1. Background
Fluid management during surgical procedures is critical for optimizing patient outcomes, particularly in spine surgery, where the risk of significant intraoperative blood loss is a substantial concern. Goal-directed fluid therapy (GDFT) has emerged as a tailored approach that uses real-time physiological data to guide fluid administration. By closely monitoring hemodynamic parameters, GDFT aims to maintain optimal intravascular volume and prevent complications associated with both under-resuscitation and fluid overload (1).
In traditional practice, fluid therapy often follows a one-size-fits-all approach, which can result in variable outcomes related to blood loss and transfusion rates. The GDFT, however, utilizes dynamic parameters such as stroke volume variation (SVV) to individualize fluid administration, thereby enhancing hemodynamic stability during surgery. This evidence-based strategy has demonstrated the potential to reduce intraoperative blood loss and, consequently, the need for blood transfusions in patients undergoing spine surgery (2).
Studies have shown that GDFT can significantly decrease the volume of fluids administered, thereby reducing the likelihood of transfusions (3). For instance, one study indicated that patients receiving GDFT required fewer units of packed red blood cells (RBCs) during major spine surgeries compared to those managed with standard fluid protocols (4). This reduction in transfusion rates not only minimizes the risks associated with transfusion-related complications but also improves overall patient safety (5).
Moreover, GDFT contributes to better management of intraoperative hemodynamics, promoting enhanced tissue perfusion and oxygenation. By ensuring that fluid resuscitation is aligned with real-time physiological needs, GDFT helps mitigate complications arising from significant blood loss, such as organ dysfunction (6). During surgery, bleeding can lead to a decrease in cardiac output (7). Spine surgery, in particular, may result in a 25% reduction in cardiac output due to the change from a supine to a prone position. The prone position increases intra-abdominal pressure (IAP), which in turn compresses the inferior vena cava and exacerbates bleeding (7, 8). Hemodynamic management during surgery must balance the goal of minimizing bleeding with the necessity of maintaining adequate spinal perfusion (9). The application of GDFT in spinal surgery can enhance the precision of intraoperative fluid volume management and restore hemodynamic stability, thus improving postoperative recovery. The physiological benefits of this approach underscore its significance in spine surgeries, where maintaining hemodynamic stability is essential for successful outcomes.
Metabolic acidosis following blood transfusion can be caused by several factors related to the storage and administration of blood products. One major contributor is the accumulation of citrate, an anticoagulant used during blood storage. Additionally, the bicarbonate content of stored blood decreases over time, impairing its buffering capacity and promoting a base deficit. As RBCs age, potassium and hydrogen ions leak from the cells into the plasma, increasing hydrogen ion concentration and worsening metabolic acidosis. Furthermore, large volumes of blood transfusion can result in dilutional acidosis, where excessive administration of normal saline or crystalloids dilutes plasma bicarbonate and leads to hyperchloremic metabolic acidosis. Finally, impaired renal function — whether pre-existing or induced by shock — can limit the body’s ability to excrete excess acids, thereby further aggravating acidosis (10).
The economic implications of reducing transfusion rates are also noteworthy. Fewer blood transfusions can lead to decreased hospital costs associated with blood products and shorter lengths of stay, providing a compelling argument for adopting GDFT in surgical practice (11). As healthcare systems increasingly focus on cost-effectiveness, the integration of GDFT represents a dual benefit of improving patient outcomes while optimizing resource utilization.
There are limited studies that examine the impact of GDFT on patients’ clinical conditions following extensive surgeries in the prone position, such as disc herniation.
2. Objectives
The present study investigated whether a specific approach to administering fluids during surgery (targeted fluid therapy) could reduce the need for blood transfusions in spinal surgeries.
3. Methods
This study was a double-blind clinical trial involving patients undergoing intervertebral disc herniation surgery (one or two levels) at Golestan Hospital, Ahvaz, Iran, from 2020 to 2022. Sixty patients participated after obtaining approval from the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (ethical code: IR.AJUMS.REC.1399.250; trial code: IRCT20201014049024N1). Informed consent was obtained from all patients after explaining the goals of the study to them.
