1. Background
According to the United Nations Program on acquired immune deficiency syndrome (UNAIDS) reports, 62% of youth infected with Human Immunodeficiency Virus (HIV) are women and this difference is increasing (1). In Asia, approximately 50 million women are at risk of acquiring HIV from their sexual male partner with high risk behavior such as paid sex, injecting drug use, unsafe homosexual intercourse. Limitations in accessing HIV prevention, treatment and care services, and economic constraints are examples of gender inequality as a key driver of the HIV epidemic (2).
The underlying mechanisms of HIV infection and the social and economic consequences of this infection significantly differ between men and women. The differences come from biology, sexual behavior and gender differences between men and women in roles and responsibilities and access to resources. The difference in HIV prevalence between men and women is narrowing. The differences in sexual transmission of HIV, pregnancy and childbearing are important issues in this field. Gender norms, violence, health-seeking behavior, health programs and services are other related issues (3).
A collaboration of 23 HIV seroconvert cohort studies from Europe, Australia and Canada reported no significant gender difference before 1997, but from 1997 onwards, women had a lower risk of AIDS and death (4). A Swiss HIV cohort study has shown that mortality risk for men and women was the same. There are conflicting results regarding this issue (5). Results from the United States showed that among those not undergoing therapy, women had lower survival rate compared to men but gender did not affect the survival of individuals who were undergoing antiviral therapy (6).
In comparison to men an equal duration of infection, women have higher CD4 and lower viral load. In general, these findings do not interpret progression rate or response to highly active antiretroviral therapy (HAART) (7). A cohort study on injecting drug users in Spain showed that HIV progression was different between participants, and women experienced lower HIV progression before and after 1997 and their compliance with medicine was higher than men. In most studies no difference has been shown in HIV progression to AIDS relative to gender. However, some have found a number of differences between pre-and post-treatment. Some reported rapid clinical progression in women although others have reported slower HIV progression (8).
An earlier study showed faster clinical progression in women compared to demographically matched men, which may be due to delay in starting antiretroviral drugs or prophylaxis. The clinical course of HIV infection differs in women due to pregnancy and child bearing, anemia as a specific issue and older age at the time of infection with HIV. Many HIV-infected women are from more underprivileged populations among whom discrimination, violence and other stressful situations are common. They are prone to adverse effects of HIV infection. Nevertheless, plasma HIV RNA levels are lower for women than men, and after adjusting for confounding factors such as CD4 cell count, race and drug use, the progression rates to AIDS were similar (7, 9).
Among factors studied as predictors of HIV progression, gender and mode of transmission have had less effect (10). A study from the United States found that the relative survival time between AIDS diagnosis and death did not differ by race/ethnicity, sex, population density, or diagnosis year but a lower number of women progressed to AIDS compared with men (11). The natural history of infection might be affected by CD4 count, age at seroconversion and mode of transmission (12). A cohort study on 1199 people infected with HIV showed that 225 subjects (18.8%) progressed to AIDS during a follow up of 5.8 years. The results showed that people of older age had a more rapid progression compared with exposure categories (13).
A study from 15 countries on 13030 HIV-1-infected individuals investigated the effect of exposure categories on HIV survival time. Median survival time was 12.5 years for those aged 15-24 years at seroconversion and 7.9 years for those aged 45-54 years at seroconversion. Progression to AIDS changed survival time to 11.0 years for those aged 15-24 years and 7.7 years for those aged 45-54 years. The five exposure categories, sex between men, injecting drug use, transfusion, and hemophilia did not differ significantly (14).
2. Objectives
To the best of our knowledge no study has investigated gender differences among people with HIV in Shiraz, thus we decided to examine gender differences in HIV progression to AIDS and death among people living with HIV in Shiraz, southern Iran.
3. Patients and Methods
To compare survival rate between men and women living with HIV, a historical cohort study was conducted using data obtained from the Shiraz Voluntary Counseling and Testing (VCT) Center. The study was based on data from 1996 to 2012. HIV infected subjects who were 17 years or older and antiretroviral therapy (ART) naive were included in this study. Basic demographic information, such as age at diagnosis, current age, gender, mode of HIV transmission, and education were extracted based on the dates of the reported positive Western Blot (WB) tests. The extraction process was not patient-identifiable. The exclusion criteria included having AIDS at first diagnosis. The diagnosis of AIDS was made according to laboratory results or clinical manifestations.
