1. Background
Spinal tumors are critically important due to their potential to cause significant disability by affecting the spinal cord and nerve roots (1). Primary spinal tumors include those arising from the spinal cord, cauda equina, and spinal meninges (2). These tumors are relatively rare, comprising approximately 3% of all central nervous system (CNS) tumors (3, 4). The rarity of the disease hinders research on the topic and undermines the effective management of patients with primary spinal tumors. The incidence of primary spinal tumors in Iran is approximately 0.48 per 100,000 individuals (5), which is lower than the rates observed in the United States (0.97 per 100,000) and Korea (3.26 per 100,000) (2, 6). This variation can be attributed to several factors, including genetic predispositions, environmental factors, and differences in healthcare access and diagnostic capabilities. Notably, countries with lower income levels tend to report lower incidence rates of spinal tumors (7). This highlights the necessity for region-based epidemiological studies on spinal tumors. Most primary spinal tumors arise in the spinal cord, followed by those in the spinal meninges and the cauda equine (2). These tumors are observed more frequently in women, with non-malignant tumors being more prevalent than malignant ones. Non-malignant tumors are more common among females, while malignant tumors are more frequently found in males. The three most prevalent histopathological types reported are meningioma, tumors of the spinal nerves, and ependymoma (2). The epidemiology of primary spinal tumors is not sufficiently studied in Iran (4, 5).
2. Objectives
The aim of our study was to provide a descriptive epidemiologic report of spinal tumors in Fars, Iran, and compare the results with other studies in Iran and worldwide.
3. Methods
We collected data from the Cancer Registry Center (CRC) of Shiraz University of Medical Sciences. The pathology samples from patients who underwent surgical treatment and biopsies performed at the three major neurosurgery centers (Namazi, Chamran, and Rajae) in Shiraz, as well as other centers across Fars province, are included in this database. The Ethics Committee of Shiraz University of Medical Sciences approved this study (approval code: IR.SUMS.MED.REC.1403.381). According to the last census in 2016, the province of Fars had a population of 4,851,274. We retrospectively selected all patients with primary spinal tumors whose data were registered in the database from 2001 to 2019. Demographic data of patients, including sex and age at the time of surgery, were obtained. We collected pathological information, including the primary tumor site (spinal cord, cauda equina, spinal meninges) and type (extradural, intradural-extramedullary, intramedullary), from the patients’ medical records in the CRC. The first revision of the ICD-O-3 (ICD-O-3.1; 2011) was used to code the tumors based on topography, morphology, and behavior. We initially included all patients with primary spinal tumors, with no age or sex limitations. We excluded all patients with metastatic tumors or non-neoplastic lesions in the pathological results. We also excluded all tumors with primary sites other than the spinal cord, cauda equina, or spinal meninges. In patients with a second surgery, only the first results were considered, and the secondary results were excluded. The Central Brain Tumor Registry of the United States (CBTRUS) classification of primary CNS tumors (8) was used for categorizing primary spinal tumors histology based on ICD-O-3 morphology codes (Table 1). Categorical data were presented as numbers and percentages, and continuous variables were presented as mean and standard deviation (SD). Chi-square and t-test were used to compare categorical and continuous data, respectively. All calculations and statistical analyses were performed using the statistical package for the social sciences (SPSS) version 27. P-values less than .05 were considered statistically significant.
