1. Background
The term “no-show” is defined as “a patient who misses an appointment or does not show up at the appointment date without advance notice” (1). Increasing the patient’s attendance at appointments and improving access to care are the challenges faced by many health service providers (2). Missed appointments or no-shows are an important challenge in the healthcare industry, whose causes and outcomes have been researched for years (3). Annually, 23% - 34% of outpatient appointments are missed in the United States (4). Although the recorded rates of missed appointments may vary slightly between countries, healthcare systems, and clinical settings, no-show is still a widespread problem around the world (5). Various studies report no-show rates from 3% to 80% (6). In a review study, the mean no-show prevalence is estimated at 23.8%. The highest rate was in North America (27.1%) and the lowest in Europe (14.9%), while it was 24.3% in Asia (7, 8).
The absence of a patient at a predetermined appointment has consequences (9). Patients who miss their appointments do not receive necessary and timely health services, and may prevent or delay the provision of treatment, follow-up, or preventive care to other patients. In general, missing medical appointments has a negative impact on health outcomes; those who lose their appointments are less likely to use preventive health services than individuals who keep medical appointments (4). Patients who do not attend an appointment have 40% - 50% increased rates of emergency department utilization and hospitalization in the future (10). Other negative effects of no-shows include underutilization of medical resources, increase in healthcare costs, decrease in access to care, reduction in revenue and provider productivity (11), and need for additional efforts by staff members to reschedule the missed appointments (9). Missed appointments also indirectly lead to increased appointment lead times, poor quality of care, and patient dissatisfaction (1). In addition, it reduces the opportunity of young physicians to learn from different cases (7).
The most common reason given by patients for no-show was that they “forgot” their scheduled medical appointments (7, 12, 13). Other patient-related factors for missing scheduled appointments are transportation issues, health status or health improvement, miscommunications (4), resistance to consultation, insurance status (14), inability to leave work/school (12), and frustration with outpatient clinic organization, resulting in long waiting times and discontinuity of care. Health-system-related factors include inadequate communication between care team and patients, quality of consultation, waiting room facilities, time interval between scheduling/referrals and appointment, administrative problems, and place of care (14).
Medical providers use different strategies to increase patient attendance and reduce the impact of missed appointments (4). The most common strategies include overbooking and short lead-time scheduling (1, 15), appointment reminders, cancellation policy, patient education, financial incentive (7), providing transportation, scheduling changes (16), and web-based scheduling (17).
Many attempts have been made to minimize the rate of no-shows; however, the problem continues for many outpatient clinics (11). Reducing the rate of no-shows is essential for healthcare providers and managers and understanding the factors that contribute to the absence of a patient in scheduled appointments is an essential step in achieving this goal (18). Iran has a developing health system; there is no evidence of this issue and to the best of our knowledge, this is the first study in this field. To improve the quality of outpatient services, in the first step, it is necessary to identify the burden and determinants of the no-show to provide a clear picture of problem to decision makers. Accordingly, in this study, we investigate the extent of no-show and its possible predictors in outpatient clinics of an academic hospital in Tehran, Iran.
2. Methods
In this retrospective study, the study population includes of all outpatients who had scheduled appointments from March 20, 2016 to March 20, 2017 (1395 Iranian calendar) at Emam Hossein medical center (EHMC) outpatient clinics. EHMC is a general teaching hospital and possesses 560 beds; it provides various inpatient and outpatient health services and is considered as a referral tertiary hospital in Tehran, the capital of Iran. Since 2011, EHMC has tried various appointment systems. Now, it runs four systems that are all linked to the hospital information system (HIS):
- Patient Self-Service Kiosk requires the patient to come to the hospital clinic and wait in the queue of the kiosk to make their appointment for the same day. It enables patients to schedule appointments for the clinic and the doctor that they want to see without needing the help of the desk in-charge.
- Telephone appointment system (TAS) is a system that patients can call the scheduling center between 8 AM and 4 PM to schedule an appointment. Trained nurses triage the patients and, based on their chief complaint, register them to the appropriate clinic.
