1. Background
Chronic obstructive respiratory diseases (CORDs) are a substantial public health problem (1). Despite their preventable and curable nature, CORDs including asthma and the chronic obstructive pulmonary disease (COPD) are still a growing problem, both in developed and developing countries (2).
As the fifth major cause of death, the prevalence of COPD was estimated to be 5.2% based on the physician diagnosis and 15.1% based on lung function testing among US adults (3, 4). Also, there are 300 million asthmatic patients worldwide who are responsible for 1% of the total burden of diseases and 250,000 deaths per year (4-6).
In Iran, according to the latest reports, the prevalence rates of asthma and COPD were estimated to be 10.80% and 9.2%, respectively (6, 7). Due to the aging population, social industrialization and changes in the pattern of tobacco consumption, the prevalence of CORDs has been increased in developing countries like Iran (3, 4, 6). Despite increase in the prevalence of this preventable disease, health policy makers and governments have not paid enough attention to these issues. One of the major reasons for this ignorance is lacking the precise information on the CORD prevalence and its major determinants (8, 9). There are scanty population-based surveys on the prevalence of CORDs in adult population of Shiraz, and there is no study on the prevalence of CORDs in adult population and its relation with socioeconomic determinants.
This study was conducted to provide a population-based data for the prevalence of CORDs and explore its association with socioeconomic determinants in adult population of Shiraz, Iran.
2. Objectives
The present study was conducted to measure the prevalence rates of COPD and asthma and their socioeconomic determinants, and also to assess the sensitivity and specificity of the COPD diagnosis questionnaire compared with the lung function testing as the gold standard.
3. Methods
3.1. Overview
This cross sectional survey was conducted on urban and suburban population of Shiraz city, the capital of Fars Province, Iran, from August to December, 2015.
3.2. Ethical Consideration
The local ethics committee of Shiraz University of Medical Sciences approved the protocol, which adhered to the tenets of the declaration of Helsinki (1975). After individuals were notified of the study objectives, voluntary participation and right to withdraw, oral informed consent was obtained from them. The confidentiality of all personal data was preserved.
3.3. Study Population and Sample Size Estimation
3.3.1. Shiraz Population
Shiraz city is a capital of Fars province, Iran. The 2011 census recorded Fars region’s population as 4.59 million that 1.7 million of them are living in the Shiraz city and marginal zones (10). The sampling frame was individuals of the urban and suburban zones of the Shiraz. Table 1 demonstrates the Shiraz population distention in the 9 municipal districts based on the 2011 census data. Accordingly, the study included more than 6000 noninstitutionalized inhabitants 20 and older than 20 years from the 9 municipal districts of Shiraz, Iran. The sample consisted of 0.5% of the 1,219,237 total inhabitants aged ≥ 20 years in the survey area.
| Districts | Populationa | Households | Sample | Participation |
|---|---|---|---|---|
| 1 | 235,262 (13.8) | 63,584 | 860 | 858 |
| 2 | 243,083 (14.3) | 65,698 | 888 | 877 |
| 3 | 239,030 (14.1) | 64,603 | 873 | 866 |
| 4 | 246,160 (14.5) | 66,530 | 899 | 855 |
| 5 | 175,847 (10.3) | 47,526 | 638 | 633 |
| 6 | 180,669 (10.6) | 48,829 | 658 | 652 |
| 7 | 195,434 (11.5) | 52,820 | 715 | 705 |
| 8 | 69,206 (4.1) | 18,704 | 260 | 247 |
| 9 | 115,996 (6.8) | 31,350 | 423 | 416 |
| Total | 1,700,687 (100) | 459,645 | 6 214 | 6 109 |
aValues are expressed as No. (%).
3.4. Inclusion Criteria
All noninstitutionalized adults ≥ 20 years in Shiraz, who had sufficient ability to cooperate well during the interview and further examinations were included in the study.
3.5. Exclusion Criteria
Inhabitants did not consent to participate were excluded from the study.
3.6. Sample Size
For sample size calculation, a complete literature search was performed. There was no population-based study about the prevalence of CORDs in Shiraz, but the prevalence rates of asthma and COPD were reported 10.8 and 9.2, respectively, in recent studies in Tehran (6, 7). Considering these reports the prevalence of CORDs was estimated to be approximately 9% in our study population.
Using the formula;
N = (z1 - α/2)*p (1 - p)/d2
A minimum sample of 5593 subjects were required based on the Z = 1.96 (the desired level of confidence 95%), margin of error = 0.75% and P = 9%. Considering a participating rate of 90%, the final sample size was calculated to be 66 152 subjects.
3.7. Sampling Plan
The target population was defined as all urban and suburban citizens, aged ≥ 20 years, who reside in Shiraz city in the year of study. The sample was selected based on the stratified random sampling method proportionate to the number of municipal districts and strata.