3.1. Randomization and Blindness
After identifying eligible participants, patients were randomized into two groups of 30 each using a computer-generated randomization chart and identical opaque envelopes for allocation concealment. Patients received either GDFT or the conventional fluid therapy method as the control group. Patients, the surgeon, and outcome assessors were blinded to the type of fluid therapy administered. All surgeries were performed by the same surgeon. Due to the nature of the intervention, the anesthesiologist administering the fluids was not blinded; however, standardized protocols were followed to minimize potential bias. Inclusion criteria included individuals aged 18 - 70 years, candidates for elective intervertebral disc herniation surgery with a duration of less than 4 hours, and classified as ASA I or II. Exclusion criteria involved patients with cardiac, pulmonary, kidney, or liver diseases, those taking oral anticoagulants, and any who expressed dissatisfaction with participation.
3.2. Sample Size
The sample size was calculated based on transfusion volume (the primary outcome), using data from the spine surgery study by Bacchin et al. (7):
The GDFT group: 350.15 ± 110.15 mL (mean ± SD)
Control group: 370.15 ± 115.20 mL (mean ± SD)
Using α = 0.05, β = 0.20, power = 80%, and targeting a 20% reduction in transfusion volume (Δ = 84.36 mL), the required sample size was 28 patients per group. To account for potential dropouts, 30 patients were recruited per group (a 15% increase).
All patients underwent surgery under identical conditions. After establishing a secure IV line, patients were transferred to the operating room, where 5 mL/kg of Ringer’s solution was administered. During surgery, all patients received standard monitoring, including electrocardiography (ECG) to track heart activity, pulse oximetry to measure blood oxygen levels, and non-invasive blood pressure monitoring. Additionally, a Bispectral Index (BIS) was used to monitor the level of consciousness. Anesthesia was administered by an anesthesiologist using the same medication regimen for all patients: Midazolam 0.05 mg/kg (Tehran Shimi, Iran), propofol 2 mg/kg (Diprivan, ICI Pharmaceuticals, Macclesfield, UK), fentanyl 2 mcg/kg (Aburaihan Co., Iran), and cisatracurium 0.2 mg/kg (Alborz Darou, Iran). After tracheal intubation, a capnogram was applied to monitor end-tidal CO2 (ETCO2), which was maintained between 30 and 35 mmHg. In addition to non-invasive monitoring, an invasive radial arterial line was placed for blood pressure monitoring and blood gas management. A urinary catheter was inserted to monitor urine output. Body temperature was measured every 20 minutes using a tympanic thermometer probe. Forced-air warming blankets were used throughout the procedure to maintain a normal body temperature (between 36.5°C and 37°C). Anesthesia was maintained with a mixture of oxygen (50%) and nitrous oxide (N2O). Isoflurane was used to control the depth of anesthesia, adjusted to maintain a BIS value between 40 and 60. Pain relief was provided with fentanyl (1.5 µg/kg/h), and muscle relaxation was achieved with atracurium (1 mg/kg/h). Mechanical ventilation was set with a tidal volume of 8 to 10 mL/kg and a fresh gas flow rate of 4 L/min. After changing the patient to the prone position, intravenous morphine 0.1 mg/kg was administered.
After the onset of surgery, hematocrit (HCT) and arterial blood gas (ABG) analyses were performed every 60 minutes for all patients. The target HCT was 27%, and if it dropped below this threshold, one unit of packed RBCs was transfused. In cases of acidosis (pH < 7.28) detected in the ABG sample, correction was performed using bicarbonate, calculated based on the following formula:
HCO3- deficit = (Desired serum HCO3- - Measured HCO3-) × 0.5 × Body weight (volume of distribution for HCO3-) (12).
After induction of anesthesia, 10 mg/kg of tranexamic acid was administered intravenously.
3.3. Intervention
The control group received fluids based on a standard calculation that considered several factors, including fasting deficit, evaporative loss, maintenance fluids, urine output, and blood loss. Crystalloid fluids were administered according to the 1 - 2 - 4 mL/kg rule for NPO hours, and an additional 10 cc/kg was infused during the fluid replacement period.
