1. Background
Episiotomy is a common obstetric procedure performed during normal vaginal delivery (NVD) to facilitate labor and prevent high-degree vaginal tears (1). Its prevalence varies significantly by country, ranging from 9.7% to 100%, with the lowest rate reported in Sweden and the highest in Taiwan, among both primiparous and multiparous women (2, 3).
Although the World Health Organization (WHO) recommends restricting episiotomy to complicated deliveries (4), it is still widely practiced around the world. However, it has been associated with higher perineal pain scores (5-7) and increased blood loss during delivery (8).
When episiotomy is indicated — for instance, in pregnancies with fetal distress, forceps or vacuum-assisted deliveries, premature births, or breech presentations (9) — it is essential to manage the associated pain and bleeding effectively.
Episiotomy is a highly painful intervention, not only at the time of the incision but also in the long term, affecting aspects such as sexual function (10). Therefore, it is crucial to use effective analgesic methods to minimize pain. Lidocaine, a widely used local anesthetic, is commonly administered in medical centers for this purpose.
Moreover, some studies suggest that combining local anesthetics with a vasoconstrictor can prolong the anesthetic effect and reduce bleeding volume (11).
Recent research has explored the use of lidocaine with or without epinephrine in various non-obstetric procedures, such as rigid nasal endoscopy (12), thoracic surgery (13), and dental surgery (14).
2. Objectives
This study was conducted to evaluate the effects of lidocaine alone and lidocaine combined with epinephrine on post-episiotomy pain and bleeding.
3. Methods
This randomized double-blinded clinical trial was conducted in 2018 on 200 pregnant women admitted for NVD at Yas Hospital Complex, Tehran, Iran, with 100 women assigned to the intervention group and 100 to the control group. Inclusion criteria included women older than 15 years with term, primigravid, singleton pregnancies in cephalic presentation and anterior placenta, who were candidates for vaginal delivery and required an episiotomy. Women with a history of heart disease, thyrotoxicosis, hypertension (blood pressure > 130/90), allergy to lidocaine or epinephrine, substance use, receipt of epidural or spinal anesthesia during labor, or with third- or fourth-degree perineal tears were excluded. The study was conducted in accordance with the Helsinki Declaration and approved by the Ethics Committee of Tehran University of Medical Sciences (IR.TUMS.MEDICINE.REC.1396.4134), and it was registered under the IRCT code IRCT20200421047160N1. A convenience sampling method was used. Sample size was calculated based on pain intensity reported in a study by Schinkel et al. (15), comparing women who received local vasoconstrictors (16.8 ± 11.6) versus those receiving lidocaine (12.4 ± 9.7) for episiotomy repair. With 80% power, a 5% type I error, and 10% attrition risk, 208 participants (104 per group) were enrolled. Simple randomization was used to allocate participants (1:1 ratio). In the intervention group, 2 - 3 minutes before episiotomy, 2% lidocaine hydrochloride (Caspian Tamin Pharmaceutical Company, Iran), in the amount of two 5 mg ampoules in 100 cc, was injected along with 1:200,000 epinephrine (Caspian Tamin Pharmaceutical Company, Iran) using a 10 cc syringe. The control group received only lidocaine hydrochloride 2% in the same volume and concentration. In both groups, if the patient reported pain, a half dose of anesthetic was re-injected. Episiotomy repair was performed similarly in both groups using 20/30 sutures. In this double-blind design, both the participants and the researcher evaluating the outcomes were blinded to group allocation. Study outcomes included pain intensity assessed using a Visual Analog Scale (VAS) and bleeding intensity measured by the number of completely blood-soaked gauze pads used during and after episiotomy. Data analysis was performed using SPSS version 24. Continuous variables were described as mean ± standard deviation, and categorical variables as frequency and percentage. Depending on the distribution, either the independent t-test or Mann-Whitney U test was used for comparing quantitative variables. Categorical data were analyzed using the chi-square test or Fisher’s exact test. A P-value < 0.05 was considered statistically significant.
