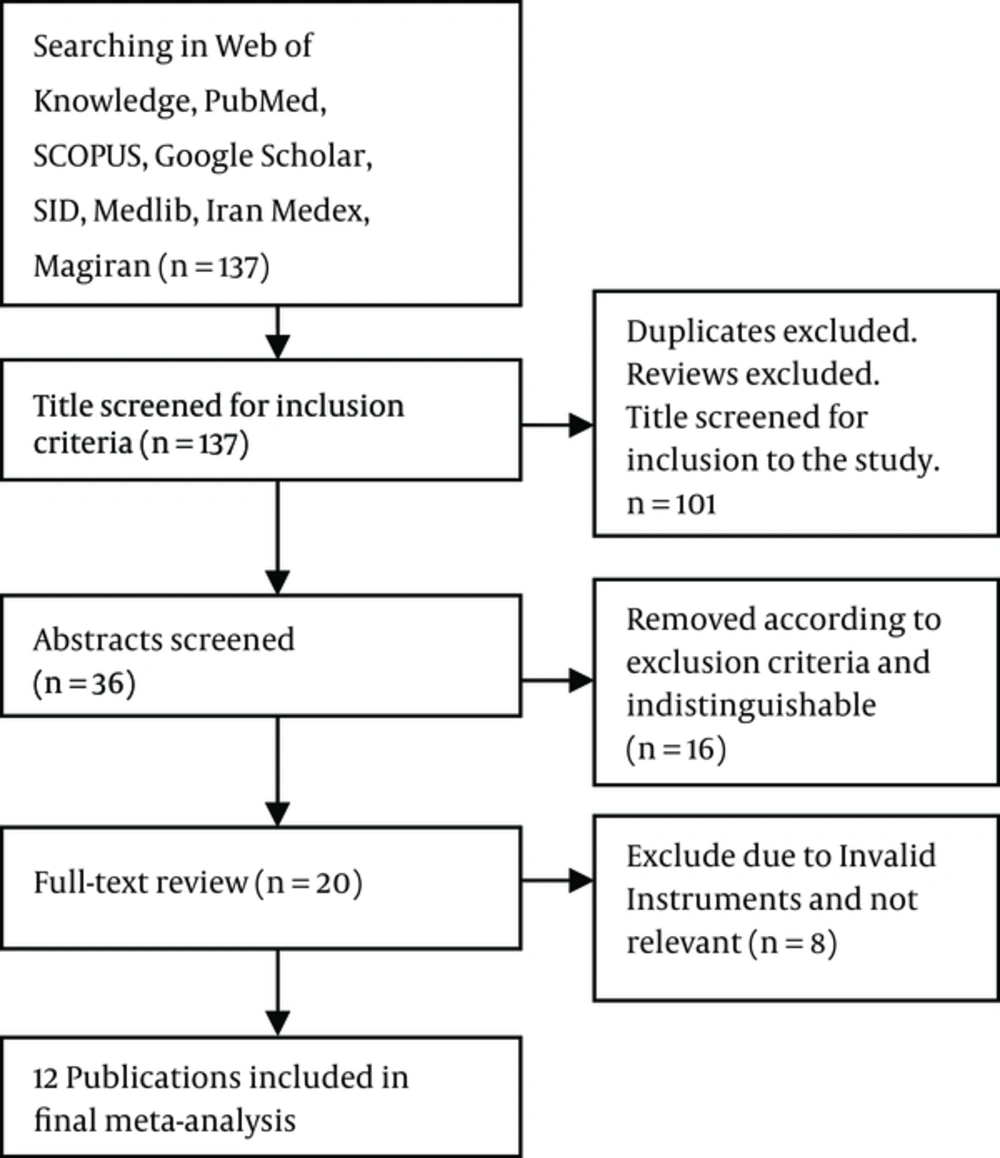
According to the literature search strategies, the final data-set consisted of 12 publications, from the period between 1997and 2015. There were 3 studies in English (3, 13, 14) and 9 studies in Persian (8, 9, 15-21). The pooled sample sizes included a total of 1708 prisoners (Figure 1). Of these, 233 (13.6%) were females with the mean age of 30.5 ± 5.1 years.
