1. Background
Elbow arthroscopy, which was first proposed in 1931, is increasingly used to diagnose and treat pathologies of the elbow (1). However, the unique anatomical complex of the elbow, limited intra-articular space, and existence of vital neurovascular structures in this area delayed advances in elbow arthroscopy for nearly half a century. Fortunately, advances in arthroscopic techniques with increase in knowledge of elbow anatomy strengthened elbow arthroscopy again for the treatment of various diseases in the early 1980s (2-4). In the last few years, elbow arthroscopy has become more common than ever. The number of elbow arthroscopies has doubled over the last decade and accounts for approximately 11% of all arthroscopy cases (5, 6). At the outset, the indications of elbow arthroscopy were limited and included patients, who complained of pain and loss of function or limited range of motion, and at the same time, clinical examination and X-ray findings were normal. Gradually, diagnosis and treatment of intra-articular pathologies (diagnostic arthroscopy), picking up of free objects, removal of osteophyte, synovial biopsy, synovectomy, separation of adhesions, and osteochondritis dissecans lesions were indications of elbow arthroscopy (7, 8). With further progress of this technique, its indications were also increased and intra-articular complex problems, such as elbow arthritis and contracture, extra-articular pathologies, such as biceps tendon disorders and lateral epicondylitis, and treatment of fractures were developed. Contraindications of this method are very limited and include changed neurovascular anatomy after previous surgery and/or existence of deformity. Also, little or lack of experience of the surgeon is considered as a relative contraindication (9, 10).
This evaluation and the therapeutic method in the elbow provides the opportunity for the surgeon to review intra-articular structures clearly, produces lower postoperative pain, reduces the infection rate, and leaves a much smaller scar in comparison to open surgery (11, 12). Review of the literature shows that the overall complication rate of elbow arthroscopy is about 6% to 15%, approximately half of which would constitute neurological injuries (5, 8, 13, 14). Infections and injuries to the nearby nerves of elbow joint are the most common complications of this technique (14, 15). These injuries involve a range from transients to irreversible damages. Other complications, which are very rare, include heterotopic ossification, compartment syndrome, septic arthritis, superficial infection, arthrofibrosis, and arthroscopy equipment breaking in the joint (5, 14).
Results of this method are almost entirely dependent on the high expertise and exact use of modern arthroscopic techniques and equipment, hence, long term learning period is considered for this diagnostic-therapeutic method (5, 7). Although available evidence is more in favor of the usefulness of this therapeutic method in elbow diseases, there is no sufficient evidence for preference and usefulness of this therapeutic method in elbow diseases, as suggested by a number of review studies (16). Since this method is very modern and almost no researches have been done on the indications, results, and complications of this technique, this study could be the beginning of research in this field in Iran. The current research tried to aid the understanding of the advantages and disadvantages of this method due to lack of similar studies in Iran and at the same time the effectiveness of this method in other countries.
2. Methods
This study was an analytical case-series study. All patients, who underwent elbow arthroscopy in a referral center during 2013 to 2015 were included. The number of these patients was 18. The standard arthroscopic equipment included a 4-mm arthroscope with a 30° angle, water pump with pressure control lever and flow regulator, shaver, pincer, and ultrasonic coagulator. The patient was positioned in the lateral decubitus position and one support was placed in the distal of arm to forearm that was free and suspended. Tourniquet was used during the surgery. Wrist and forearm plastic bandage was used to prevent liquid penetration to the interstitium. After distension of elbow joint, the joint was entered through the mid-lateral portal at the center of olecranon, lateral epicondyle, and head of radius triangle. Then, posterolateral portal was created in the front of olecranon head and lateral of triceps muscle. Anterior compartment is primarily accessible at 2-cm proximal to lateral epicondyle through proximal lateral portal. Proximal medical portal was induced by arthroscopic vision and illumination creation through the skin. The joint was completely washed with saline and movement was begun immediately after surgery and physiotherapy.
Patients were grouped in one of the following eight groups based on surgery indications:
Diagnostic arthroscopy
Removing free objects
Arthrolysis (separation of adhesions and elbow stiffness)
Removing of osteophytes and debridement in elbow arthritis
Synovectomy in rheumatoid arthritis
Elbow OCD
Removal of foreign body
Treatment of tennis elbow
By evaluation of medical records and patients questionnaires, which were obtained before and after surgery and at final visit (one-year after surgery), pain status and function of the elbow based on VAS visual scale, maximum range of motion in involved elbow against opposite side in pronation and supination, flexion-extension, therapeutic results after surgery with the help of Quick Dash Disability of Arm Shoulder and Hand Questionnaire (17), postoperative complications (including infection, nervous damage, and compartment syndrome), range of elbow movement before and after surgery and demographic information (age and gender), were obtained. The Quick Dash questionnaire contained 11 five-choice questions, in which the patient could obtain a score between 11 (best situation) and 55 (worst situation). The VAS questionnaire covered a range of without pain to most imaginable pain with a score of 0 to 10. For final statistical analysis, the SPSS version 19 was used. Absolute and relative frequency (percentage) for description of qualitative variables and mean and standard deviation (with 95% confidence interval) for quantitative variables were used. The T test was used for determination of changes in pain, function and range of movement of elbow before and after arthroscopy; P < 0.05 was considered as significant difference.
