1. Introduction
Schwannomas and neurofibromas are the most common tumors affecting the nerve coverings outside the brain and spinal cord (1). Schwannomas develop from the cells surrounding nerves and can occur at any age (1). They are benign growths with a very low likelihood of becoming malignant (1). In contrast, neurofibromas often present as multiple growths and may quickly transform into a type of cancer called sarcoma (2). Between 25% and 40% of schwannomas are found in the head and neck region (3), but they are rare in the nasal and sinus areas (4). Approximately 4% of schwannomas originate in the nasal region or sinonasal tract (4).
Schwannomas grow slowly, exerting pressure on nearby tissues and causing appearance and sensory issues (5). When a schwannoma is present in the nose, most symptoms arise from tumor pressure on surrounding structures, worsening as the tumor grows (5). Schwannomas at the tip of the nose can reduce skin sensitivity (2). Although generally asymptomatic, these benign growths can sometimes cause epistaxis, nasal pain, or rhinorrhagia. Nasal obstruction and headaches are the most common complaints reported by patients seeking medical attention (6). Computed tomography (CT) and magnetic resonance imaging (MRI) scans are essential for evaluating nerve tumors (5). Additionally, specific stains, such as S-100 protein, calretinin, and CD56, aid in achieving a more accurate diagnosis (7). Various treatment methods, including craniotomy, endoscopic endonasal approach, rhinotomy, and others involving the nose and sinuses, are available for managing these tumors (6).
Schwannomas on the nasal tip are rare. Approximately 20 cases of nasal septal schwannomas have been reported in the literature (7). This paper presents a case of a schwannoma located at the nasal tip, detailing its clinical manifestations, diagnostic process, and treatment approach.
2. Case Presentation
A 14-year-old Iranian girl visited an ear, nose, and throat specialist with a primary complaint of a lump at the tip of her nose that had gradually increased in size. She first noticed the lump two years before this consultation, during which time it caused a noticeable change in the appearance of her nasal tip (Figure 1). She had not sought prior treatment. Her medical history was unremarkable, with no nasal injuries, illnesses, deformities, or congenital abnormalities reported. The patient did not experience any significant symptoms, such as skin discoloration or nasal blockages, apart from mild discomfort, slight pain from the lump, and minimal numbness on the bridge of her nose. She did not report a stuffy nose or additional numbness.
On examination, a lump measuring approximately 26 × 30 mm was palpated at the nasal tip. It consisted of round, movable, soft nodules with a smooth surface covered by normal skin and tissue. There were no signs of ulceration, bleeding, or skin discoloration. While the skin and mucous membrane over the lump were mobile, they adhered to the underlying cartilage. The nasal cavities were symmetrically sized. Sensory impairment was evaluated through two-point discrimination testing with a caliper, showing a range of 17 - 20 mm compared to the normal reference range of 10 - 12 mm (8).
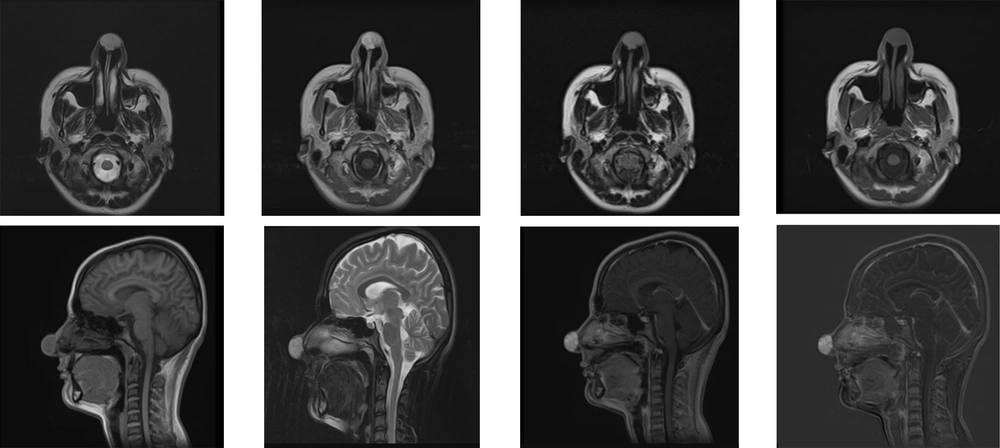
Preoperative ultrasound imaging revealed a mixed solid and fluid-filled mass that had not infiltrated the nasal septum, cartilage, tissue, or bone. Further assessment with MRI provided additional details. Axial images, 3 mm thick, were acquired in various sequences (T1- and T2-weighted) to enhance visualization of internal structures. After administering a contrast agent, additional images were taken. Magnetic resonance imaging results showed a clearly defined, round lump measuring about 24 × 28 mm located beneath the nasal tip skin. The mass appeared bright on T2-weighted images and less intense on T1-weighted images. After contrast administration, the mass became brighter, with a clear border around it. No evidence suggested extension to deeper structures such as the nasal sinuses or intracranial areas. The edges of the mass were smooth and well-defined. No external fistulas were detected. The tumor exhibited bright signals in T2-weighted images, while in T1-weighted images, it appeared similar to muscle tissue with a darker surrounding capsule. Substantial and uniform contrast enhancement was observed (Figure 2).