- Interactive voice response (IVR) is an automated telephonic system that interacts with callers and allows patients to schedule appointments.
- The web-based appointment system (WAS) uses the hospital’s website for scheduling.
It is noteworthy that no reminders and cancellation system is provided for any appointment type.
The data of this study were extracted from the database of HIS. Variables were selected based on their availability in the HIS and consensus development among the researchers and staff. For each patient, the following data were obtained: patient ID number, scheduling date (the date on which appointment was entered into the system), appointment date (the date for which the appointment was scheduled), appointment month, clinic working shift (morning or evening), type of appointment system (TAS, IVR, WAS), clinic name, and the final appointment status (show or no-show). In addition, the appointment lead time was determined by computing the number of days between the scheduling date and the appointment date. Also, we describe a no-show event as a patient that does not show up for the appointment. Walk-in patients (users of self-service kiosks) were excluded from study. No-show rates were calculated based on the number of no-shows divided by the number of scheduled patients.
Data were analyzed using SPSS.21. Continuous variables are presented as means and standard deviations (SD), whereas categorical variables are presented as numbers and percent. Independent two-sample t-test for the quantitative variables and Chi-square test for qualitative variables were used for comparing the variables in the two groups of show and no-show patients.
Backward stepwise logistic regression analysis was used to describe the importance and effect of each predictor of all no-show variables entered into the model. The strength of the relationship was assessed using odds ratios (OR) and 95% confidence intervals (CI).
3. Results
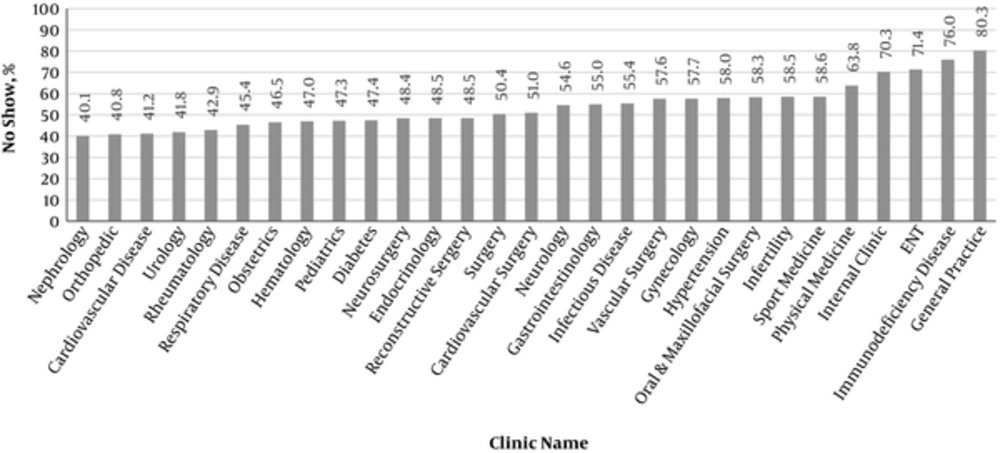
A total of 148077 outpatient appointments were scheduled across the study period, of which 74,138 patients did not adhere to their appointment. Thus, the no-show rate was 50.1%. As shown in Figure 1, general practice (80.3 %) and nephrology (40.1%) clinics had the highest and the lowest no-show rates, respectively (P < 0.001). The no-show rate varied from 45.3% in Farvardin (Mar 20 - Apr 19) to 53.3% in Esfand (Feb 19 - Mar 20). Significant differences in no-shows were observed based on months of appointments (P < 0.001).
