1. Background
Dacryocystitis is an inflammation of the lacrimal sac, commonly resulting from factors such as nasal fractures, orbital fractures, sinus inflammation, nasal polyps, or cancer (1-3). This condition may present acutely, typically with fever and swelling of the inferomedial orbit, often due to bacterial infections, or chronically, often due to obstruction within the nasolacrimal duct (4). Epiphora, or increased tear production, is another common concern in ophthalmology. While its pathogenesis is multifactorial, it often correlates with increased basal tear flow. Patients may experience exacerbated symptoms under conditions such as exposure to cold or wind. When not attributable to these environmental factors, the excess tearing can often be traced to structural issues like partial obstruction of the nasolacrimal duct or ectropion of the lower eyelid (5, 6). A potential complication of rhinoplasty, which involves surgical manipulation near the nasolacrimal duct and lacrimal sac, is an injury to the nasolacrimal system, manifesting as conditions like dacryocystitis and obstructions of the nasolacrimal meatus (7, 8). Given the proximity of these structures to the surgical site, predicting and mitigating damage to the lacrimal drainage system is feasible and crucial during surgical planning (9). Before this study, there was a paucity of comprehensive research focusing on the occurrence of dacryocystitis and epiphora, specifically following rhinoplasty.
2. Objectives
The objective of this research is to assess these complications post-rhinoplasty and to establish a model that predicts the relationship between rhinoplasty and these complications effectively. By identifying consistent patterns, this study could enable surgeons to implement preventative measures that enhance postoperative outcomes and patient quality of life.
3. Methods
3.1. Study Design and Participants
In this retrospective cohort study, the medical profiles of 165 patients who underwent rhinoplasty at Taleghani Hospital, affiliated with Shahid Beheshti University of Medical Sciences, between 2022 and 2023 were reviewed. A total of 124 patients met the inclusion criteria for the study. Sampling was performed sequentially from patients who visited the hospital. Patients were classified into two groups (with and without complications). Inclusion criteria were adults aged 20 to 40 years, a minimum of 3 months of postoperative follow-up, and access to complete medical records. Exclusion criteria included any prior inflammation or infection of the lacrimal apparatus, history of rhinoplasty, or previous head and neck surgery.
3.2. Data Collection
Once informed consent was obtained and patient confidentiality ensured, we collected demographic and medical data. This included age, sex, and occupational background, as well as medical history regarding the use of immunosuppressive drugs, antibiotics, and existing conditions such as diabetes, dyslipidemia, and hypertension. Each patient underwent rhinoplasty under general anesthesia, and the type of osteotomy performed was documented for further analysis. Post-operative follow-up assessments were conducted at one week, one month, and three months to evaluate the development of dacryocystitis and epiphora. Each case of dacryocystitis or epiphora was clinically diagnosed by an attending ophthalmologist during scheduled follow-up visits.
3.3. Ethical Considerations
The study received approval from the Ethics Committee of Shahid Beheshti University of Medical Sciences (approval code: IR.SBMU.MSP.REC.1401.497). Participants were provided with information about the study's purpose in clear language, and consent was obtained. All procedures adhered to the highest standards of ethical conduct, guaranteeing patient anonymity and the right to withdraw at any time without financial repercussions.
3.4. Sample Size Collection
The appropriate sample size for this study was estimated by an epidemiologist at 81 patients, based on a prevalence estimate of 3.6% for nasolacrimal canal obstruction and epiphora (10), with a margin of error of 3% and an α error of 5%, using G*Power software version 3.1.
3.5. Statistical Analysis
Data analysis was performed using Python and utilized a set of optimized libraries for data manipulation and analysis. The Shapiro-Wilk test was used to assess the normality of the distribution. Descriptive statistics (mean and standard deviation) for continuous variables, and frequency and percentage for categorical variables were calculated. To compare quantitative variables between two groups assuming normality, an independent t-test was used, and if normality was not established, the Mann-Whitney test was used. Variables that showed a significance level of P < 0.15 in the univariate analysis were included in a multiple logistic regression analysis using the forward selection approach.
To explore the associations between post-surgical complications and patient characteristics, logistic regression models were constructed using the scikit-learn library. To estimate the significance of the regression coefficients, a bootstrap method was implemented using the resampling capabilities provided by scikit-learn's `utils` submodule. The bootstrap approach involved resampling the dataset with replacement to create numerous bootstrap samples, fitting a logistic regression model to each sample using scikit-learn, and then aggregating the coefficients obtained from each sample. Confidence intervals for these coefficients were calculated based on their distributions across the bootstrap samples.