Additional fluids were administered based on the patient’s blood pressure. If the mean arterial pressure (MAP) dropped below 20% of baseline, fluids were given in stages: First, 10 mL/kg of crystalloid solution. If blood pressure remained low, an additional 10 mL/kg of crystalloid solution. If hypotension persisted after fluid administration, 10 mg of ephedrine was injected to raise blood pressure.
The GDFT group received fluids based on a specific protocol designed to optimize blood flow (13). The SVV, a measure of blood flow fluctuation, was continuously monitored throughout surgery using a specialized device (FloTrac/Vigileo, Edwards Life Sciences, Irvine, CA). While SVV has known limitations in the prone position (9), we maintained consistent patient positioning and utilized FloTrac’s proprietary algorithms to mitigate these limitations.
Here’s how they managed fluids and blood pressure:
The goal was to maintain SVV below 13% and MAP above 65 mmHg: If SVV increased above 12%, a crystalloid fluid bolus was administered to reduce it. If MAP dropped below 65 mmHg and SVV remained within acceptable limits, ephedrine 10 mg was administered to raise blood pressure.
Blood loss replacement: Three mL of saline solution was given for every 1 mL of blood lost.
The RBC transfusion: If HCT dropped below 27%, or hemoglobin fell below 9 g/dL, both groups received a blood transfusion.
Acidosis correction: If blood gas analysis revealed metabolic acidosis, bicarbonate was administered using the following formula:
HCO3- deficit = (Desired serum HCO3- - Measured HCO3-) × 0.5 × Body weight (volume of distribution for HCO3-) (12).
3.4. Outcomes
The primary outcome was transfusion requirement. Secondary outcomes included the volume of intravenous fluid administered, the amount of ephedrine used, volume of bleeding, incidence of acidosis, and urinary output.
3.5. Statistics
Statistical analysis was performed using SPSS version 22.0. Measurement data were presented as mean ± standard deviation, and comparisons between groups were made using the independent t-test. Categorical data were presented as frequency and percentage, and comparisons were performed using either the χ2 test or Fisher’s exact test. A P-value < 0.05 was considered statistically significant.
4. Results
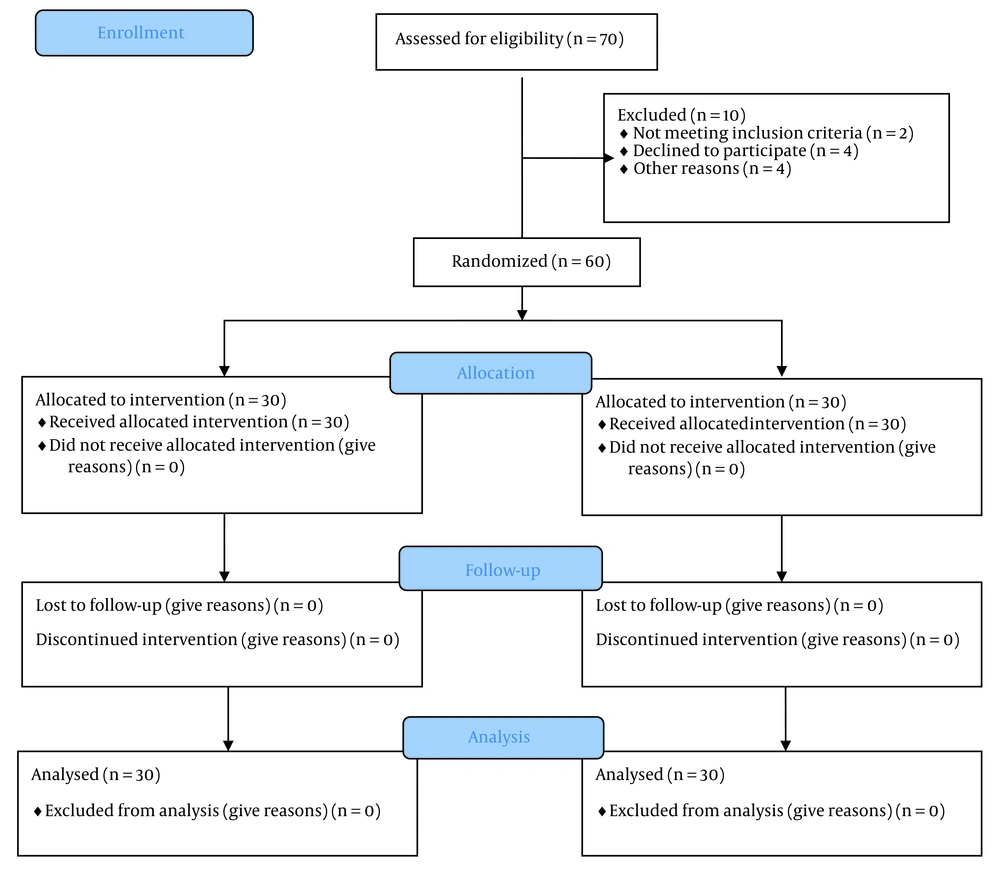