The mean lead time of all appointments was 10.2 (± 14.7) days. As shown in Table 1, the average lead time for the no-show patients was 11.7 (± 15.6) and 8.8 (± 13.7) days for the attended patient (P < 0.001). The rate of no-shows for appointments scheduled within not more than two weeks was significantly lower (46.6% vs. 62.6%) than appointments scheduled for more than two weeks (P < 0.001). Appointments for morning clinics had a significantly higher no-show rate of 50.5% (P < 0.001). The findings show that the lowest rate of non-attendance occurred in TAS (26,349 patients or 41.9%), and the highest rate of no-shows was in WAS (12,251 patients or 56.5%) (P < 0.001).
| Variable | Show | No-Show | P Value |
|---|---|---|---|
| Lead time, d | < 0.001 | ||
| Mean (SD) | 8.8 (13.7) | 11.7 (15.6) | |
| ≤ 2 w | 61979 (53.4) | 54146 (46.6) | < 0.001 |
| > 2 w | 11960 (37.4) | 19992 (62.6) | |
| Clinic working shifts | < 0.001 | ||
| Morning | 42719 (49.5) | 43558 (50.5) | |
| Evening | 31220 (50.5) | 30580 (49.5) | |
| Appointment systems | < 0.001 | ||
| TAS | 36544 (58.1) | 26349 (41.9) | |
| WAS | 9421 (43.5) | 12251 (56.5) | |
| IVR | 27974 (44) | 35538 (56) | |
| Month of appointment | < 0.001 | ||
| Farvardin (20 Mar - 19 Apr) | 5011 (54.7) | 4150 (45.3) | |
| Ordibehesht (20 Apr - 20 May) | 6668 (52.8) | 5955 (47.2) | |
| Khordad (21 May - 20 Jun) | 7028 (53.3) | 6158 (46.7) | |
| Tir (21Jun - 21 Jul) | 5923 (50.3) | 5855 (49.7) | |
| Mordad (22 Jul - 21 Aug) | 6416 (51.3) | 6087 (48.7) | |
| Shahrivar (22 Aug-21 Sep) | 6025 (48.1) | 6493 (51.9) | |
| Mehr (22 Sep - 21 Oct) | 5563 (49.0) | 5794 (51.0) | |
| Aban (22 Oct - 20 Nov) | 6388 (51.1) | 6101 (48.9) | |
| Azar (21 Nov - Dec) | 6018 (47.4) | 6674 (52.6) | |
| Dey (21 Dec - 19 Jan) | 6802 (48.5) | 7235 (51.5) | |
| Bahman (20 Jan - 18 Feb) | 6677 (47.3) | 7454 (52.7) | |
| Esfand (19 Feb - 20 Mar) | 5420 (46.7) | 6182 (53.3) |
Characteristics of Patient Appointments (N = 148,077)a
The results of logistic regression analysis show that variables including the lead-time (OR = 1.80), web-based appointment system (OR = 1.71), interactive voice response appointment system (OR = 1.69), month of appointment (OR = 1.03), and clinic working shift (OR = 0.94) were the predictive variables for patient no-shows. Based on these findings, the most important predictive variable was the lead time; the odds of no-shows among patients with higher lead time (> 2 week) was 1.8 times more than that of other patients (≤ 2 week). In addition, the odds of no-shows in the AVR appointment system was 1.69 times more than that of TAS. The odds of non-attendance in patient who used WAS was 1.71 times more than that of patients scheduled with TAS. No-shows were 0.6% lower in evening clinics than in morning clinics (OR = 0.94) (Table 2).
| Variables | OR | 95% CI for OR | P Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Lead-time, w (> 2/≤ 2) | 1.80 | 1.76 | 1.85 | < 0.001 |
| Appointment system1 (WAS/TAS) | 1.71 | 1.66 | 1.76 | < 0.001 |
| Appointment system 2 (AVR/TAS) | 1.69 | 1.65 | 1.73 | < 0.001 |
| Appointment month(other month/march) | 1.03 | 1.02 | 1.03 | < 0.001 |
| Clinic working shift (evening/morning) | 0.94 | 0.92 | 0.96 | < 0.001 |
4. Discussion
This is the first study in Iran that investigates the no-show rate and its predictors in a general teaching hospital. The results show that the no-show rate is 50.1%. Previous studies in other countries report the no-show rate to be from 4% to 41% (7, 18-23). Compared to previous studies, the non-attendance rate was significantly higher in our study. It seems that the lack of reminders and a missing cancellation process in the appointment system are the main reasons for this issue. McLean et al. report that reminder systems such as voice or text messaging are effective in improving the patient attendance at the clinic (24). It has been proved that deploying reminders can reduce the no-show rate (25). Moreover, employing the process for change and cancelation of appointment is a feature of a good appointment system (26). Therefore, implementing text message reminders and a cancelation process in outpatient clinics can decrease the no-show rate and improve patient attendance.