3.2. Major Depression
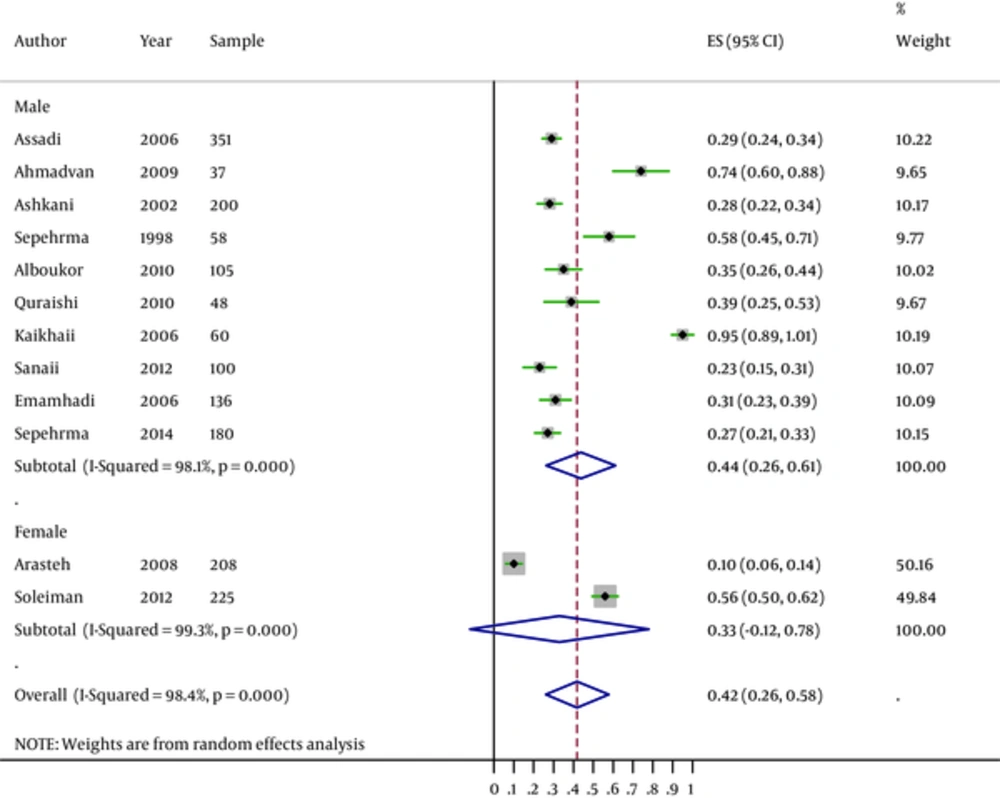
At the end of the systematic review, 12 studies in which major depression was reported in 1708 male and female prisoners were enrolled (Table 1). After the exclusion of two outliers, the pooled prevalence of major depression was 42% (95% CI: 26.0% - 58.0%). In overall, 44% (95% CI 26 - 61) of male prisoners and 33% (95% CI 26 - 58) of female prisoners have had a major depression. A significant heterogeneity was observed in both genders, in males (heterogeneity statistic = 473.79, P ≤ 0.001, I2 = 98.1%, 95% CI 97.2 - 99.4) and also in females (heterogeneity statistic = 138.50, P ≤ 0.001, I2 = 99.3%, 95% CI 98.9 - 99.7). The difference between the prevalence rates of depression in male and female prisoners was statically significant (z = 35.18, P ≤ 0.001) (Figure 2).
