1. Background
Pain is a common and unavoidable component of the delivery process (1). Labor pain in terms of severity and location is very diverse and is among the most severe pains in human (2). There are several ways to reduce labor pain that are divided into two general categories: non-pharmacological (psycho prophylactic, hypnotism, acupuncture, healing touch therapy, relaxation exercises, massage therapy, music therapy, aromatherapy, etc.), and pharmacological (systemic medicines, inhalation anesthesia, general anesthesia, regional anesthesia) methods (3-5). Non-pharmacological methods of reducing the labor pain are often cheap and simple and can be used as a complementary therapy along with medication. They reduce the physical sense of pain, and also by increasing the mother's mental ability can stop the pain (6). Among non-pharmacological methods of reducing labor pain are heat and cold therapies with water that are considered as effective methods of labor pain relief (7). The application of heat therapy is simple, inexpensive, available during labor, requires no previous skills, and has few side effects if applied properly (8). The effect of heat to reduce pain is explained by the gate theory of pain. This theory suggests that there is a gate mechanism in the spinal cord that inhibits the crossing of pain signals by closing the gate system in the spinal cord (9). Heat increases pain threshold with increasing temperature, blood circulation, and metabolism and reduces muscle spasms (10). Studies showed that the heat causes a significant increase in uterine activity without altering the fetal heart rate (11). Therefore, hot water is effective in reducing the duration of the first phase of labor (12, 13). The study by Dahlen et al., showed that, heat therapy on perineum at the second phase of labor significantly reduced the severity of pain in this phase and post-labor pain during the first three to four hours in comparison with the control group (14).
Cold therapy with different mechanisms may help to decrease pain. This effect varies from analgesic stimulation, inhibition of awareness of pain by stimulating peripheral nerve receptors, improving the flow of energy in acupuncture points (15), reducing muscle tension (16), changing velocity of nerve conduction, and slowing down the transmission of pain to the central nervous system (17) to the distraction of thought from pain (18). Reducing the levels of catecholamine and increasing the levels of endorphins are among other mechanisms of cold therapy (19). According to the gate theory of pain, the cold effectively blocks the conduction of sensory fibers, and reduces pain; and in this way the pain threshold is increased (20). Cold therapy or cryotherapy as a non-pharmacological intervention has a range of surface application of deep massage with ice on the back, chest, rectum and perineum to reduce labor pain. This method, in addition to relieving pain has a healing effect on muscle spasms, reduces inflammation, and helps to improve tissue edema during labor (12, 21-23).
Due to the importance of reducing the labor pain, and based on the focus of program “holistic promotion of health and medical education” to prioritize natural delivery (24), use of non-pharmacological methods of reducing labor pain, suffering, and fear of delivery leads to the reduction of cesarean section and promotion of natural birth (25). The majority of previous studies were conducted only on pain intensity and few studies were conducted on birth outcomes. Therefore, the current study aimed at investigating the effect of localized heat and cold therapy on pain intensity, duration of the phases of labor, and birth outcomes among primiparous females. Satisfaction of mother was also compared in the two intervention groups.
2. Objectives
The current study aimed at investigating the effect of localized heat and cold therapy on pain intensity, duration of phases of labor, and birth outcomes among primiparous females referring to Kamali hospital, Karaj, Iran.
3. Methods
The current randomized, controlled trial was conducted from September 2015 to January 2016. The study was performed at Iran hospital in Karaj city (Alborz Province, Iran). The inclusion criteria were primiparous females (18 - 35 years old) with a singleton pregnancy, gestational age over 37 weeks, cervical dilation 3 - 4 cm, cephalic presentation, and receiving no analgesia during labor.
Exclusion criteria were diagnosed anatomical or mental disorders (psychosis, schizophrenia, disorders of the uterus, and cephalopelvic disproportion (CPD), known chronic diseases, including heart disease, lung disease, hypertension, diabetes and skin diseases (including any injury, inflammation, and eczema in heat/cold therapy location), indication for cesarean section, abnormal fetal heart rate patterns, history of chronic pelvic pain, history of infertility, any complications during labor (prolapsed cord, abnormal fetal positions, placental abruption, etc.), living apart from husband (due to the violence, divorce, and on the verge of divorce), and the use of narcotics about eight hours before active labor.