The no-show rate was 16% lower for appointments with less than two weeks of lead time and the odds of no-show for appointments with lead time of more than two weeks was 1.8 time higher than that for other appointments. The findings of previous studies show that patients with higher appointment lead time are more likely to not attend their scheduled appointments (5, 15, 27). Drewek et al. report that the rate of non-adherence is significantly lower for visits scheduled ≤ 30 days in advance compared to visits scheduled > 31 days in advance (23%. vs. 47%) (18). Huang et al. stated that the odds of patient showing up with lead time of less than two weeks were 0.66 (11). All these findings are in line with our results. It seems that long waiting times make patients reluctant to seek treatment or motivate them to go to another clinic. Increasing working hours of outpatient department or improving clinic efficiency through process reengineering may decrease lead time and non-attendance rate.
Finding indicate that no-show probability in evening clinics is 6% less than that in morning ones. This result is contrary to the previous findings that point out that evening appointments significantly anticipate no-shows (11, 23, 28). In EHMC, most of the evening clinics are staffed by faculty physicians without the presence of medical residents, which may be the reason for better patient shows in the evening clinics. McMullen et al. showed that the no-show rate in resident clinics is higher than that in faculty clinics (9.1% vs. 2.4%) (2). Another possible reason may be that the evening shift is a good time for employees, while in the morning shift, due to job issues, patients may not be able to keep their medical appointment. AlSadhan indicates that the inability to take a leave from ones workplace or school was one of the main reasons for the missed appointment (12).
The findings imply that no-show rates are lowest during the spring and summer months and highest in the fall and winter. The highest rate of no-shows (53.3%) was in Esfand (Feb 19 - Mar 20). This can be due to the characteristics of this month in Iran. Esfand in Iran coincides with the beginning of the New Year and the related holidays; as a result, this outcome is expected. Meanwhile, the weather conditions in the fall and winter months can be a reason for the high rate of no-shows. Kheirkhah et al. report that the rate of no-shows is higher in the winter months, which matches the results of our study (6).
No-show rates were significantly lower in patients who used TAS compared to users of other appointment systems (41.9% vs. 56.5% and 56%, P < 0.001). In our model, “appointment system” is the second-most important predictor of no-shows. In other words, no-show odds in patients scheduled with WAS and IVR are approximately two times higher than those with TAS. The reason for this is the use of nurse-led telephone triage, which provides better interaction with the patient, better understanding of the patient’s conditions, and guidance for choosing the right specialty. Shaffer et al. indicate that implementation of triage systems compared to traditional scheduled system significantly enhance patients’ adherence rates (29). In addition, implementing a triage procedure in a child and adolescent psychiatry outpatient clinic in Hong Kong led to a decrease in waiting time and non-attendance rates (30).
This study has certain limitations. Due to the lack of registration of the patient demographic variables (such as gender, age, place of residence, etc.) in the appointment system, we were not able to compare the no-show rate based on these variables and their impact on no-shows. Such variables should be analyzed in future researches. However, large samples sizes, no missing values, and use of the regression model are some of the main advantages of this study.
4.1. Conclusions
Regarding the high rate of patient no-show and the clinical and economic consequences of this phenomenon on the patient, hospital, and the health system, its prevention and reduction are necessary. Findings indicate that appointment lead time is the main predictor of no-shows. Therefore, any interventions aimed to reduce the no-show rate should consider the lead time. Deploying strategies to reduce lead time such as increasing the number of physicians, increasing working hours, or improving clinic efficiency can improve patient attendance. Appointment reminders, cancellation policy, and nurse-led telephone triage can be expected to decrease patients’ no-show.