4. Results
4.1. Demographics and Baseline Characteristics
The study included 124 patients who underwent rhinoplasty, with an average age of 29.19 ± 5.19 years. Of these participants, 36 (29%) were male and 88 (71%) were female. Detailed analysis of comorbidities and baseline characteristics indicated a higher prevalence of hypertension and mental disorders among different gender groups, which is summarized in Table 1.
| Total Patients | 124 Patients | Dacryocystitis Status | P-Value | |
|---|---|---|---|---|
| Yes (N: 3) | No (121) | |||
| Age (mean ± SD) | 29.19 ± 5.19 | 32.3 ± 2.1 | 29.07 ± 5.1 | 0.084 |
| Gender | 0.001 | |||
| Male | 36 (29) | 0 (0) | 36 (29.8) | |
| Female | 88 (71) | 100 (100) | 85 (70.2) | |
| Hypertension | 10 (8.1) | 1 (33.3) | 9 (7.4) | 0.061 |
| Mental disorders | 8 (6.5) | 1 (33.3) | 7 (5.7) | 0.058 |
| Diabetes | 16 (12.9) | 1 (33.3) | 15 (12.4) | 0.042 |
| Obesity | 26 (21) | 2 (66.6) | 24 (19.8) | 0.001 |
| Autoimmune diseases | 6 (4.8) | 1 (33.3) | 5 (4.1) | 0.024 |
| Allergies | 20 (16.1) | 1 (33.3) | 20 (15.7) | 0.039 |
| Smoking | 42 (33.9) | 3 (100) | 39 (32.2) | 0.001 |
Demographic and Comorbidity Distribution in Patients with and Without Dacryocystitis a
4.2. Incidence and Timing of Complications
Of the 124 patients monitored post-operatively, 3 (2.4%) developed acute dacryocystitis, all of whom were female, diagnosed at the ages of 29, 35, and 33. The onset of symptoms varied, with one case reported within the first week and the remaining within two weeks post-surgery. All instances of dacryocystitis resolved with standard ophthalmological treatment within three months.
4.3. Association Between Comorbidities and Dacryocystitis