| Primary Spinal Tumor Histologic Categories | ICD-O-3 Codes |
|---|---|
| Tumors of neuroepithelial tissue | |
| Ependymal tumors | 9392, 9383, 9394, 9391, 9393 |
| Astrocytic tumors a | 9400, 9420, 9401, 9440 |
| Embryonal tumors | 9473 |
| Glioma malignant | 9380 |
| Tumors of meninges | |
| Meningioma | 9530, 9539 |
| Mesenchymal tumors | 8857, 8850, 8801, 9150 |
| Other neoplasms related to the meninges | 9220, 9370 |
| Primary melanocytic lesions | 8728 |
| Tumors of cranial and spinal nerves | |
| Nerve sheath tumors | 9560, 9540, 9570 |
| Germ cell tumors and cysts | |
| Germ cell tumors, cysts and heterotopias | 9084 |
| Unclassified tumors | |
| Hemangioma | 9120, 9121 |
| Neoplasm, unspecified | 8004, 8000 |
Histology Categories and ICD-O-3 Codes of Primary Spinal Tumors Based on the Central Brain Tumor Registry of the United States Grouping
4. Results
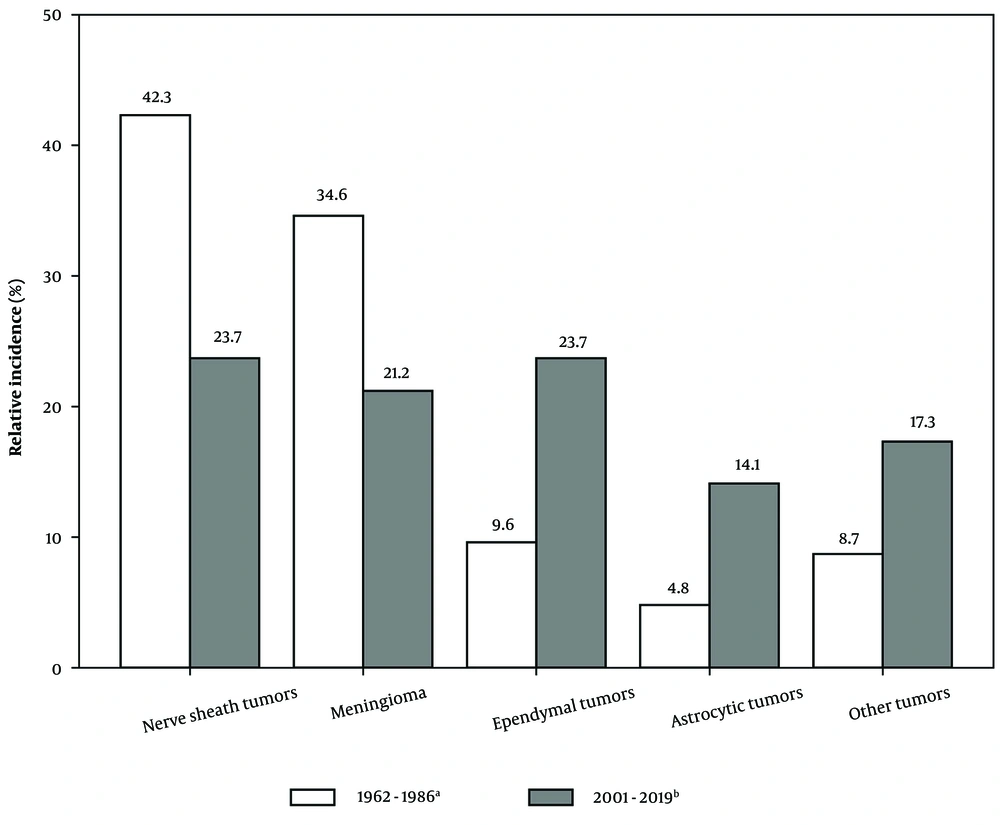
A total of 295 patients were initially included in this study. We excluded 38 patients due to the extra-spinal origin of tumors, 46 patients because their pathology results indicated a non-neoplastic diagnosis, and an additional 45 tumors due to their metastatic origin. Of the remaining 166 patients, 74 (44.6%) were male and 92 (55.4%) were female. The mean age of the patients was 41.9 years (SD, 17.1 years). A total of 111 tumors (66.9%) originated from the spinal cord, while 43 tumors (25.9%) arose from the spinal meninges, and 12 tumors (7.2%) were located in the cauda equina region. Among the pathologic samples, 75 tumors (45.2%) were classified as intradural-extramedullary, 70 tumors (42.2%) were intramedullary, and 21 tumors (12.7%) were extradural. Of the primary tumors, 45.8% were malignant and 54.2% were non-malignant (45.2% benign and 9.0% uncertain whether benign or malignant). The majority of spinal cord tumors were malignant, while non-malignant tumors were more prevalent among tumors of the spinal meninges (P < 0.001). Additionally, most malignant tumors were intramedullary, whereas most non-malignant tumors were intradural-extramedullary (P < 0.001) (Table 2). The most frequent histologic types were ependymal tumors (24.1%), nerve sheath tumors (22.3%), and meningioma (20.5%). The most frequent histologies among the primary malignant tumors were ependymal (38.2%) and astrocytic tumors (32.9%). Most of the tumors with borderline behavior belonged to the ependymal tumors category (73.3%), specifically myxopapillary ependymoma and subependymoma. The most prevalent benign tumors were nerve sheath tumors (48.0%) and meningioma (41.3%) (Table 3). The relative incidence of the four major primary spinal tumors (nerve sheath tumors, meningioma, ependymal tumors, astrocytic tumors) is compared side by side with data from 1962 to 1986 in Figure 1 (9).