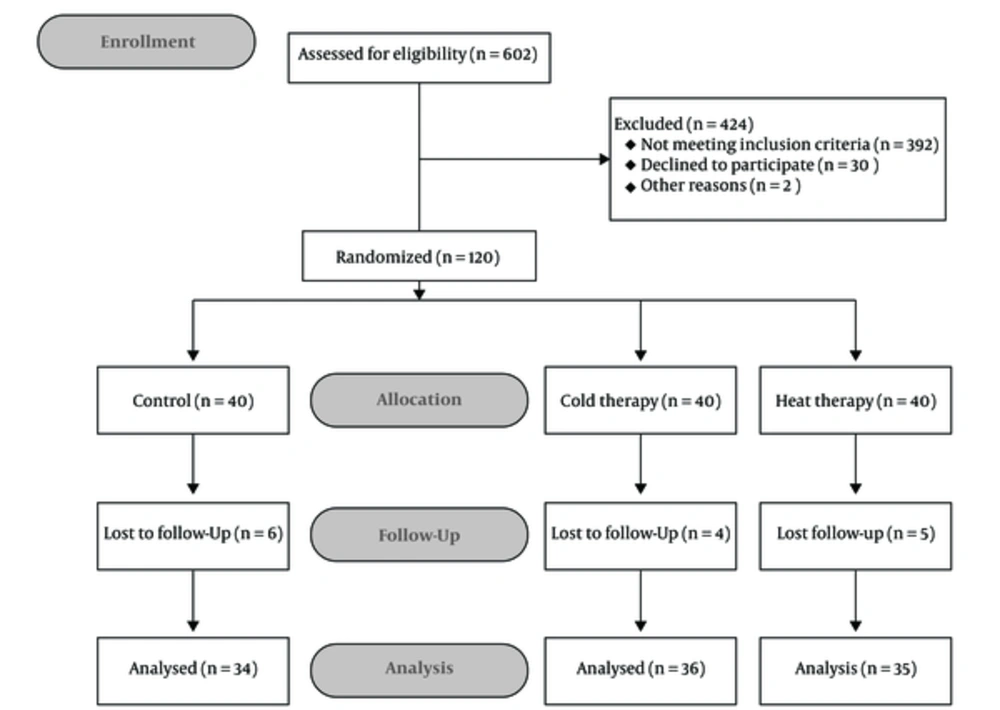
The sample size was estimated based on statistical formula (power: 80%, confidence interval (CI): 95%, α = 0.05, K = 3). With the prediction of 10% dropouts in follow-up, the minimum required subjects in each group were determined 40; total subjects 120. All eligible subjects signed the informed consent form before enrolment in the study. The current study was approved by the ethics committee of Alborz University of Medical Sciences (AUMS) (IRCT number: IRCT2015031021020N1).
The subjects were selected using a convenience sampling method, and randomly divided into two interventions and one control groups. Randomization numbers were sealed in a predetermined computer-made randomization opaque envelope. The pregnant females’ screening sequence numbers were printed outside the envelope, whereas the group names were printed inside. All envelopes were numbered consecutively. Researchers screened the eligible pregnant females after baseline, separated the envelopes from the strain, and opened them according to the pregnant females’ screening sequence numbers, and then assigned the patients to either the intervention groups (two groups) or the control group. Before any intervention, the intensity of pain in 3 - 4 cm dilatation (the beginning of the active phase) in all three groups was measured by McGill pain ruler. McGill pain ruler indicates 0 (no pain) to 10 (most intense pain) from left to right. The test-retest analysis was used to assess reliability. In the pilot study, the pain intensity in 20 mothers was measured by the researchers, separately, and the correlation between their measurements were r = 0.78. Face and content validity of satisfaction questionnaire was measured by 10 reproductive health experts.