Multiple logistic regression analysis showed that obesity (OR = 1.83, 95% CI = 1.05 to 2.62, P = 0.009), female gender (OR = 0.72, 95% CI = 0.54 to 0.91, P = 0.021), smoking (OR = 1.66, 95% CI = 1.1 to 2.11, P = 0.006), and lateral osteotomy (OR = 1.6, 95% CI = 1.09 to 2.09, P = 0.016) were significantly associated with the occurrence of dacryocystitis. Other variables such as diabetes, age, autoimmune diseases, mental disorders, allergies, and transverse, medial oblique, double level, and paramedian osteotomy did not show a significant association. These findings are detailed in Table 2.
| Variables | Coefficient | Odds Ratio | 95% CI | P-Value |
|---|---|---|---|---|
| Diabetes | 0.36 | 1.44 | 0.51, 2.37 | 0.45 |
| Obesity | 0.60 | 1.83 | 0.32, 0.95 | 0.009 a |
| Smoking | 0.50 | 1.66 | 1.1, 2.11 | 0.006 a |
| Age | 0.13 | 1.14 | 0.71, 1.58 | 0.25 |
| Gender (male) | -0.31 | 0.72 | 0.54, 0.91 | 0.021 a |
| Autoimmune | 0.15 | 1.7 | 0.51, 2.62 | 0.36 |
| Mental disorder | 0.32 | 1.3 | 0.6, 2.01 | 0.58 |
| Allergies | 0.37 | 1.4 | 0.51, 2.32 | 0.61 |
| Lateral osteotomy | 0.48 | 1.6 | 1.06, 2.09 | 0.016 a |
| Transverse osteotomy | 0.14 | 1.15 | 0.34, 1.99 | 0.74 |
| Medial oblique osteotomy | -0.04 | 0.95 | 0.15, 1.76 | 0.39 |
| Double level osteotomy | -0.11 | 0.89 | 0.18, 1.61 | 0.44 |
| Paramedian osteotomy | -0.09 | 0.90 | 0.21, 1.82 | 0.75 |
Multivariable Logistic Regression Model of Predictors for Dacryocystitis
4.4. Osteotomy Types and Complication Rates
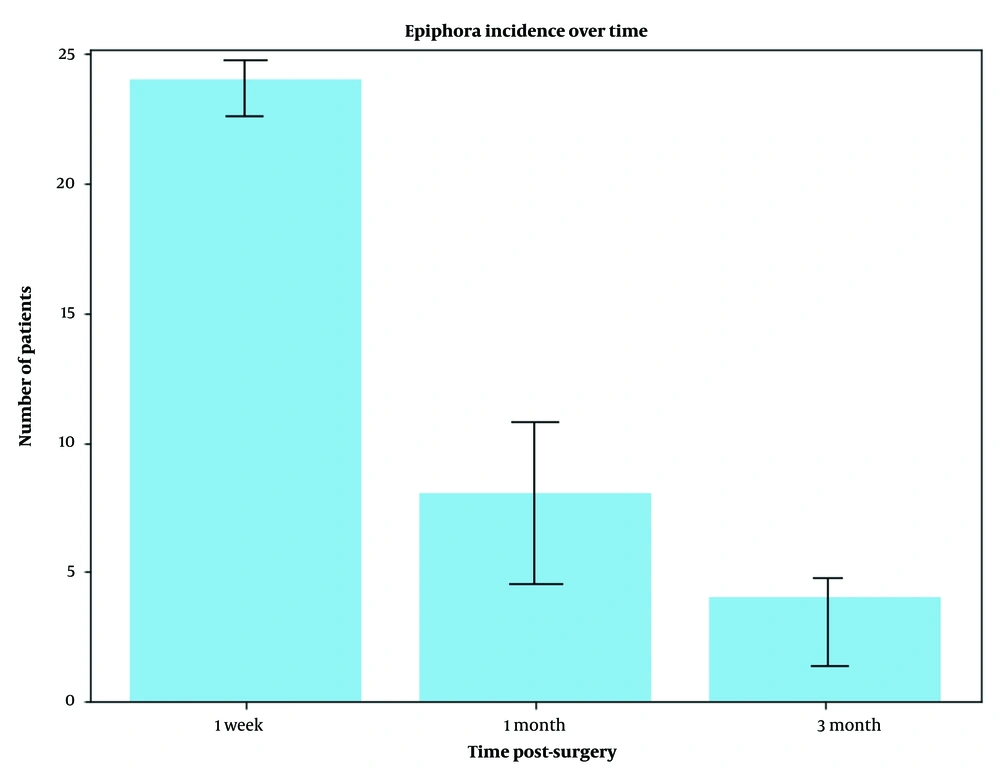
Patients undergoing specific types of osteotomies exhibited different rates of complications. Notably, of the patients who developed dacryocystitis, two had undergone lateral osteotomy, and one had a transverse osteotomy. The incidence of epiphora, initially observed in 24 patients (19.3%), decreased progressively, correlating with the reduction in post-operative inflammation and edema. This trend is depicted in Figure 1.
This bar chart illustrates the number of patients experiencing epiphora post-surgery at one week, one month, and three months, showing a clear trend of decreasing incidence.