4. Results
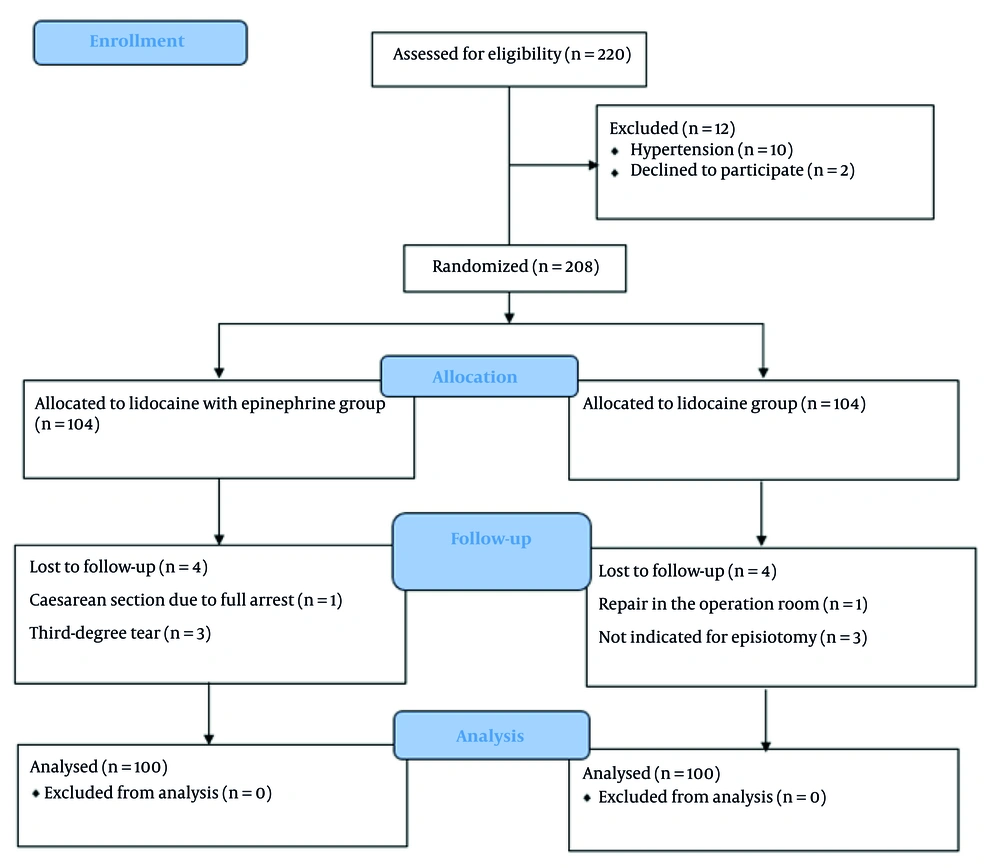
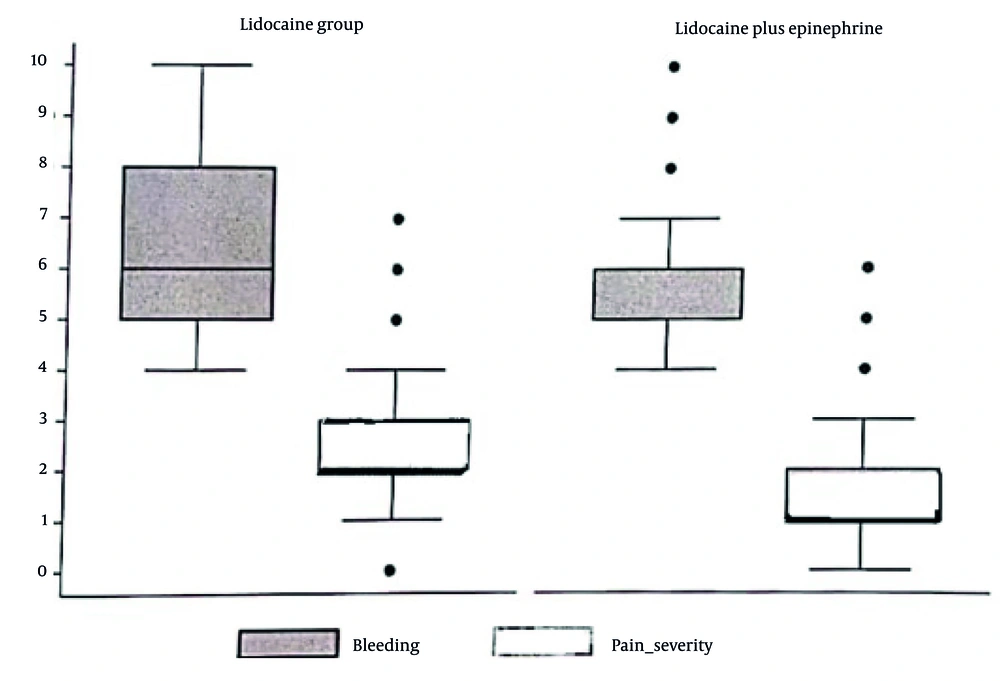
We assessed a total of 220 pregnant women, of whom 12 were excluded from the study (10 due to hypertension and 2 who declined to participate). The remaining 208 women were randomly assigned to either the lidocaine with epinephrine group or the lidocaine-only group. During the study, 8 women (4 from each group) were withdrawn due to cesarean section following full arrest (n = 1), third-degree perineal tear (n = 3), repair in the operating room (n = 1), and cases where episiotomy was ultimately not indicated (n = 3). Therefore, the final analysis was conducted on 200 pregnant women (Figure 1). Baseline characteristics of the two groups were statistically comparable (Table 1). Pain scores were significantly lower in the intervention group compared to the lidocaine group during (1.61 ± 1.49 vs. 1.95 ± 1.63, P = 0.029) and after (1.94 ± 1.04 vs. 2.46 ± 1.46, P = 0.007) episiotomy. Additionally, the number of completely blood-soaked gauze pads was significantly higher in the control group (6.59 ± 1.64 vs. 5.79 ± 1.40, P < 0.001) (Figure 2). Most participants in both groups were able to urinate within 4 hours postpartum, with no statistically significant difference between them (92% in the intervention group vs. 87% in the lidocaine group, P = 0.249). No significant differences were found between the groups regarding other outcomes, including episiotomy length, use of sedative medication, episiotomy repair duration, duration of labor ward stay, breastfeeding initiation time, time to first postpartum urination, or time to ambulation. Potential confounding variables, such as newborn birth weight and participation in prenatal educational classes, were also assessed and found to be statistically similar between the two groups.