3. Results
Among 18 evaluated patients, there were 14 males (77.8%) and four females (22.2%). Mean age of the participants was 36.11 ± 6.14 years, of which four patients (22.2%) were less than 30 years old, 10 patients (55.6%) were 31 to 40 years old, and four patients (22.2%) were in the range of 41 to 50 years old. Minimum and maximum age was 24 and 47 years, respectively.
Thirty-two indications of elbow arthroscopy were found in 18 patients. Most of the indications were arthrolysis (12 cases) and removal of osteophytes and debridement in elbow arthritis (9 cases). Frequency of arthroscopic indications of elbow in evaluated patients is summarized in Table 1.
| Indications of Elbow Arthroscopy | Number | Percentage (of Total 18 Cases) |
|---|---|---|
| Arthrolysis | 12 | 66.7 |
| Osteophytes removal and debridement in elbow arthritis | 9 | 50 |
| Extraction of free objects | 4 | 22.2 |
| Synovectomy in rheumatoid arthritis | 2 | 11.1 |
| Removing foreign objects | 2 | 11.1 |
| Diagnostic arthroscopy | 2 | 11.1 |
| Elbow OCD | 1 | 5.5 |
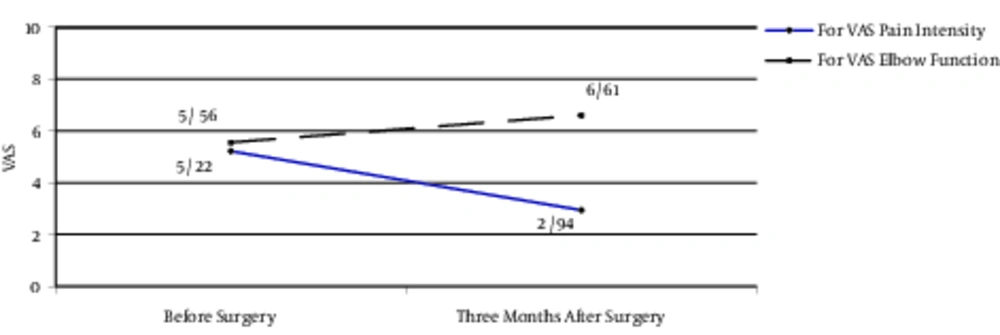
Based on the VAS visual scale, mean score of elbow pain intensity in patients was 5.22 ± 1.7 before the surgery and 2.94 ± 1.73 at final follow-up. In comparison with changes of pain intensity by paired t test, a significant difference in VAS before and after surgery was detected (P < 0.001). Also, by using the VAS visual scale, mean score of elbow function in patients was 5.56 ± 2.14 before the surgery and 6.61 ± 2.17 at final follow-up. In comparison with changes of elbow function by paired t test, a significant difference in VAS before and after surgery was detected (P < 0.001, Figure 1).
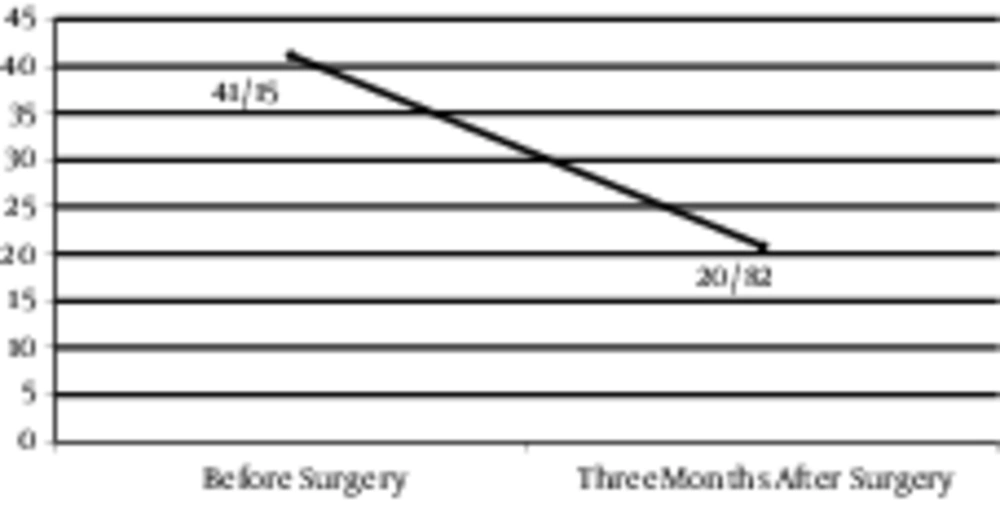
The mean score obtained in Quick Dash questionnaire was 41.2 ± 16.5 before the surgery and 20.8 ± 12.9 at final follow-up. Comparison of these scores with paired t test, revealed a significant difference before and after surgery (P < 0.001, Figure 2).