| Characteristics | Primary Malignant | Primary Non-malignant | All Tumors | Primary Malignant vs. Non-malignant |
|---|---|---|---|---|
| Total | 76 | 90 | 166 | |
| Gender | 0.055 | |||
| Female | 36 (47.4) | 56 (62.2) | 92 (55.4) | |
| Male | 40 (52.6) | 34 (37.8) | 74 (44.6) | |
| Primary site | < 0.001 | |||
| Spinal cord | 67 (88.2) | 44 (48.9) | 111 (66.9) | |
| Spinal meninges | 4 (5.3) | 39 (43.3) | 43 (25.9) | |
| Cauda equina | 5 (6.6) | 7 (7.8) | 12 (7.2) | |
| Tumor type | < 0.001 | |||
| Extradural | 11 (14.5) | 10 (11.1) | 21 (12.7) | |
| Intradural-extramedullary | 4 (5.3) | 71 (78.9) | 75 (45.2) | |
| Intramedullary | 61 (80.3) | 9 (10) | 70 (42.2) | |
| Age at diagnosis | 0.073 | |||
| 0 - 19 | 12 (15.8) | 4 (4.4) | 16 (9.6) | |
| 20 - 39 | 23 (30.3) | 35 (38.9) | 58 (34.9) | |
| 40 - 59 | 31 (40.8) | 35 (38.9) | 66 (39.8) | |
| +60 | 10 (13.2) | 16 (17.8) | 26 (15.7) | |
| Mean age | 39.3 ± 17.4 | 44.2 ± 16.6 | 41.9 ± 17.1 | 0.992 |
Description of Primary Spinal Tumors by Sex, Primary Site, Tumor Type and Age at Diagnosis a
| Histology | Female | Male | Total | Mean Age |
|---|---|---|---|---|
| Tumors of neuroepithelial tissue | 32 (34.8) | 43 (58.1) | 75 (45.2) | 37.0 ± 16.6 |
| Ependymal tumors | 17 (18.5) | 23 (31.1) | 40 (24.1) | 39.2 ± 14.6 |
| Astrocytic tumors | 10 (10.9) | 15 (20.3) | 25 (15.1) | 36.5 ± 19.5 |
| Embryonal tumors | 4 (4.3) | 4 (5.4) | 8 (4.8) | 28.9 ± 16.8 |
| Glioma malignant, NOS | 1 (1.1) | 1 (1.4) | 2 (1.2) | 30.5 ± 13.4 |
| Tumors of meninges | 34 (37) | 9 (12.2) | 43 (25.9) | 52.0 ± 16.1 |
| Meningioma | 30 (32.6) | 4 (5.4) | 34 (20.5) | 52.8 ± 17.3 |
| Mesenchymal tumors | 3 (3.3) | 2 (2.7) | 5 (3.0) | 53.4 ± 12.0 |
| Primary melanocytic lesions | - | 1 (1.4) | 1 (0.6) | 48.0 ± 0.0 |
| Other neoplasms related to the meninges | 1 (1.1) | 2 (2.7) | 3 (1.8) | 42.3 ± 8.5 |
| Tumors of spinal nerves | 21 (22.8) | 16 (21.6) | 37 (22.3) | 38.1 ± 13.5 |
| Nerve sheath tumors | 21 (22.8) | 16 (21.6) | 37 (22.3) | 38.1 ± 13.5 |
| Germ cell tumors and cysts | 1 (1.1) | - | 1 (0.6) | 23.0 ± 0.0 |
| Germ cell tumors, cysts and heterotopias | 1 (1.1) | - | 1 (0.6) | 23.0 ± 0.0 |
| Unclassified tumors | 4 (4.3) | 6 (8.1) | 10 (6.0) | 52.0 ± 15.6 |
| Hemangioma | 2 (2.2) | 1 (1.4) | 3 (1.8) | 39.3 ± 22.0 |
| Neoplasm, unspecified | 2 (2.2) | 5 (6.8) | 7 (4.2) | 57.4 ± 9.4 |
Number of Primary Spinal Tumors by Major Histology Groupings a
Relative incidence of primary spinal tumors during 1962 - 1986 and 2001 - 2019. a, only primary spinal tumors are included (104 tumors). b, patients younger than 15 years were excluded to match with the data from Ardehali’s study (156 tumors) (9).