| Study Location (Year of Publication) | First Author | Gender | Offense of Prisoners (Number) | Qualitya | Total Sample | Instrument Assessment | Structured Clinical Interview | Specific Disorder | Characteristics of the Sample Were Significant (P Value). | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Any Axis I Disorder (%) | Major Depression (%) | Psychotic Disorder (%) | Mood Disorder (%) | Anxiety Disorder (%) | |||||||||
| Tehran 2006 | Assadi et al. | Male | Non violent (71), Violent (74), Drug (72), Immoral (50), Financial (84) | High | 351 | PCL-SV | DSM–IV | 57.2 | 29 | 3.1 | 30.6 | 7.7 | Age (< 0.001), Education (< 0.001), Time served in prison, (< 0.001), Marital status (< 0.001) |
| Kashan 2009 | Ahmadvand et al. | Male | Drug (37) | High | 37 | BDI | DSM–IV | - | 74.3 | - | - | - | Non |
| Shiraz 2002 | Ashkani et al. | Male | Of all offenses | Medium | 200 | SCL - 90 – R | DSM–IV | - | 28.2 | 5.6 | 41.9 | 8.1 | Non |
| Yazd 1998 | Sepehrmanesh et al. | Teenage male | Of all offenses | Low | 58 | BDI | DSM–IV | - | 58.6 | - | - | - | Personal Housing (< 0.05), Family size (< 0.05) |
| Shiraz 2010 | Alboukordi et al. | Male | Non violent (10), Violent (37), Drug (10), Immoral (21), Financial (27) | High | 105 | BDI | DSM–IV | - | 35.4 | - | - | - | Non |
| Kashan 2010 | Quraishi et al. | Male | Drug(48) | Medium | 48 | GHQ-28 | DSM–IV | - | 39.1 | - | 47.7 | 18.1 | Non |
| Ahvaz 2006 | Kaikhaii et al. | Male | AIDS infected prisoners (60) | Low | 60 | BDI | DSM–IV | - | 95 | - | - | - | Non |