We examined gender differences during the time between HIV, AIDS and death. Kaplan-Meier survival curves and log-Rank test were used to display and test gender differences in AIDS and death events over 15 years after diagnosis of HIV. Cox proportional hazard regressions were constructed to examine the influence of age at the time of diagnosis and sex on survival time between AIDS and death. Bootstrap was used for estimation of parameters. A P value of less than 0.05 was considered statistically significant and the SPSS 16 software was used for statistical analysis.
4. Results
Among the 1721 enrolled subjects who met the inclusion criteria, 1456 (84.6%) were male and 265 (15.4%) female. Among all transmission routes, injecting drug use (IDU) was the most frequent for men (1262 = 86.7%) and sexual transmission was the most frequent for women (226 = 85.3%). Mean age and mean age at diagnosis were 39.67 ± 8.67 and 34.67 ± 8.34 years, respectively. During the 180 months of follow up, 805 (46.77%) AIDS [642 (44.09%) men, 163 (61.50%) women], 449 (26.08%) deaths [389 (26.71%) men, 60 (22.64%) women] were detected.
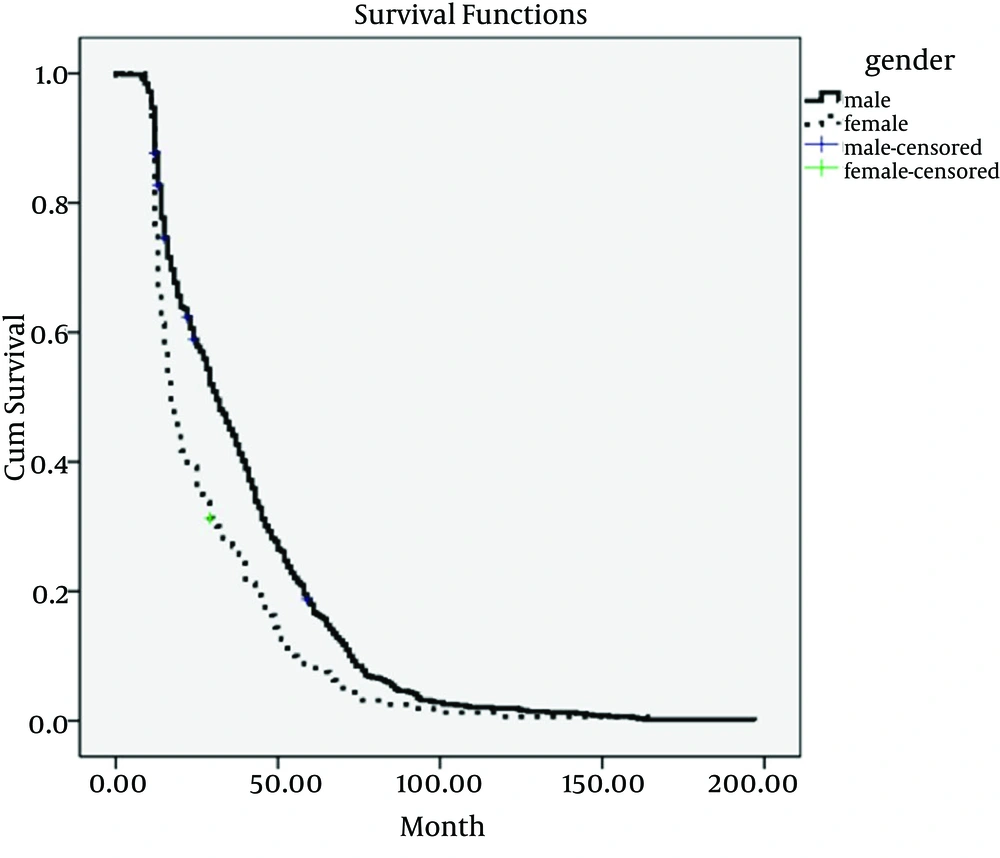
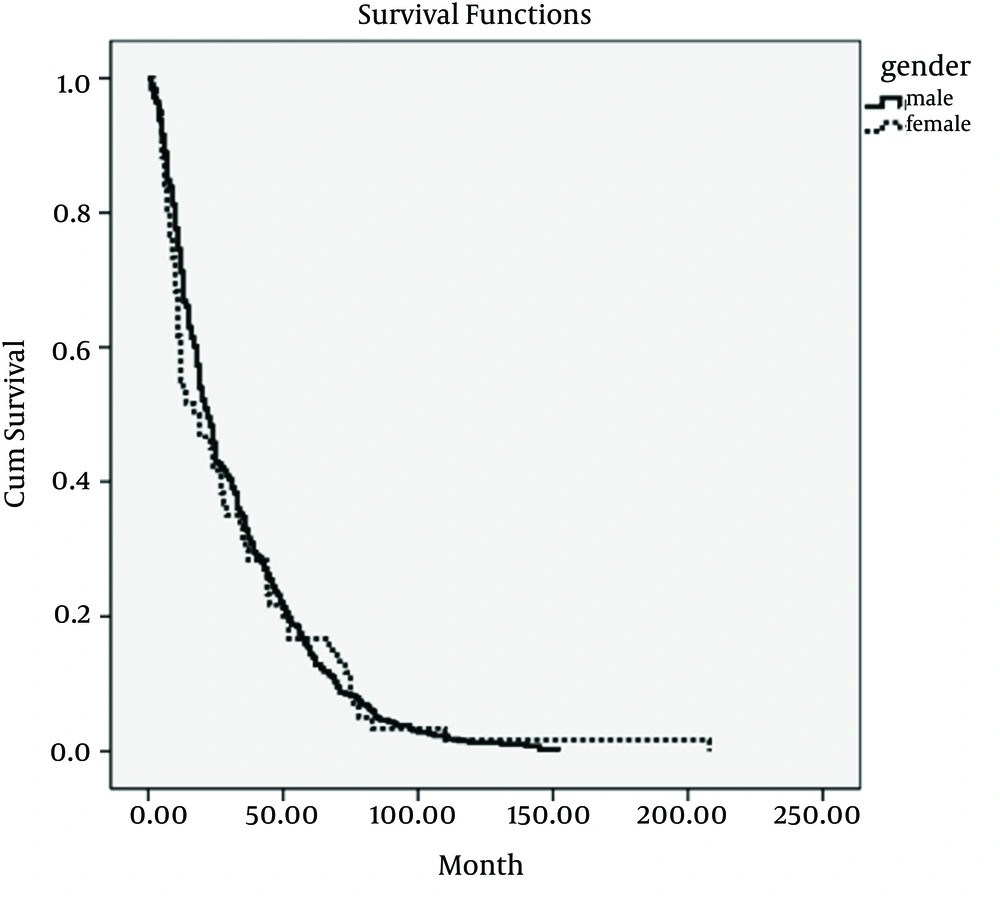