| Variable | Lidocaine Group | Lidocaine + Epinephrine Group | P-Value |
|---|---|---|---|
| Age (y) | 26.09 ± 5.33 | 25.04 ± 4.80 | 0.337 |
| Gestational age (d) | 279.56 ± 6.04 | 5.83 ± 280.54 | 0.245 |
| BMI (kg/m2) | 29.99 ± 2.83 | 30.16 ± 2.82 | 0.670 |
| Admission to delivery (h) | 18.70 ± 9.66 | 17.45 ± 10.02 | 0.370 |
| Episiotomy length (cm) | 3.86 ± 0.58 | 3.85 ± 0.62 | 0.907 |
| Episiorrhaphy time (min) | 29.20 ± 6.87 | 30.15 ± 6.41 | 0.313 |
| Receive the second dose of Lidocaine | 2 (2) | 1 (1) | 0.561 |
| Newborn weight (g) | 3358.5 ± 397.51 | 3344.5 ± 459.62 | 0.818 |
5. Discussion
Episiotomy is a common obstetric procedure, with an estimated 35% to 45% of NVD in low- and middle-income countries involving its use (16). Episiotomy typically results in approximately 300 to 600 mL of blood loss (11). In addition to concerns about bleeding, post-episiotomy pain is a frequent complaint among women, with about half reporting pain that persists for up to one week after delivery (10).
Although various pharmacological and non-pharmacological methods for reducing perineal pain — such as far-infrared radiation (17), capacitive-resistive radiofrequency (18), cold application (19), cryotherapy (20), and biofeedback-assisted pelvic floor muscle training (21) — have been evaluated in previous studies, limitations include limited global accessibility and lack of efficacy in reducing bleeding.
Lidocaine is a widely used anesthetic agent for episiotomy (17). However, pain and bleeding during and after episiotomy are not fully managed by lidocaine alone, suggesting the need for complementary agents such as superficial vasoconstrictors to enhance its analgesic effects.
In this study, we evaluated the effect of adding epinephrine to lidocaine in nulliparous women undergoing episiotomy. The results showed that epinephrine significantly reduced post-episiotomy pain severity and bleeding volume.
Due to the favorable impact of epinephrine — which was also confirmed in our study — it is currently recommended by the Ministry of Health. Epinephrine exerts its effect by enhancing the blockade of the pudendal nerve and interfering with the generation and conduction of nerve impulses (17).
Another study conducted on 96 Brazilian women undergoing NVD and requiring perineal repair found that adding a vasoconstrictor (epinephrine) to lidocaine significantly reduced the volume of lidocaine needed to repair first- and second-degree perineal lacerations (15), which aligns with our findings.
Epinephrine exhibits dose-dependent effects. At low doses, it primarily stimulates β1 and β2 receptors, while at higher doses, it acts on α-adrenergic receptors (22). Several studies (22-24) have indicated that using epinephrine can prolong the duration and depth of anesthesia, as well as reduce the required volume of anesthetic agents, thereby minimizing potential side effects.
A clinical trial investigated the use of lidocaine, with or without the local application of lidocaine-prilocaine cream, in reducing pain during episiotomy repair. The results showed that pain intensity was significantly lower in postpartum women receiving both lidocaine and lidocaine-prilocaine during perineal muscle and skin repair, without any reported adverse effects (25).
Episiotomy remains a routine procedure in both developed and developing countries, often leading to prolonged and severe pain that can interfere with postpartum maternal responsibilities. Co-treatment with epinephrine appears to significantly enhance the analgesic effect and duration of lidocaine, while also reducing bleeding associated with episiotomy.
Despite the strengths of this study, certain limitations should be acknowledged, including the relatively small sample size and the single-center design. Future research with larger sample sizes is recommended to assess long-term adverse effects and evaluate the impact of epinephrine on the quality of episiotomy repair.
Although the analgesic effect of lidocaine is well established, our study demonstrated that combining it with epinephrine significantly enhances its efficacy and duration, while also effectively reducing episiotomy-related bleeding.