| Sanandaj 2008 | Arasteh et al. | Female | Of all offenses | High | 208 | - | DSM–IV | 26 | 10.1 | - | - | - | Age, (< 0.003) Gender, (< 0.004) |
| Bushehr 2012 | Soleimani et al. | Female | Of all offenses | Medium | 25 | BDI | DSM–IV | - | 56 | - | - | - | Age, (< 0.05) Child number, (< 0.05) |
| Minab 2012 | Sanaii | Male | Of all offenses | Low | 100 | SCL - 90 - R | DSM–IV | - | 23.18 | - | - | - | Education (< 0.01), Time served in prison (0.03) |
| Tehran 2006 | Emamhadi et al. | Male | Violent (136) | High | 136 | SCL - 90 - R | DSM–IV | - | 31.6 | - | - | - | Non |
| Kashan 2014 | Sepehrmanesh et al. | Male | Non violent (47), Violent (21), Drug (67), Other (124) | High | 180 | SCL - 90 - R | DSM–IV | 36 | 27.6 | 4.3 | - | 13 | Head trauma (< 0.05), Education (< 0.03) |
Features and Characteristics of the Studies Included in the Study
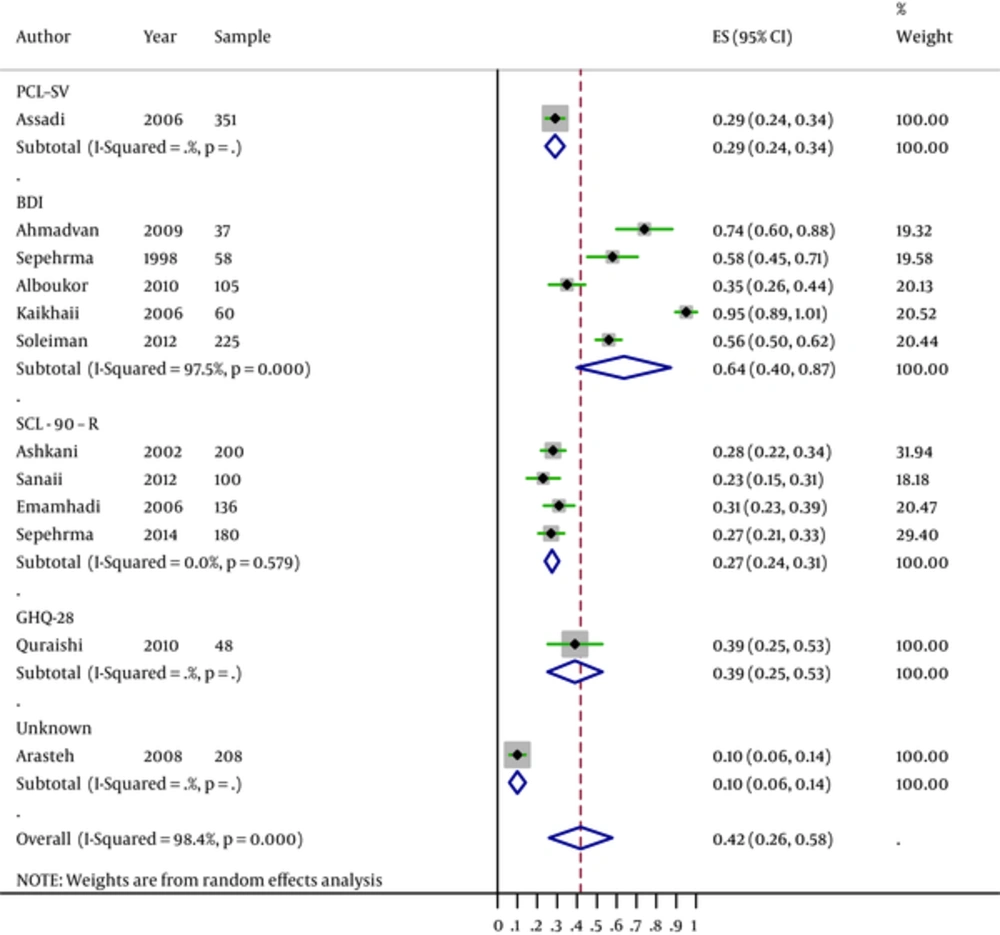
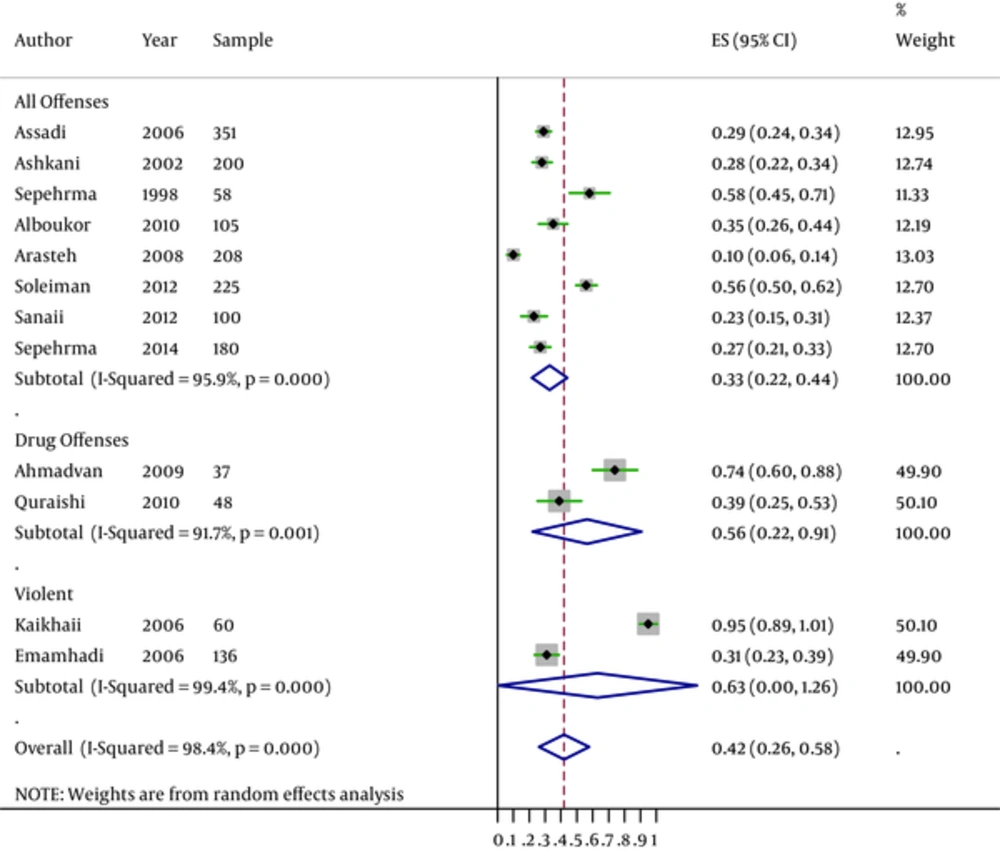
Based on the beck depression inventory (BDI) instrument and symptom checklist-90-Revised (SCL-90-R), the prevalence rates of pooled major depression in prisoners were 64.0% (95% CI: 0.40 - 0.87) and 27.0% (95% CI: 24.0 - 31.0), respectively, which showed a higher rate of major depression in studies with the BDI instrument (Figure 3). The prevalence of major depression in prisoners with all offenses was 33.0% (95% CI: 22.0 - 44.0) and in prisoners with drug and violent offenses were 56.0% (95% CI: 0.22 - 0.91) and 63.0% (95% CI: 0.0 - 1.26), respectively (Figure 4).