The mean (SE) time between HIV and AIDS was 35.98 ± 0.95 months (38.04 ± 1.09 for men and 27.85 ± 1.80 for women, P < 0.001, log rank test) (Figure 1). The median (95% CI) was 29.00 (26.44-31.55) months overlay, 31 (28.04-33.95) months for men and 17(14.61-19.38) months for women. Mean (SE) time between HIV and death was 31.74 ± 1.36 months (31.83 ± 1.41 for men and 31.15 ± 4.47 for women, P = 0.773, log rank test) (Figure 2). The median (95% CI) was 22.00 (19.60-24.38) overlay, 22 (19.58-24.41) months for men and 17 (3.08-30.09) months for women. The HIV-infected women, as compared with men, had faster progression to AIDS (odds ratio = 3.52) (Table 1).
| Event | β Coefficient | P Value | ORa (95% CI) |
|---|---|---|---|
| Death | |||
| Gender | |||
| Male | Baseline | - | 1 |
| Female | -0.626 | 0.169 | 0.535 (0.219-1.30) |
| Age at time of diagnosis | 0.00 | 0.996 | 1.00 (0.988-1.013) |
| Interaction of sex-age at time of diagnosis | 0.02 | 0.112 | 1.020 (0.995-1.045) |
| AIDS | |||
| Gender | |||
| Male | Baseline | - | 1 |
| Female | 1.26 | < 0.001 | 3.52 (1.85-6.72) |
| Age at time diagnosis | .031 | < 0.001 | 1.031 (1.021-1.041) |
| Interaction of sex-age at time of diagnosis | 0.024 | 0.006 | 0.976 (.960-993) |
a Abbreviations: ORa, odds ratio adjusted; CI, confidence intervals.