Due to the large size of the mass, the surgeon opted for an incision using the open rhinoplasty approach, which provided the necessary visibility and access, particularly since the mass was adhered to the soft tissue. Under general anesthesia, a W-shaped incision was made on the columellar skin to expose the area. Upon accessing the nasal structure, the surgeon observed seventeen nodules of varying sizes, ranging from 3 to 14 mm (Figure 3). The mass had developed within the nasal septum, causing a deviation to the left and significantly affecting the lower cartilage on that side. Notably, the typical bump on the nose was absent due to the tumor pressing against it. The surgeons excised the multiple nodules using both sharp and blunt instruments.
No adhesions were detected, allowing the surgeon to proceed with correcting the nasal deviation. To stabilize the nasal spine, bone grafts were harvested from the lower part of the nose and the central bony wall. After removing the growths, the nasal tip was reconstructed by suturing and adding a support graft. The entire mass was successfully excised. The procedure went smoothly, and the patient reported satisfaction with her appearance (Figure 4). Histopathological analysis of the excised tissue, which appeared as a greyish, oval, soft mass measuring approximately 25 × 25 mm, confirmed the diagnosis of a benign schwannoma.
Nine months post-surgery, the patient's nasal appearance remained favorable. During a follow-up visit, two-point discrimination testing around the area of the mass showed improved sensation compared to pre-surgery, though it had not completely normalized. There were no signs of recurrence or other complications.
3. Discussion
A schwannoma was identified in a 14-year-old girl who reported pain and reduced sensation in her nose. Magnetic resonance imaging revealed a well-defined, bright, rounded mass, and the diagnosis was confirmed through tissue analysis. Open rhinoplasty was performed without complications.
Nasal tip schwannoma is an uncommon growth, typically enclosed within a small sac and not strongly adhered to nearby tissues. This condition is rare, with only a few reported cases (5, 9, 10). In a similar instance, a 35-year-old woman had a tumor on her nasal tip and experienced mild pain following open rhinoplasty. She had seven small lumps, ranging from 2 to 16 mm in size. After CT and MRI scans, the diagnosis of schwannoma was confirmed through analysis of tissue characteristics (11). A study of 94 patients with schwannomas in the anterior skull and nasal area found that these growths appeared brighter on T2- and T1-weighted MRI images and darker on others (6). In this case, the mass appeared consistently bright on T2-weighted images and showed a similar brightness to muscle tissue on other MRI settings. It was also surrounded by a thin, darker layer.
When diagnosing a patient with a bulbous nasal tip, several possibilities should be considered, including hematoma, hemangiomas, dermoid cysts, lipomas, tumors, von Recklinghausen disease, chondroma, leiomyoma, leiomyosarcoma, inverted papilloma, granuloma, myxoma, chondrosarcoma, malignant neurilemmoma, neuroblastoma, mucocele, and schwannoma (12). Hemangiomas, for instance, arise from blood vessels and show darker areas on T2-weighted MRI images (13). Schwannomas originate from nerves and resemble muscle tissue on T1-weighted images but appear brighter in certain areas on T2-weighted images (13). Additionally, detailed MRI can reveal unique twisted patterns, suggestive of an inverted papilloma (14). Nasal polyps, characterized by excess tissue growth, appear brighter on T2-weighted images, distinguishing them from tumors (15). In this case, MRI helped confirm the absence of a cartilaginous tumor on the nasal septum, as there was a clear gap between the tumor and the septum. Additionally, it was unlikely that a tumor involved the muscles or skin, as it was not in contact with these nearby structures. Magnetic resonance imaging can reveal two signs specific to neurogenic tumors. The “target sign” appears as a bullseye on T2-weighted images, with a darker center and a bright outer ring, indicating dense fibrous components centrally and softer myxomatous tissue peripherally. The “fascicular sign” shows bundle-like formations in neurogenic tumors, similar to normal nerve bundles (13). Further tests, such as histopathology, may be necessary to differentiate malignant peripheral nerve sheath tumors from myxomas. Although a CT scan was not conducted in this case, it could serve as a useful tool for initial evaluations or when MRI is unavailable.