In the heat therapy group, after making an appropriate communication with the pregnant females, researcher used a hot water bottle covered with a towel all through the labor to warmth lower back and abdomen of the subject. The hot water bottle was used during contraction in the first phase of labor (the least amount of time used in the first phase was 60 minutes). The reason for the use of this device was that it was easy to provide, use, and clean for other participants. The researcher had two hot water bottles for each subject; therefore, if the first bottle lost its warmth (checked the temperature with a mercury thermometer every 10 minutes), the second bottle was used. According to several studies (12), the researcher tested the temperature of hot water bottle by placing it against her forearm for few seconds and if the temperature was right covered the bottle with a towel and placed it on the skin of the participant during labor at desired locations. Based on previous studies (7) the temperature of hot water bottle should be 38 - 40°C. The temperature of hot water bottle in this situation was also checked by mercury thermometer to ensure that the temperature was right. The temperature of the bottle was continuously measured to make sure it was 38 - 40°C.
In the second phase of labor, before transferring the subject to the delivery bed, the researchers covered the hot water bottle with a clean towel and placed it on perineum during the contraction for at least four minutes (26).
In the cold therapy group, a similar method was used, but hot water bottle was replaced with an ice pack on lower parts of the subject’s back and abdomen for 10 minutes every 30 minutes during the first phase and on perineum for five minutes every 15 minutes during the second phase of labor (27). The temperature of the ice pack was expected to reduce pain perception, which should be in the range of 10 - 15°C (28). The temperature of the ice pack was checked using a mercury thermometer to ensure the temperature was right. It should be mentioned that, the ice pack was placed on the desired area as long as it had the right temperature (10 -15°C). Pain assessment in the first phase of labor in addition to dilatation of 3 - 4 cm (the beginning of the active phase of labor), dilation of 5 - 6 cm (accelerated phase), 7 - 8 cm (maximum of slope), and 9 - 10 cm (the deceleration) was also conducted after the delivery. To assess pain intensity, the McGill linear pain scale was explained to the mothers by the researcher in order to measure the pain. But, no intervention was applied to the control group.
A total of 15 participants were excluded from the current study. In the cold therapy group, four participants were excluded due to intolerance of old therapy (n = 2), and emergency caesarean section (n = 2). In the heat therapy group, five participants were excluded due to abnormal pattern of fetal heart rate (n = 3), and intolerance to heat therapy (n = 2). In the control group, six participants were excluded due to emergency caesarean section (n = 4), diagnosis of placental abruption (n = 1), and abnormal pattern of fetal heart rate (n = 1). The final analysis was performed on 105 subjects (Figure 1).
3.1. Statistical Analysis
Data were analyzed using the Fisher exact, Chi-square, the Kruskal-Wallis, and ANOVA tests with SPSS version 19. In all the tests, P value < 0.05 was considered statistically significant.
4. Results
A total of 120 participants were included in the study of which 105 were considered eligible for data analysis. Chi-squire test did not show statistically significant differences among the three groups (two intervention groups and one control group) before the intervention in terms of demographic and clinical characteristics such as occupation, educational level, and status of amniotic fluid (Table 1). The Kruskal-Wallis test also did not show statistically significant differences among the three groups before intervention in terms of demographic and clinical characteristics such as age, gestational age, time of rupture of membrane, and time of oxytocin usage (Table 2).
| Variable | Heat Therapy | Cold Therapy | Control | P Value |
|---|---|---|---|---|
| Occupational status | 0.843 | |||
| Unemployed | 14 (40) | 14 (40) | 16 (44.3) | |
| Employed | 21 (60) | 22 (60) | 18 (55.7) | |
| Educational level | 0.841 | |||
| Illiterate | 6 (17.1) | 7 (20) | 4 (11.4) | |
| Primary school | 7 (20) | 11 (28.6) | 7 (20) | |
| Middle and high school | 14 (40) | 10 (28.5) | 13 (40) | |
| Graduated | 8 (22.9) | 8 (22.9) | 10 (28.6) | |
| Status of amniotic fluid | 0.851 | |||
| Intact | 18 (51.4) | 20 (57.1) | 20 (57.1) | |
| Rupture | 17 (48.6) | 16 (42.9) | 14 (42.9) |
aValues are expressed as No. (%).