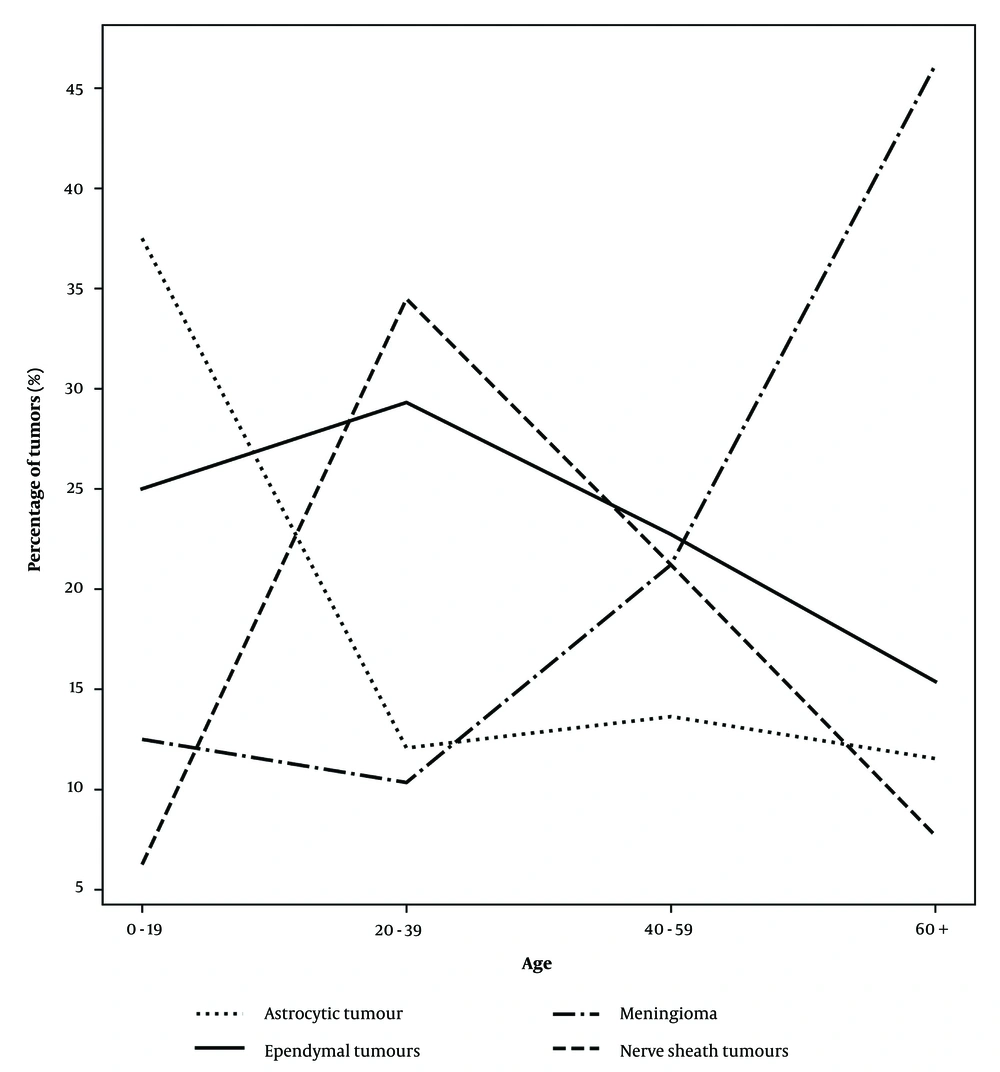
The prevalence of the male sex was higher in malignant tumors (52.6% vs. 47.4%), while the prevalence of women was higher in non-malignant tumors (62.2% vs. 37.8%; P = .055), but this difference did not reach statistical significance (Table 2). In women, meningioma was the most prevalent tumor type (32.6%), while ependymal tumors had the highest prevalence in men (31.1%) (Table 3). The mean age of patients did not show a significant difference between malignant and non-malignant primary tumors [39.3 years (SD, 17.4 years) vs. 44.2 years (SD, 16.6 years); P = 0.992)]. The frequency of spinal tumors was lowest among subjects under 20 years old and peaked in individuals aged 40 to 59 years. Non-malignant tumors were most common in patients aged 20 to 39 years, whereas malignant tumors peaked in the same age group and remained stable among those aged 20 to 59 years before declining in patients over 60 years old (Table 2). In patients under 20 years of age, astrocytic tumors were the most common histological type, while nerve sheath tumors and meningioma were the most prevalent in patients aged 20 to 39 years and those over 60 years old, respectively. Meningioma, nerve sheath tumors, and ependymal tumors were equally distributed in patients aged 40 to 59 years (Figure 2).