The sampling was performed in two stages:
- First stage: stratification
Considering the 9 municipal districts of Shiraz city and stratification of the sample, we selected the participants. Proportional to the total number of the sample size, household size, and logistical facilities, the appropriate number of blocks in each municipal district was calculated using the Microsoft Excel 2007 software (Table 1).
- Second stage: random sampling
After identifying the index household in each block, the interviewer enumerates 10 neighbor households systemically by the clock-wise rotation. If there is more than one eligible person in selected households, the Kish selection method was used to choose the right participant.
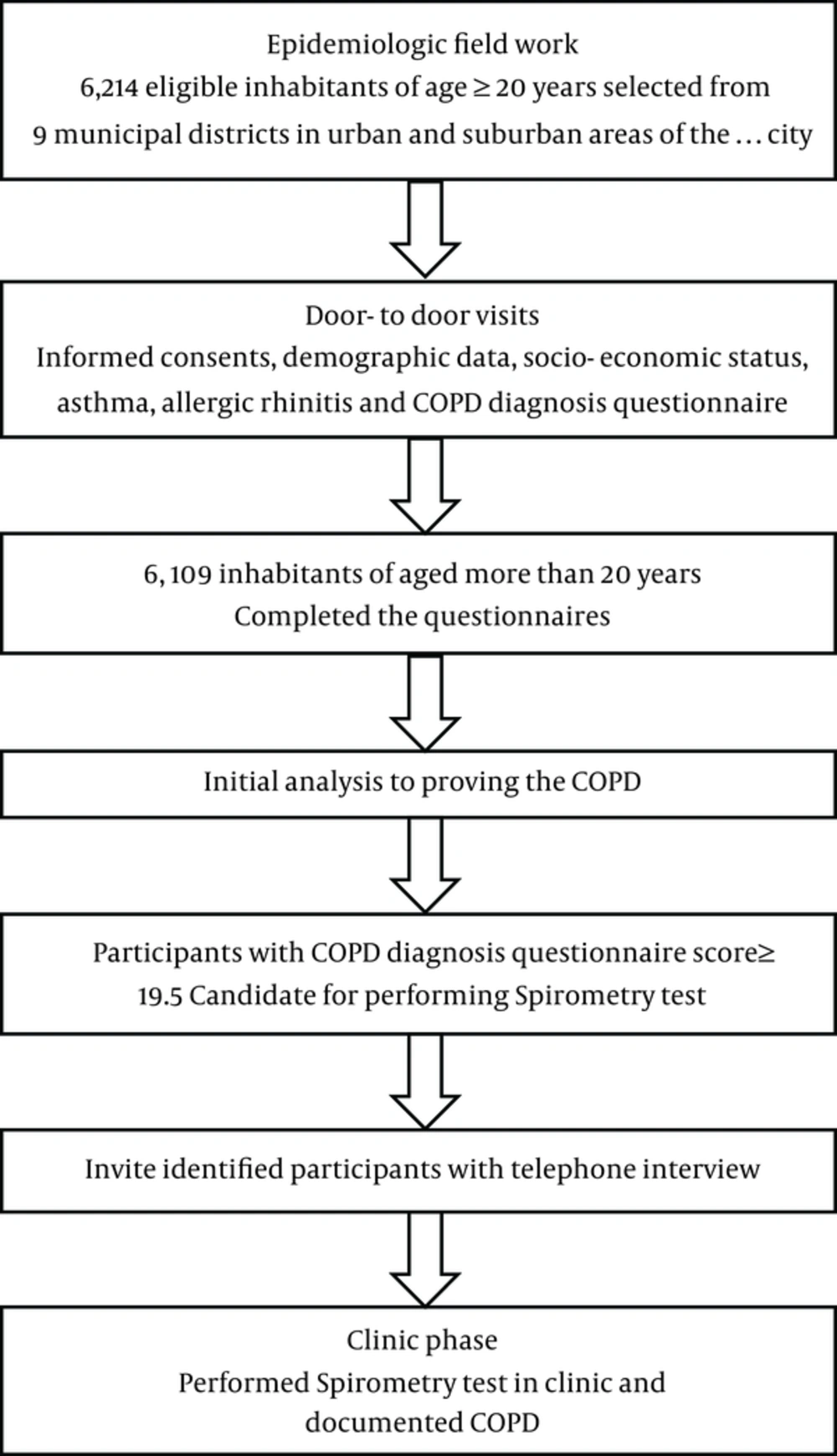
3.8. Recruitment Process and Questionnaires
The recruitment process was started with necessary coordination to obtain official permission to visit homes. By presenting their identification cards, interviewers introduced themselves and explained the project to the main member of the households; eligible members were invited to complete the questionnaires. At the end of the interview, we asked about the participants’ cooperation to perform spirometry if necessary for proving the respiratory disease. Following the completion of recruitment and an initial analysis process, we called and invited the participants with the COPD diagnosis score more than 19.5 (11) to pass the spirometry test in the clinic (Figure 1).
3.9. Nonresponse
Following the initial invitation, we tried two other episodes of recruitment, subjects who did not attend the interview process or spirometry test were considered as nonrespondents in this study.