| Variable | Heat Therapy | Cold Therapy | Control | P Value |
|---|---|---|---|---|
| Age, y | 25.08 ± 5.41 | 24.02 ± 4.72 | 24.77 ± 4.91 | 0.71 |
| Gestational age, week | 39.14 ± 1.11 | 39.20 ± 1.10 | 38.77 ± 0.91 | 0.203 |
| Time of oxytocin usage, min | 39.14 ± 1.11 | 39.20 ± 1.10 | 38.77 ± 0.91 | 0.071 |
| Time of rupture of membrane, min | 59.70 ± 31.79 | 58.66 ± 40.94 | 53.81 ± 50.66 | 0.692 |
The Kruskal-Wallis test showed that the three groups before intervention had no statistically significant differences in terms of pain intensity in 3 - 4 cm dilated (beginning of active labor). After intervention, in dilations of 5 - 6 cm (P = 0.049), 7 - 8 cm (P = 0.042), and 9 - 10 cm (P = 0.001) in the first and second phase of the labor (P = 0.001), statistically significant differences were observed in terms of pain intensity among the three groups. Results of least significant difference (LSD) test showed that the least mean pain intensity in different dilatations was during the first and the second phases of labor in the heat therapy group (Table 3). Therefore, after intervention, in dilations of 5 - 6 cm, 7 - 8 cm, and 9 - 10 cm in the first and second phases of the labor, the mean pain intensity in the intervention groups was lower than that of the control group. The highest reduction in the pain intensity in different dilatations during the first and the second phases of labor, according to LSD test, was related to the heat therapy group.
| Pain Intensity | Heat Therapy | Cold Therapy | Control |
|---|---|---|---|
| Before intervention (dilatation 3 - 4 cm) | 3.82 ± 1.17 | 3.85 ± 1.14 | 3.57 ± 1.14 |
| After intervention (dilatation 5 - 6 cm) | 3.25 ± 0.91 | 3.57 ± 1.14 | 4.00 ± 1.37 |
| After intervention (dilatation 7 - 8 cm) | 4.08 ± 0.91 | 4.88 ± 1.05 | 4.97 ± 1.17 |
| After intervention (dilatation 9 - 10 cm) | 6.00 ± 1.35 | 6.40 ± 1.09 | 7.80 ± 1.18 |
| Second phase | 6.22 ± 1.13 | 7.37 ± 1.08 | 7.94 ± 1.08 |
aValues are expressed as mean ± SD.
The Kruskal-Wallis test showed a statistically significant difference among the three groups in terms of the average duration of the first phase (P = 0.001), but there was no statistically significant difference among the three groups in terms of the average duration of the third phase. ANOVA results showed a statistically significant difference among the three groups in terms of the average duration of the second phases of labor (P = 0.023) (Table 4).
| Phase | Heat Therapy | Cold Therapy | Control | P Value |
|---|---|---|---|---|
| First, min | 293.70 ± 68.97 | 368.57 ± 79.82 | 400.86 ± 77.43 | 0.001 |
| Second, min | 42.85 ± 13.60 | 51.71 ± 12.24 | 46.85 ± 13.67 | 0.023 |
| Third, min | 10.68 ± 5.33 | 10.31 ± 3.92 | 9.20 ± 4.04 | 0.493 |
aValues are expressed as mean ± SD.