5. Discussion
A report from Iran states that proportion of HIV infected women has increased from 7% to 8.7%. The main mode of transmission in Iranian women is sexual contact with their infected husband (15). A joint report by UNAIDS/UNFPA/UNHFEM stated that half of injecting drug users in Iran were married and a third had remarked having an extra-marital relationship (16). On other hand, knowledge about this disease and its route of transmission is low in Iran. Self-reported HIV testing among Iranian women was lower than a previous study (17).
Women biologically and socially are more prone to HIV infection than men. In developing countries, women are more prone to this infection due to lack of empowerment in sexual relationships, forced sex, unprotected sex, and sex with men who are likely to be infected with the virus. They are more affected by this virus because of stigma, lack of access to treatment and cost of antiviral drugs in many countries (1). As we know, no study has investigated gender differences in Iran although contradictory results have been reported from other countries. This study showed that HIV-infected women, as compared with men, had faster progression to AIDS. This result may indicate that women’s referral to health centers is delayed, so they are diagnosed during the developed stages of the infection. Univariate and multivariate tests were used and no difference was found between survival time of men and women. Although women are diagnosed late, due to the fact that men do not refer to health centers routinely and have less compliance with medication, survival rate of both genders was equal.
Before introduction of HAART in 1997, no gender differences in mortality and HIV progression to AIDS was detected whereas from 1997 onwards women had lower risk of death compared to men (4); this might be due to the healthier lifestyle of women and lower rate of violence, death, and better response to health intervention among women. A cohort study from Europe, North America, and Australia investigated survival or time to diagnosis of AIDS before widespread use of HARRT. This study showed the same results as a previous study (14). We found that disease progression in women was faster than men and median of time from diagnosis to AIDS in women was less than men. Gender difference was not significant between men and women regarding survival time of AIDS to death.
A study in Singapore found that among investigated factors such as gender, ethnic groups, occupation and mode of sexual transmission, none were associated with disease progression; this study also showed that older age at diagnosis and baseline CD4 cell counts were measurable predictors for HIV progression to AIDS (12). The result of this study was not in agreement with that of our study. However, another survey found similar results to that found by the study from Singapore. These results support the assumption that when equal access to medical intervention is available, the impacts would be similar for different genders, ethnic groups, occupations and modes of sexual transmission (18, 19).
A study from New York found that factors that impact the survival rate of individuals are different depending on HARRT. Age and time since seroconversion were effective factors before the HAART era. After 1996, factors that affect survival include socioeconomic status, access to care, onset of therapy, physician’s experience in care and treatment of HIV/AIDS individuals, compliance with complex medical instructions that may result in drug resistance to antiviral drugs (20).
In order to slow down disease progression, it is not important to know the effective factors, inconvertible genetic or environmental and social factors on gender differences; what is important is to have equal access to medical interventions (19). In comparison with men, in equal situation of access to care, women have a healthier behavior and compliance with medication, and are more alert about health (4). The difference in progression from the initial diagnosis of HIV to AIDS may be due to access or adherence to treatment or late diagnosis process (11). The inconsistency of the obtained results could be due to differences in the study design and residual confounding by social and economic situations (8). Most studies have shown that in equal situations of access to health care, gender differences do not influence the disease prognosis (11, 12, 19). Gender differences in our study can be attributed to the lack of equitable access. Social and economic barriers may be the reason for unfair access. As we know, in Iran, HIV/AIDS health care is provided equally for women and men. However, some social and economic factors are obstacles for receiving counseling and prevention and treatment services equally.
A qualitative study was conducted among HIV positive women about their life experience in Iran. The main factor that researchers found was negligence, especially about the sexual transmission route of HIV. The first challenge of these women was rejection from family and the society and loss of their jobs. Most HIV infected women did not refer to medical services due to embracement and fear (21). A survey from five provinces of Iran showed that health literacy was low especially in particular groups such as women. Education level was the most important factor in improving health literacy (22). These two studies found barriers among HIV positive women in Iran regarding access to health centers.
In conclusion, identification of risk factors that contribute to disease prognosis empowers healthcare workers to provide suitable counseling and deliver proper health care services. The community should build strong infrastructure to combat this challenge, by improving public awareness about the modes of transmission. Initiating a supportive financial system to help these women, improving reproductive health services, paying attention to their children and their education (especially health education), are strategies to overcome discrimination. Adequate training of health care workers who work with HIV positive women and family of HIV infected men to overcome their fear and embracement and implantation of preventive programs for HIV infected men’s family seem to be necessary.