4.5. Statistical Analysis of Epiphora Over Time
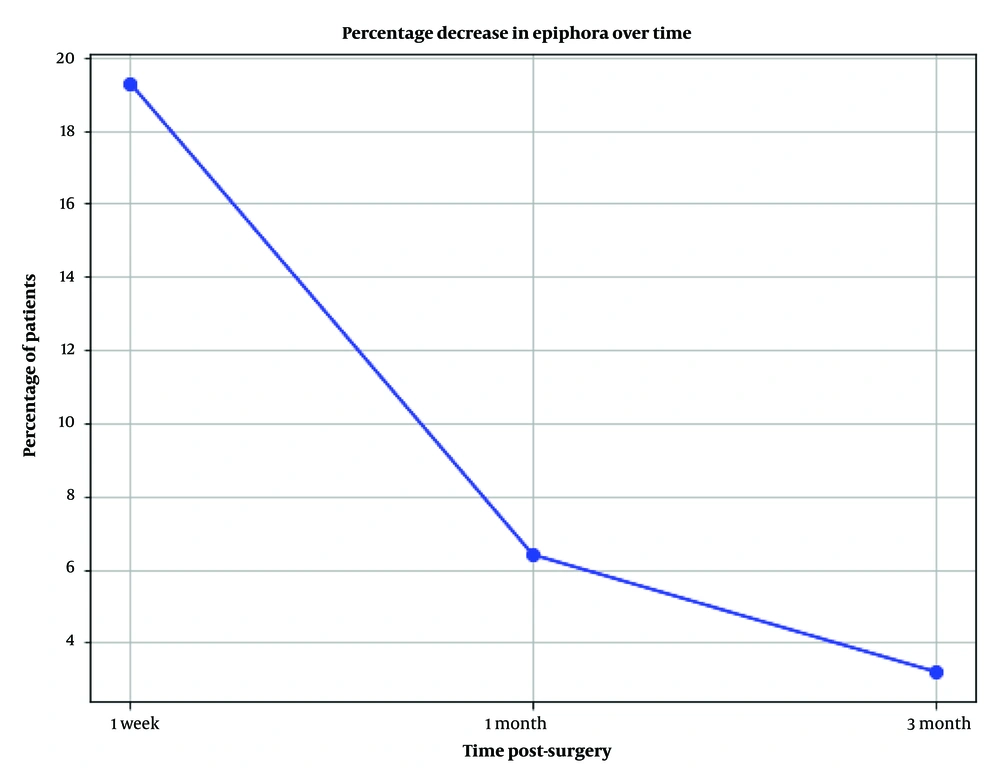
The frequency of epiphora decreased from 19.3% at one week post-operatively to 6.4% at one month, and further to 3.2% by three months, illustrating significant recovery and healing dynamics over time. This pattern is illustrated in Figure 2.
This line graph details the percentage decrease in epiphora from the immediate post-operative period up to three months, highlighting the recovery trajectory.
5. Discussion
This study aimed to explore the incidence and associated risk factors of dacryocystitis and epiphora following rhinoplasty. Notably, the incidence of acute dacryocystitis was found to be low at 2.4%, affecting only female patients. Multiple analyses showed that diabetes, obesity, and smoking were significantly associated with dacryocystitis. Epiphora, which was more frequently observed immediately post-operation, showed a marked decrease over time, demonstrating that while it is a common initial complication, it tends to resolve as the surgical effects subside. This trend highlights the body's capacity to heal post-surgery and may reflect the effectiveness of current post-operative care practices.
The findings regarding the types of osteotomies suggest that specific surgical techniques, such as lateral and transverse osteotomies, may be more likely to result in complications such as dacryocystitis and epiphora. This information could be pivotal for surgical planning, allowing surgeons to weigh the risks associated with each technique more accurately and potentially opt for alternative methods that might reduce the risk of nasolacrimal system complications. To our knowledge, no study has examined the prevalence of dacryocystitis and its predictors after rhinoplasty. All cases of dacryocystitis occurred in women, which could be explained by differences in female characteristics, including potential anatomical/hormonal confounding factors such as narrower nasolacrimal ducts in women.
Chakrabarti et al. (11) investigated the role of inflammation in the occurrence of dacryocystitis. They recommended that inflammation plays a crucial role in the pathogenesis of chronic dacryocystitis. In another study, Edris et al. (12) investigated toll-like receptor signaling, as an important parameter in the initiation of inflammation, in the pathogenesis of dacryocystitis. They also confirmed the role of inflammation in the occurrence of this disorder. In 2014, Harkare et al. investigated the effective factors in the pathogenesis of dacryocystitis. They introduced allergies and exposure to smoke as influencing factors (13). Also, smoking, by increasing oxidative stress, can create favorable conditions for the occurrence of dacryocystitis, but in our study, oxidative stress parameters such as superoxide dismutase, catalase, and glutathione peroxidase were not investigated. Conducting a study that also examines parameters related to oxidative stress in patients will yield more reliable results.
Osteotomy is one of the most critical steps to obtain acceptable results, and it is needed to narrow nasal width. Also, osteotomy is a difficult step in surgery because it is blind and meticulous (14). Based on statistical analysis, a positive correlation was observed between lateral osteotomy and dacryocystitis. The anterior crus of the medial canthal tendon protects the lacrimal sac by passing anteriorly and attaching to the frontal process of the maxilla. The medial canthal tendon splits around the sac on its path to attach to the anterior lacrimal crest of the maxilla and posterior lacrimal crests of the lacrimal bone (15, 16). However, the medial canthal tendon does not fully protect the lacrimal sac and is vulnerable during lateral osteotomy.