The Kruskal-Wallis test showed no statistically significant difference among the three groups in terms of birth outcomes (e g, the mean first and fifth Apgar scores, the time of cuddling the newborn infant, and the first breastfeeding) (Table 5).
| Variable | Heat Therapy | Cold Therapy | Control | P Value |
|---|---|---|---|---|
| First Apgar score | 8.68 ± 0.47 | 8.62 ± 0.49 | 8.68 ± 0.47 | P = 0.841 |
| Fifth Apgar score | 9.85 ± 0.35 | 9.94 ± 0.23 | 9.97 ± 0.16 | P = 0.172 |
| Time of cuddling the newborn | 4.14 ± 0.97 | 4.14 ± 1.00 | 4.34 ± 1.23 | P = 0.861 |
| Time of breastfeeding | 5.28 ± 1.90 | 5.31 ± 1.89 | 5.91 ± 2.17 | P = 0.432 |
aValues are expressed as mean ± SD.
The Fisher exact test showed no statistically significant differences between the two interventions groups in terms of maternal satisfaction (Table 6).
| Satisfaction | Heat Therapy | Cold Therapy | P Value |
|---|---|---|---|
| Type of intervention | 0.671 | ||
| Satisfied/very satisfied | 24 (68.6) | 25 (65.6) | |
| Neutral | 11 (31.4) | 11 (34.4) | |
| Dissatisfied/very dissatisfied | 0 (0) | 0 (0) | |
| Desire to re-use | 0.782 | ||
| Yes | 25 (71.4) | 26 (74.3) | |
| Delivery process | 0.952 | ||
| Satisfied/very satisfied | 27 (77.1) | 28 (77.2) | |
| Neutral | 8 (22.9) | 8 (22.8) | |
| Dissatisfied/very dissatisfied | 0 (0) | 0 (0) | |
| First experience of breastfeeding | 0.782 | ||
| Satisfied/very satisfied | 29 (82.9) | 28 (80) | |
| Neutral | 6 (17.1) | 8 (20) | |
| Dissatisfied/very dissatisfied | 0 (0) | 0 (0) |
aValues are expressed as No. (%).
5. Discussion
The results of the current study showed no statistically significant difference in the pain severity before the intervention in 3 - 4 cm dilatation among the three groups. However, statistically significant differences were observed among the three groups in other dilatations in the first phase of labor, that is the 5 - 6 cm, 7 - 8 cm, and 9 - 10 cm dilatations, and also in the second phase of labor. These results were consistent with those of the study by Ganji et al., entitled “effects of alternating heat and cold on the pain and labor outcomes”. In their study, they used 38 - 40°C hot water bottle wrapped in a towel on the abdomen, lower abdomen, and lower back of females in labor for 30 minutes during contraction. Then, they placed an ice pack wrapped in a towel on the same places for 10 minutes during the first phase of labor. This exercise was repeated frequently during the first phase of labor. In the second phase, hot water bottle was placed on the perineum for 15 minutes and then, the ice pack was placed in the same locations for five minutes. This exercise was repeated frequently during the second phase of labor. Results showed that the severity of pain was reduced in the first phase of labor during 5 - 6 cm, 7 - 8 cm, and 9 - 10 cm dilatations as well as the second phase, and this pain reduction was statistically significant compared with that of the control group (7). In the current study, although the method of intervention was not frequently repeated and the effects of cold and heat therapy were examined separately, the obtained results regarding the reduction of pain severity at the first phase during 5 - 6 cm, 7 - 8 cm, and 9 - 10 cm dilatations as well as the second phase of labor were consistent with the findings of Ganji et al. Furthermore, results of the study by Shirvani et al., that investigated the effect of ice pack on pain reduction and labor outcomes showed that using ice pack on abdomen and back for 10 minutes every 30 minutes at the first phase and also on perineum for five minutes every 15 minutes at the second phase of labor could not significantly reduce the pain severity at the first phase during 5 - 6 cm, 7 - 8 cm, and 9 - 10 cm dilatations as well as the second phase of labor (23). In their study, although pain intensity was slightly lower in the heat therapy group during labor, it was not significantly different among the three groups. The duration of the second stage of labor was significantly lower in the cold therapy group (P = 0.02). There were no significant differences in duration of the first and third stages, fetal heart rate, and Apgar score among the groups. Based on the current study results, the effect of heat and cold therapy on the reduction of labor pain was not significantly different. Also, alternating the sensory stimulus by heat and cold was not more effective than each of them separately. In the study by Smith BW et al., pain threshold raised with both heat and cold in patients with rheumatoid arthritis. There were no significant differences in the pain threshold between warm bath and ice massage groups. Of course, the cold effects were more than the heat (29). It seems that applying cold or heat can influence the