3.3. Psychiatric and Personality Disorders
There were 3 studies reported rates of psychotic illnesses. The fixed effect of overall prevalence of psychotic illnesses was 3.5% (95% CI 2.3 - 5.0) in prisoners. Results did not confirm heterogeneity between the studies (heterogeneity statistic = 1.33, P = 0.513). An anxiety disorder had the highest prevalence (56.3%), followed by mood disorders (34.6%). Antisocial personality disorders were diagnosed in 24.0% of the participants, and borderline disorders in 7.1% (Table 2).
| Specific Disorders | Prevalence % (95% CI) | Test(s) of Heterogeneity | ||
|---|---|---|---|---|
| I2 (%) | X2 | |||
| Psychiatric disorders | Psychotic disorder | 3.6 (2.3, 5.0) | 00.0 | 1.33b |
| Mood disorder | 34.6 (30.8, 38.4) | 79.8b | 9.89b | |
| Anxiety disorder | 56.3 (53.7, 59.0) | 99.4b | 39.33b | |
| Personality disorders | Antisocial | 24.0 (20.6, 27.3) | 94.6b | 36.93b |
| Borderline | 7.1 (5.0, 9.1) | 85.7b | 14.02b | |
Prevalence Rates of Specific Disorders and Personality Disorders Among the Samplesa
3.4. Meta-Regression Analysis
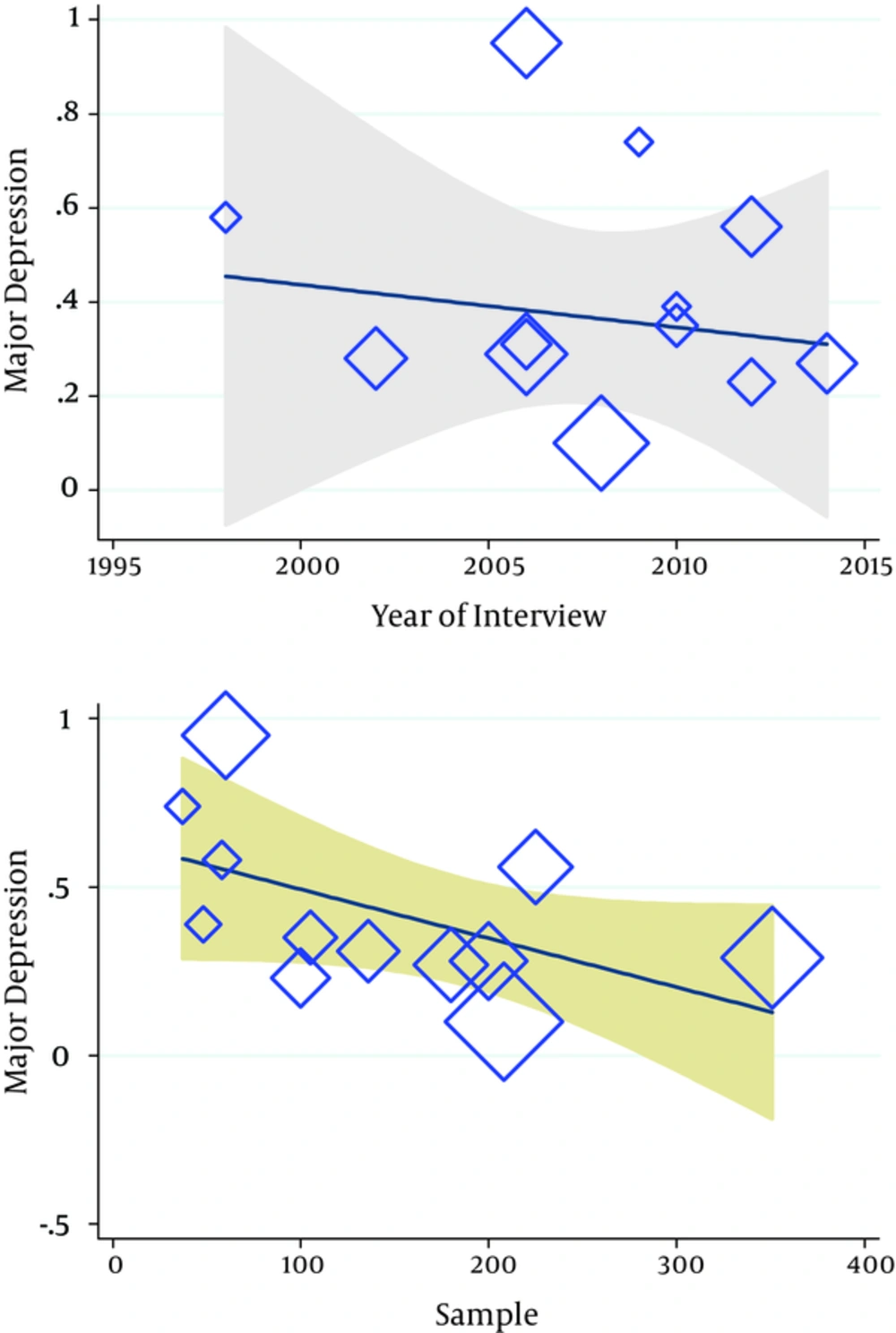
According to the results of the meta-regression analysis (Figure 5), the year of publication and number of subjects had no association with heterogeneity in results. Thus, the year of publication and number of subjects showed no relationship with the causes of variability in the results of a five-year survival rate (Reg Coef = 0.287, P = 0.63 and Reg Coef = 0.291, P = 0.115, respectively). In particular, we found that the rates of major depression in prisoners have been flat over time (P = 0.47).Therefore, the results of meta-regression showed a constant trend from 1995 to 2014 (b = 21.09, s.e. (b) = 33.76, P = 0.54) (Figure 5).
4. Discussion
Our results in this systematic review showed that the prevalence of major depression in prisoners (n = 1708) was observed in 42% of inmates. Previous reports showed that these disorders might be risk factors for suicide (5). Rates of major depression were significantly higher in male than in female prisoners (44% in males versus 33% in females). Consistent with our results, the current reviews have been shown that psychiatric disorders are more prevalent in prisoners than general population (4, 22). Andreoli et al. in Brazil (2014) reported that a 12-month prevalence of any mental disorder was 39.2% among women, and 22.1% among men which was much lower than the percentage in this study (23). Some divergences in studies can be resolved by difference in the methodological approach. A review by Fazel and Danesh found 3.7% and 10% for psychotic illnesses and major depression, respectively in male prisoners (22).