3.10. Questionnaire
The main questionnaire that covered respiratory symptoms was developed from prior validated questionnaires that had been used in several studies (11, 12). Demographic factors including age, gender, self-reported weight and height and marital status were recorded. The educational level, occupation, residency location and income were being considered as a proxy of the socioeconomic status of each household. Residential areas were classified as urban and suburban districts. Self-reported education was measured by asking each subject about his/her educational level. Finally, responses were combined into three categories including basic, secondary, and higher educational levels. Household income was defined as a sum of all family member income, which received during one year. The classification was based on the median income of all households in Iran.
3.11. Definitions
3.11.1. Asthma
We considered current asthma if at least one of the following factors presents in the last year: 1) awakening by an attack of shortness of breath, cough, or chest tightness without any identifiable cause, 2) having an asthma attack, 3) currently using medication for asthma and 4) having wheezing or whistling in the chest not associated with a cold or the flu (12). Ever diagnosed asthma was defined as responding “yes” to the question “Has a doctor ever said that you had asthma?”
3.12. Chronic Obstructive Pulmonary Disease
A diagnosis of COPD should be considered in each subject with symptoms of cough, productive sputum, dyspnea and history of exposure to risk factors. According to the COPD diagnosis questionnaire, participants who have the COPD diagnosis score more than 19.5 will be candidates to performing spirometry (11). Airway obstruction and its severity are defined as the forced expiratory volume 1 (FEV1)/ forced vital capacity (FVC) of lower than 70% based on the revised GOLD criteria (13).
3.13. Cigarette Smoking
Cigarette smoking was defined as active smokers who smoke at the present time and past smokers those who had previously quit smoking. In all participants, duration and number of per day cigarette smoking was recorded.
3.14. Waterpipe Tobacco Smoking
Waterpipe smoking was defined as active water-pipe smokers who smoke daily or more frequent at the present time and past smokers those who had previously quit smoking (abstinence from smoking). In all participants, the amount of usage per head of tobacco and duration of smoking in years were assessed.
3.15. Second-Hand Tobacco Smoke
Second-hand smoke was assessed by whether or not they frequently inhaled waterpipe or cigarette smoke at or outside the home.
3.16. Spirometry
Spirometry was done by a specially trained technician in the clinic according to the American thoracic society (ATS) recommendations (14). Spirometry was performed before and after the administration of 200 mg (2 puffs) of salbutamol using the spirometer (ZAN 100; Oberthulba, Germany) for any subjects suspicious to have obstructive lung diseases. The primary spirometry measurements including the FEV1 and the FVC, and FEV1/FVC were measured and analyzed.
3.17. Quality Assurance
Before starting the project, several training courses were carried out for the study staff about the study purposes, sample selection method, interview, questionnaires and technical skills needed to conduct the protocol. During the study period (approximately 6 months) the accuracy of interviews were controlled and verified by project observers every week. In addition, the validity of the data was reviewed periodically; the director verified 10% - 15% of the questionnaires to monitor the data precision in each cluster and feedback was given to the observers monthly. The spirometry instrument was calibrated daily by trained operators using the manufacturer’s guidelines.
3.18. Data Handling and Statistical Analysis
3.18.1. Data Entry and Editing
On completion of interviews on each block, data were entered and checked. At the clinic, relevancy of the spirometry data has been evaluated by the supervisor. Missing or wrong data were obtained after evaluating the process and consulting with related interviewer. During data entry, the completeness and consistency of the questionnaires were checked by the data entry software.
3.18.2. Statistical Analysis
We used the SPSS software version 15.0 (SPSS Inc, Chicago, Illinois, USA) for analyzing the data. The accuracy of the final data was assessed by a qualified statistician. Demographic and socioeconomic characteristics of the participants, and participation rate of different districts of the survey area were presented using descriptive statistics. Main variables were presented as mean (SD), range or frequency and percentages. A P value of less than 0.05 was regarded as statistically significant.
4. Discussion
The presented protocol describes the design, methods and respiratory evaluation of the subjects in the cross sectional, population-based survey in Shiraz, Iran. We intended to provide a valid data source about CORDs via the proper quality assurance processes. The collected data from this study are supposed to indicate the prevalence of CORDs and their related determinants in the studied population. Such data could be an important advocacy tool for policy makers. They can develop targeted approaches for prevention of CORDs, and as a result have a great cost saving in their healthcare system. The biggest challenge of this study was the participants’ drop-out. To increase the participating rate and solve the challenges at the clinic, certain approaches were implemented: the clinic was open during early morning (7:30 - 9:00 AM) and noon (12:00 - 14:00 PM) five days per week, a certain visit time of the clinic was devoted to the study participants, and spirometry costs were waived. We anticipate that future reports from the Shiraz adult respiratory disease study would estimate the prevalence of CORDs and its related determinants in the community. This study would also provide basic information about patients who should be targeted by respiratory disease prevention programs.