This study investigated whether a specific fluid management strategy called GDFT could reduce the need for blood transfusions during spine surgery. It was conducted as a randomized, double-blind clinical trial. Sixty patients (30 in each group), aged 18 - 70 years, were hospitalized at Golestan Hospital, Ahvaz, Iran (2020 - 2022). A CONSORT flow diagram illustrates the enrollment process: Seventy patients were screened, 10 were excluded (2 ineligible, 4 declined to participate, and 4 for other reasons), and 60 were randomized (30 per group) (Figure 1).
Patients were analyzed in two groups: The GDFT group and the control group. The researchers observed sex distribution and age among participants. There were more males in the control group (70%) compared to the GDFT group (56.6%). The average age was similar between the groups — 44.1 years in the control group versus 45.5 years in the GDFT group (Table 1).
| Variables | GDFT Group | Control Group | P-Value b |
|---|---|---|---|
| Age (y) | 45.53 ± 10.801 | 44.10 ± 8.066 | 0.084 |
| Sex (male/female) | 17 (56.6)/13 (43.3) | 21 (70)/9 (30) | 0.284 |
Abbreviation: GDFT, goal-directed fluid therapy.
a Values are expressed as No. (%) or mean ± SD.
b P-value < 0.05 is considered statistically significant.
More importantly, the study investigated blood transfusion rates. Approximately 26.6% of patients in the GDFT group received a transfusion, compared to 30% in the control group. The volume of transfused blood was also similar between the two groups: 350.15 ± 110.15 mL in the GDFT group versus 370.15 ± 115.20 mL in the control group. The mean difference was -20.0 mL (95% CI: -96.4 to 136.4, Cohen’s d = 0.18, P = 0.796).
The amount of bleeding was 361.67 ± 112.71 mL in the GDFT group versus 386.67 ± 143.20 mL in the control group (mean difference: -25.00 mL, 95% CI: -89.34 to 39.34; Cohen’s d = 0.20, P = 0.587).
The required ephedrine dose was 14.40 ± 1.02 mg in the GDFT group compared to 12.80 ± 0.93 mg in the control group (mean difference: 1.60 mg, 95% CI: -1.23 to 4.43; Cohen’s d = 0.35, P = 0.428).
Fluid input was significantly lower in the GDFT group (3583.33 ± 373.32 mL) than in the control group (4090.00 ± 628.27 mL), with a mean difference of -506.67 mL (95% CI: -782.45 to -230.89; Cohen’s d = 1.02, P = 0.01).
Urine output was higher in the GDFT group (661.67 ± 224.64 mL) than in the control group (515.00 ± 172.78 mL), showing a mean difference of 146.67 mL (95% CI: 8.34 to 285.00; Cohen’s d = 0.65, P = 0.048).
Acidosis occurred in 9 patients (30%) in the GDFT group and in 7 patients (23.3%) in the control group (risk difference: 6.7%, 95% CI: -12.3% to 25.7%; odds ratio: 1.40, 95% CI: 0.45 to 4.34, P = 0.774) (Table 2).