Uzun et al. listed that lateral osteotomy, in addition to the unwanted effects on the lacrimal drainage system, can cause medial canthal displacement, periductal inflammation, and medial displacement of puncta (17). Jafaripour and Kashfi (18) reported two patients with damage to the lacrimal system after rhinoplasty. They introduced lateral osteotomy as a predisposing approach for damaging the lacrimal system. They recommended that osteotomies must be performed at least 3 mm from the medial canthus or medial to the line from the alar base to the medial canthus. This principle (3 mm distance) was followed in the present study as well; however, acute dacryocystitis was reported in three patients. This suggests the indirect transmission of infection to the lacrimal sac, as well as the person's susceptibility to inflammation.
Yarmohammadi et al. (19) investigated tear passage time after rhinoplasty. Based on their results, after lateral osteotomy, tear passage time dramatically increased in the first week after rhinoplasty, which could be due to inflammation and edema in the paranasal sinus and pressure over the tearing outlet. In a case series study conducted by Jamshidian Tehrani et al. (20) in 2021, the problems of the lacrimal drainage system after rhinoplasty were investigated. They stated that most of the patients who had epiphora after surgery resolved their problems within 3 months. In our study, most patients reported a decreasing trend in epiphora, which is in line with the results of the above study.
Similar to our study, PA Bezditko and Bezega (21) in 2022 showed that the incidence of dacryocystitis in patients with diabetes was approximately two times higher than in non-diabetic patients. These results were also confirmed in the study by A Ghosal et al. (22). These results may be explained by the role of diabetes in delaying the natural healing process after surgery.
Logistic regression analysis revealed significant associations between various factors and the study conditions. Obesity was one of the most pronounced risk factors; individuals categorized as obese had an odds ratio of 1.83, indicating that they were approximately 1.83 times more likely to develop the condition than non-obese individuals. Smoking also showed a significant positive association with the condition, with an odds ratio of 1.66, suggesting that smoker individuals are 1.66 times more likely to develop the condition than non-smoker individuals. Conversely, male patients exhibited a protective effect with an odds ratio of 0.72, implying that they were 28% less likely to develop the condition compared to females.
These findings highlight the complexity of factors influencing the risk of developing complications after rhinoplasty and underscore the importance of considering a broad range of patient characteristics and surgical details in managing and planning rhinoplasty procedures. The results also emphasize the need for targeted preventive measures to mitigate potential complications in high-risk groups.
5.1. Conclusions
The study confirms that while the overall incidence of dacryocystitis following rhinoplasty is low, it is significantly associated with several modifiable risk factors, such as diabetes, obesity, and smoking. The decreasing trend in epiphora incidence postoperatively suggests the effective management of initial complications and supports the resilience of the surgical recovery process. These insights underline the importance of preoperative assessment and patient counseling regarding lifestyle factors that can mitigate potential risks. Future research should focus on larger multicenter studies to validate these findings and potentially explore the impacts of other unexamined factors. Additionally, the development of standardized protocols for managing patients with high-risk profiles for dacryocystitis and epiphora could significantly improve outcomes following rhinoplasty.
5.2. Limitations
This study had several limitations that warrant consideration. The sample size of 124 patients, while adequate for initial observations, was relatively small to generalize the findings across a broader demographic. Moreover, the study's cross-sectional design limits our ability to establish causality between the observed risk factors and postsurgical complications. Longitudinal studies are necessary to confirm these associations over longer periods and across multiple surgical settings. Due to the study design, we were unable to assess the effect of several key variables, including surgeon experience, on outcomes.
Another limitation is the use of bootstrap methods for statistical analysis. While robust for estimating confidence intervals and suitable for our logistic regression framework, bootstrap methods do not provide traditional P-values, which are often favored in medical research for hypothesis testing. Future studies could integrate traditional statistical methods that provide P-values alongside bootstrap techniques to enhance the comprehensiveness and acceptability of statistical analysis.
There was a possibility of overfitting due to the low event rate. Therefore, designing studies with larger sample sizes in subgroups, considering a number of key variables, including intraoperative imaging (navigation-guided osteotomy), could help to estimate the results more accurately.