5. Discussion
The incidence of CNS tumors has increased globally in recent years (10, 11). A similar trend is observed in Iran on a national scale and in Fars province (4, 12, 13). Spinal tumors form a small portion of all CNS tumors. The percentage of spinal cord tumors reported in Iran varies between 3.14% and 7.1% (4, 5), while those of the spinal cord form 3.1% of all CNS tumors in the United States (3). The majority of primary spine tumors are non-malignant (2, 6). In our study, 45.5% of tumors were malignant, comparable to other studies performed in Iran, which reported 43.75% malignant tumors, but higher compared to other studies in Asia (23.4%) and the United States (22.45%) (2, 6). In this study, the most common histology types found among primary spinal tumors were ependymoma (22.7%), nerve sheath tumors (21.6%), and meningioma (19.3%). However, in another study conducted in Guilan province in Iran, schwannoma (30.1%) was the most frequent finding, followed by meningioma (20.6%) and ependymomas (9.6%) (14). Moreover, a study conducted on data from the national cancer registry of Iran reported neurofibroma (30.7%) as the most prevalent spinal tumor, with meningioma (25.7%) and ependymoma (10.1%) coming next (5). Meanwhile, studies in the United States and Croatia reported meningiomas as the most frequent tumor type, followed by those of the spinal nerves and ependymomas (2, 15, 16). When comparing the results to data from the same region between 1962 and 1986 (9), we observed an increase in the relative incidence of ependymal and astrocytic tumors (Figure 1). This finding, along with the higher prevalence of astrocytic tumors noted in comparison to other regions (2, 15, 16), suggests a potential rise in the prevalence of these tumors in the Fars region over time. However, it is important to note that this data does not definitively indicate an increase in the incidence rate of these tumors, as this study only evaluates the relative incidence among surgically treated patients and does not assess population-based incidence rates. Given the significance of this issue, further studies are warranted to confirm this trend and explore its underlying etiology.
Regarding sex-based differences, the percentage of women with primary spinal tumors was higher compared to men. While malignant tumors were almost equally distributed between sexes, the proportion of female patients was higher in non-malignant tumors. These observations align with other reports from the United States and Korea (2, 6). Meningioma was the most common histological type of primary tumor observed among women, and ependymal tumors were the most frequent tumor among men, consistent with previous observations (2). The frequency of primary spine tumors was lowest in patients under 20 years old and highest in patients aged 40 to 60 years. Similarly, the majority of primary spine tumors were observed in middle-aged patients in Korea and the United States (2, 6). Astrocytic tumors were the most frequent histologic type in young patients, while meningioma was the dominant tumor in patients over 60 years.
Our study has several limitations. First, the database only included spinal tumors confirmed through pathological samples; therefore, it was not possible to reliably calculate the incidence rate of all spinal tumors. Future studies that include all diagnosed spinal tumors will help address these biases and provide a clearer understanding of spinal tumor epidemiology. Second, we did not evaluate metastatic tumors or tumors of the vertebrae, as the data, primarily collected from tertiary referral centers, may not fully represent these cases. More comprehensive studies are needed to establish population-based incidence rates of all spine tumors in Iran. Lastly, our study population was limited to Fars province; therefore, additional research on spinal tumor epidemiology at the national level is recommended.
5.1. Conclusions
This study presents the epidemiology of primary spinal tumors in Fars province, offering a detailed analysis of age and sex differences as well as the distribution of histological types of spinal tumors. We observed a higher prevalence of ependymal and astrocytic tumors compared to other regions and earlier studies conducted in this area. Further research is necessary to confirm these findings and explore their underlying etiology.