| Variables | GDFT Group | Control Group | Mean/Risk Difference (95% CI) b | Effect Size c | P-Value d |
|---|---|---|---|---|---|
| Fluid input (cc) | 3583.33 ± 373.320 | 4090.00 ± 628.271 | -506.67 (-782.45 to -230.89) | Cohen’s d = 1.02 | 0.01 |
| Transfusion volume (cc) | 350.15 ± 110.15 | 370.15 ± 115.20 | -20.00 (-96.40 to 136.40) | Cohen’s d = 0.18 | 0.796 |
| Bleeding (cc) | 361.67 ± 112.712 | 386.67 ± 143.198 | -25.00 (-89.34 to 39.34) | Cohen’s d = 0.20 | 0.587 |
| Acidosis | 9 (30) | 7 (23.3) | RD: 6.7 (-12.3 to 25.7) | OR: 1.40 (0.45 - 4.34) | 0.774 |
| Urinary output (cc) | 661.67 ± 224.639 | 515.00 ± 172.782 | 146.67 (8.34 to 285.00) | Cohen’s d = 0.65 | 0.048 |
| MAP (mm Hg) | 90.26 (8.56) | 91.62 (4.75) | -1.36 (-4.32 to 1.60) | Cohen’s d = 0.19 | 0.821 |
| Vasopressor use (mg) | 14.40 ± 1.023 | 12.80 ± 0.925 | 1.60 (-1.23 to 4.43) | Cohen’s d = 0.35 | 0.428 |
Abbreviations: GDFT, goal-directed fluid therapy; RD, risk difference; OR, odds ratio (for binary outcomes); MAP, mean arterial pressure.
a Values are expressed as No. (%) or mean ± SD.
b Confidence intervals are 95%.
c Effect sizes interpreted as: Cohen’s d: 0.2 = small, 0.5 = medium, and 0.8 = large.
d P-value < 0.05 is considered statistically significant.
5. Discussion
This survey aimed to study the influence of GDFT on the amount of transfusion during spine surgery. Our findings showed that there was no significant difference between the two groups regarding the amount of bleeding during surgery, the amount of transfusion, and the incidence of acidosis. The amount of urinary output and the requirement for ephedrine administration, although higher in the GDFT group, did not indicate any significant difference. Conversely, the amount of input fluids among patients in the GDFT group was less than that of the control group, which is justifiable considering the targeted phase of fluid therapy during surgery in the targeted group. However, there was no significant difference concerning the amount of input fluids between the two groups. Maintaining an adequate amount of circulating blood and tissue perfusion during surgery is essential. Insufficient vascular volume and failure to replace fluid loss during surgery can lead to systemic hypoperfusion and acidosis. Therefore, it is crucial to replace the exact amount of intravascular fluids in patients undergoing surgery. Before administering fluids during surgery, it is important to measure the body's response to the fluid to avoid both hyper-fluid treatment and hypo-fluid treatment.
The analysis of research in this field shows conflicting results. A survey conducted in 2016 examined the impacts of targeted fluid therapy during surgery compared to traditional fluid therapy. This analysis encompassed 23 studies involving a total of 2099 patients: 1040 who received GDFT and 1059 who were treated with conventional fluid methods. The implementation of GDFT led to a notable decrease in morbidity, duration of hospital stays, and length of time in intensive care. Nonetheless, while there was a reduction in the mortality rate and overall hospitalization time for the targeted therapy group, no statistically significant differences were found (3).
In another review study conducted in 2018, results showed that targeted fluid therapy resulted in fewer side effects with colloidal treatment compared to crystalloid treatment, possibly due to less fluid therapy during surgery or the type of colloid used (14). A 2016 review study analyzing fluid therapy in non-cardiac surgeries in Portugal included a total of 10 RCTs with 1527 patients. The study showed a significant reduction in mortality associated with GDHT compared to conventional fluid therapy. However, the reduction in deaths was not remarkably significant (15). According to some clinical studies, GTD has led to better clinical outcomes. In a meta-analysis that reviewed 23 studies, side effects of surgeries were reported. Overall, 4805 patients across all 29 studies were included. The use of preventive hemodynamic intervention with GTD navigation significantly reduced surgery-related deaths. Consequently, they concluded that applying a preventive strategy of hemodynamic surveillance and GTD could reduce surgery-related mortality (16).