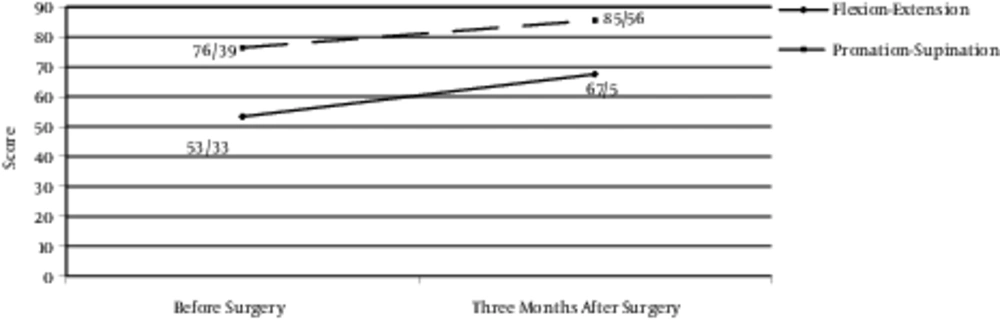
Based on clinical examination, range of movement in flexion-extension was 53.33 ± 25.02 before the surgery and 67.5 ± 26.41 at final follow up and this difference was shown to be statistically significant using the paired t test (P < 0.001). Also, range of movement in pronation and supination changed from 76.39 ± 13.26 before the surgery to 85.56 ± 11.99 at final follow up, which was statistically different (P < 0.001, Figure 3).
It must be mentioned that no complications, such as infection, nervous damage, and compartment syndrome were seen in patients in the follow-up.
4. Discussion
The present study was an analytical case-series study, in which 18 patients were evaluated. This number of patients is lower than other studies due to the limited number of performed arthroscopies. Mean age of the patients was 36 years, which is near values reported in other studies. For instance, 41.4 years was reported by Clasper (18).
The current patients underwent arthroscopy with different indications. Among them, the most common indication was arthrolysis and removing osteophytes and debridement in elbow arthritis. However, most indications in Garg’s study was related to removal of free objects, articular surface debridement and intra-articular adhesions, release of capsular contracture lower than 45 degrees and removal and extraction of impingement related osteophytes (19). In the study of Marti et al., osteoarthritis, stiffness, and foreign body of elbow joint were the most common indications of elbow arthroscopy (8). Also, Adams et al. reported that the most common indications of elbow arthroscopy were debridement of septic arthritis, synovectomy in elbow inflammation, osteoarthritis debridement, and treatment of osteochondral defects (13).
In the study of Schubert et al., 24 patients, who underwent elbow arthroscopy for a 12-year period were followed for six years (12). The DASH score after the surgery was 56 and VAS for pain and function were 2.6 and 6.9, respectively. They found that elbow arthroscopy was a safe and effective method, without associated permanent and severe complications, with very slight pain.
Ball et al. conducted a study on 14 patients with contracture after trauma; in this study pain decreased and ROM and function increased after arthroscopy (20). In the study of Kelly et al., which was conducted on 25 patients, with primary elbow osteoarthritis, ROM was increased after surgery (21).
In contrast to the current report, the study conducted by Blonna (5) was a review study, which evaluated the effects of arthroscopy in treatment of elbow stiffness and the indication was ROM return of elbow. They found that, although retrospective studies showed that this method has a good outcome, further studies are needed, especially prospective and clinical trials. Also, Yeoh et al. agreed in this context that although evidence supports the appropriateness of this method, more evaluations and studies are needed to confirm the preference and usefulness of this therapeutic method (16).
In contrast to the current study, which only evaluated the arthroscopic findings, Peart et al. (22) compared the results of arthroscopic and surgical treatments of epicondylitis in 75 patients, and the results of arthroscopic treatment were better. Also, Adams et al. expressed that arthroscopy is an appropriate procedure for treatment of inflammatory arthritis, osteoarthritis, and lateral epicondylitis (13).
Amongst 18 evaluated patients, no arthroscopy related complications were seen, which may be related to the low number of samples. In addition, arthroscopic complications were not so common in this procedure. For instance, in the study of Nelson et al. (14), who evaluated 417 patients, only 37 cases of minor complications and 20 cases of major complications were reported, the most common of which were superficial and deep infections, re-operation needed ossification, and temporary complications of sensory nerves. Also, Marti et al. (8) with similar findings in evaluation of 100 patients, only reported minor complications in five patients, including hematoma, temporary nervous damages, wound healing interference, and complex local pain syndrome.
One of the limitations of this study was the low number of patients, which decreased the value of this study. Performing studies with longer evaluation time is recommended for better evaluation of post-operative complications. Also, it is recommended that future studies be performed on the results of arthroscopic treatments of specific diseases or indications, to better evaluate and compare its results.
4.1. Conclusions
The current study and other studies showed that arthroscopic treatment of elbow joint has low complications and good results. This enables rapid recovery of patients and is a specialized and secure method in the hands of a skilled orthopedist.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all participants included in the study.