Radiological tests may not precisely indicate the origin of a neurogenic tumor, but they can aid in distinguishing between schwannoma and neurofibroma. Schwannomas typically present as a single lump, often located in the arms or legs, with a soft texture. In contrast, neurofibromas in individuals with von Recklinghausen’s disease can appear in multiple locations, often originating from a central point and feeling firmer to the touch (16, 17). In our case, the position and texture of the nasal tip mass led us to suspect a schwannoma rather than a manifestation of von Recklinghausen’s disease.
Both neurofibromas and schwannomas appear bright on T2-weighted images. The bright area observed on T2-weighted images in our patient did not provide specific diagnostic information. Two additional considerations in imaging neural tumors are the nerve’s location relative to the mass and the presence of a capsule. In schwannomas, the nerve is typically found on the periphery of the tumor, and around 70% are encapsulated. In contrast, neurofibromas often have the nerve running centrally or may lack a visible nerve entirely, with only about 30% of cases showing a capsule. No affected nerve was identified in our patient, likely due to its small size and peripheral location. The MRI did show a capsule, suggesting a schwannoma diagnosis (6, 11, 15).
Septal schwannomas often resemble polyps but lack distinctive features, making differentiation from other conditions challenging. During diagnosis, doctors may use various imaging techniques such as CT and MRI, occasionally combined with PET scans (18). A biopsy may be required to confirm the diagnosis. Microscopically, schwannomas exhibit two characteristic patterns known as Antoni A and Antoni B. In the Antoni A regions, closely packed spindle cells are arranged in a circular pattern around an acellular center, called Verocay bodies.
In contrast, the Antoni B area has a looser cell arrangement, with various cell types scattered throughout a significant amount of jelly-like matrix (19). Malignant peripheral nerve sheath tumors differ from schwannomas, displaying malignant features like high mitotic activity and diverse cell types. Other sarcomas lack the nerve-like characteristics of schwannomas and are more distinct at the cellular level (20). Hemangiomas, for example, appear as clusters of blood vessels under a microscope, with smaller branches extending outward (21).
Due to microscopic similarities between schwannomas and neurofibromas, differentiating between them can be challenging, especially in small biopsy samples. Schwannomas are encapsulated and exhibit irregularly positioned stiff blood vessels, while neurofibromas lack a capsule and contain traversing nerve fibers (22). Microscopic examination of schwannomas often reveals fluid-filled cystic areas. Magnetic resonance imaging can be useful in ruling out cartilage tumors by showing a clear separation between the tumor and the nasal septum (9). When cell morphology alone is insufficient for diagnosis, immunohistochemical staining can be employed to confirm schwannomas (23).
Research indicates that transnasal procedures are more commonly performed than open surgeries for nasal schwannomas (57.7% vs. 26.7%) (23). Open rhinoplasty, as used in our case, is relatively rare, reported in only 1.4% of cases (23). Treatment decisions are based on the tumor’s size, location, and potential spread to adjacent areas (23). As in our case, individuals with nasal schwannomas who underwent surgical removal did not experience recurrence (24).
5.1. Conclusions
A nasal tip schwannoma is an uncommon condition in the nasal region. While MRI and CT scans aid in the diagnostic process, a definitive diagnosis depends on examining tissue samples and utilizing immunohistochemistry. Patients undergo surgery, either through open approaches or minimally invasive techniques, to address the condition, with most achieving near-complete recovery and minimal risk of recurrence. Considering a range of differential diagnoses, particularly hemangioma, is crucial. Therefore, a thorough review of the patient’s medical history, comprehensive physical examination, and relevant diagnostic tests are essential for ensuring an accurate and timely diagnosis.