However, reports indicate that GTD offers no clinical advantages. In a randomized controlled clinical trial for adult patients undergoing colorectal laparoscopic surgery, ileus was used as the primary postoperative outcome. The study analyzed 128 patients, with 64 in both the GTD and control groups. The occurrence of early ileus following surgery was recorded at 22% for both the GTD group and the control group. Throughout the surgical procedure, individuals in the GTD group were administered a lower volume of intravenous fluids (mostly less crystalloid) while receiving a higher volume of colloids. Those in the GTD group exhibited more significant increases in SVA and CO. There was no significant difference between the two groups in terms of hospitalization duration, side effects within the first 30 days post-surgery, and mortality. Therefore, researchers concluded that GTD during surgery does not offer benefits over traditional fluids in reducing early ileus after colorectal laparoscopic surgery (17).
In 2014, a study examined the effect of targeted fluid therapy in patients undergoing large orthopedic surgeries. The findings indicated that the amount of injected fluids during surgery was less in the targeted group, and hemodynamic stability was better maintained. Our findings are somewhat similar to this study's conclusions (18).
A crucial point here is that targeted fluid therapy does not mean reducing the amount of volume input fluids in a patient or lowering their blood pressure. Its main goal is managing and controlling the amount of input fluids and other injected blood products to avoid overloading the heart and other crucial organs, thus reducing secondary side effects and postoperative mortality.
The results of this study align with a study conducted in 2011, which concluded that there was no significant difference concerning cardiac side effects between patients undergoing targeted fluid therapy and those in the control group after surgery. The only notable difference was that urinary output was higher in patients of the targeted group (19). In contrast, a study in 2010 claimed that targeted fluid therapy significantly reduces side effects and decreases hospitalization duration for patients (20).
On the other hand, another study indicated that targeted fluid therapy reduces surgery side effects and treatment costs for patients undergoing major surgeries (21). Consistent with this conclusion, a 2016 study reported a remarkable reduction in side effects and kidney failure post-surgery among patients who underwent abdominal surgeries with targeted fluid therapy (22).
Additionally, recent meta-analyses have shown a significant reduction in side effects and ICU hospitalization duration post-surgery (23), as well as a decrease in abdominal side effects and infectious ulcers (24) in patients undergoing targeted fluid therapy treatment.
Another study’s results indicated that targeted fluid therapy for abdominal surgery candidates significantly reduced side effects and ICU hospitalization duration after surgery. However, it was noted that while this treatment protocol can effectively reduce side effects during and after surgery, it does not have an effective role in reducing surgery-related mortality. Other studies have shown no significant statistical differences between targeted fluid therapy and the traditional method in terms of side effects during and after surgery (25-28).
Contrary to the previous findings, another study conducted in Italy analyzed spine surgery candidates using targeted fluid therapy (7). In their study, they found that targeted fluid therapy could reduce bleeding, blood transfusion, and hospitalization duration in patients (27).
Such contradictions may arise due to differences in sample sizes, types of surgery, and inclusion criteria among clinical trials. Additionally, variations in fluid therapy methods and the application of existing recovery protocols for patients could contribute to these discrepancies.
An additional advantage of GDT must be tailored based on surgical procedures and patients’ risk levels, meaning it may not be suitable for all surgeries. GDT should not be applied in isolation; rather, hemodynamic management during surgery and the priorities of the patient’s fluid therapy must always be considered. The main goal of GDT is to maximize oxygenation to body tissues by achieving optimal hemodynamic status with the required amount of fluid treatment. An effective GDT program must include the optimization of flow-related parameters.
Abnormal findings may reflect: (A) Stroke volume variation limitations in the prone position (9), (B) relatively short surgeries (under 4 hours), limiting fluid management differences, and
(C) low-risk patients (ASA I-II) having minimal hemodynamic fluctuations.
5.1. Conclusions
The GDFT did not reduce transfusions in this population (P = 0.796), possibly due to study limitations. While it reduced fluid volumes (P = 0.01), broader benefits were not observed. Further research should evaluate GDFT in high-risk patients undergoing longer procedures.
5.2. Limitations
The limitations of this research included: (1) Single-center design, (2) focus on short-duration, low-risk surgeries (ASA I-II), (3) potential unreliability of SVV in the prone position, and (4) lack of postoperative follow-up for renal outcomes.