outcomes. In the current study, the same form of heat and cold was used, thus more investigations are needed to compare the effect of various forms of heat and cold. Also, more reduction of pain was observed at the first phase during 5 - 6 cm, 7 - 8 cm, and 9 - 10 cm dilatations in the heat therapy group compared with the control group. Most studies did not compare the relieving effect of heat and cold (23). In the current study, the heat therapy intervention was also conducted at the second phase of labor, which also showed the reduction of pain at the second phase in heat therapy group. In this regard, the study by Dahlen et al., that examined the effect of heat therapy on the perineum at the second phase of labor indicated that the severity of pain in pregnant females during the second phase of labor three to four hours before discharging from delivery room was statistically different from that of the control group, which indicated the reduction of pain due to the effect of heat therapy in the intervention group compared with the control group (14).
In the current study, the average duration of first and second phases of labor showed a statistically significant difference among the three groups, but no statistically significant difference was observed among the three groups regarding the average duration of the third phase of labor, which was inconsistent with the results of the study by Behmanesh et al. They reported that the duration of the first and third phases of labor in the heat therapy group was less than those of the control group, but the duration of the second phase showed no statistically significant differences between the two groups (30). Perhaps, one of the reasons of this inconsistency could be the non-similarities of factors such as watering rupture (premature rupture of membranes; PROM) and lack of oxytocin use in the two studies. According to another report, labor pain was decreased by a cold pack (31). It was also reported that the intermittent heat and cold therapy effectively decreased labor pain compared with the control group (7). Some mechanisms for effectiveness of heat/cold include providing stimuli from peripheral sensory receptors to inhibit pain awareness, antinociceptive effects on the gate control system, decreasing muscle tension, and distraction of attention from pain (32-34).
In the current study, no statistically significant difference was observed among the three groups in terms of average Apgar score in the first and fifth minutes, which was consistent with the results of several other studies (14, 23, 30). Therefore, it seems that heat therapy and cold therapy intervention had no negative effects on Apgar score or other factors such as time of cuddling the newborn after giving birth and the first breastfeeding.
In the current study, no statistically significant difference was observed between the two groups (heat and cold) such as satisfaction with the type of intervention, the desire to re-use, satisfaction with the delivery process, and satisfaction with breastfeeding. Therefore, both groups were equally satisfied with the method of heat and/or cold therapy. It seems that females able to actively participate in their labor and control their pain had higher satisfaction (32). Taavoni et al., showed that the average satisfaction score was significantly higher in the heat therapy group than the control group (35). In another study (23, 36), most of the mothers preferred heat, since majority of them had high satisfaction in the heat and alternate heat and cold therapy groups, whereas most of the mothers in the cold group had moderate satisfaction (23). Of course, the type of heat/cold therapy may affect the satisfaction. In a review, East et al., reported that females were more satisfied with the use of cold gel pads than ice packs. Mothers’ satisfaction should be considered for selection of a pain relief method (37). Both heat and cold provide relief and comfort, and should be used by desire and the preference of females. Superficial heat and/or cold therapy provide active participation of females in the birthing process, and promote a more positive birth experience. Among other factors associated with mothers’ satisfaction with the process of labor and delivery are the mother's emotions and feelings, duration of labor, the need for intervention, condition of the infant, and the support of the treatment team and family (38, 39). This study had certain limitations. The control of individual differences and previous experience of the patients were not possible. Localized heat and cold therapies are non-pharmacological, non-invasive, satisfying the primiparous females, and effective methods to control and relieve pain during labor without adverse effects on maternal and fetal outcomes.