We found a significant heterogeneity among the studies, according to the findings of major depression in both male and female prisoners. The positive heterogeneity among studies somewhat was to be predictable as a result of different methods in different groups across a diversity in study population. In addition, some parts of the observed heterogeneity in the results can be attributed to the number of studies, which included seven studies for males and two studies for females. Asymmetric funnel plots maybe explained by positive heterogeneity in this study. A meta-regression analysis was used to explore heterogeneity among the studies. Results found no variations in the year prevalence of major depression and showed that rates of major depression in prisoners have been flat over time (Figure 5).
Implication in this study was subgroup meta-analyses by gender, offense of prisoners and instrument assessment (Table 2). We found different prevalence rates of psychiatric diagnoses among offence categories. The highest prevalence was observed in prisoners with violent offences (74.0%). This result suggests that prison authorities should be paying more attention to the mental health prisoners with violent offences.
Our results contained a number of implications. First, we did not find increase in the trend of major depression over time; generally, an important explanation was not obvious but some progress steps in screening and care programs of illness, some facilities to better living conditions, and diversion of mentally-disordered offenders from prison to a hospital may have contributed to these findings. Second, we found a higher prevalence of psychiatric morbidity in Iranian prison compared with general population. In current report, the prevalence of psychiatric disorders in the general population in Iran was 17%, which implied that the rate of psychiatric morbidity was approximately triple higher in prisoners (2).
Limitations in this review included the small number of studies involved in the final meta-analysis. Second, we did not find some reasons for a positive heterogeneity in this study because we did not test it, such as comorbidity, due to lacking in primary studies. Lastly, studies that exclusively determined psychotic disorders in women prisoners were limited.
In summary, our results revealed that one-in-three male prisoners and one-in-four female prisoners had depression, and treatment can possibly present extra benefits, such as lowering the risk of suicide and reducing levels of reoffending. Future prisoners’ studies should include studies to increase of knowledge on psychiatric history of prisoners and screening of other potential psychological problems such as suicide attempts, evaluation of treatment that received in prison, besides the relationship between mental illness in prisoners and repeat of the crime rates requires assessment in future studies.