1. Background
Nowadays, the fast increasing trend of chronic diseases is one of the main health challenges of the world and the burden caused by these diseases increase in spite of the relative improvement of community health status (1-3). Chronic diseases are one of the main causes of mortality, disability, and dissipation of health expenditure in the world (4, 5). The long lasting nature of chronic diseases causes the health systems to reverse their aim of curing the disease to maintain the patients function and ability. Chronic disease management needs special attention due to their high impact both on the individual and the community (6, 7).
Hence, most of HIT interventions are developed for people with chronic illnesses. These technologies have an important role in optimal management of chronic diseases and changing patients’ lifestyle (6, 8-10). Nowadays, lots of HIT technologies such as decision support technologies, telemedicine, teleconsultation, professional medical websites, social networks, virtual visits, and electronic reservation systems are introduced to manage and control the chronic diseases (9, 11, 12).
Patient-based information communication technologies (ICT) help patients to have an active role in their own care and decision-making process and to directly interact with health care providers and health care systems about their individual health concerns (12-14). Also, health information technology (HIT) interventions in chronic diseases lead to individual results such as quality of life improvement, mortality reduction, pain reduction, and facilitating communication with care providers, professional health related results including drug and treatment compliance, improving the quality of documentation and communication, and increasing health knowledge, and organizational results such as cost-effectiveness, the effectiveness of time and quality, decline in length of hospitalization, reduction of emergency visits, and replacement of in person visits instead (6, 12, 15). The importance of the HIT role to manage chronic diseases is more and more in future years due to the increasing trend of patients with such diseases (6).
However, despite the development of various applications of information technology in the whole clinical aspects and ensuring their efficiency, the application of technology in medical and therapeutic fields is not fully developed yet, and there are lots of challenges and barriers in its adoption and application (4, 10). The wide range of technologies, the way to access them, concerns about security, privacy, lack of motivation, and low skill of users are among the challenges which lead to HIT utilization decrease (4, 16, 17).
Health care costumers should have the necessary capabilities and skills to benefit from the IT in the health filed (10, 18, 19). IT tools can help the self-management of chronic diseases only if patients are prepared to use these technologies and accept them (10, 16, 19, 20). Therefore, assessing patients’ readiness including investigating their skills, concerns, and motivation to use technology can predict their use of these technologies (10). The HIT system developers should pay attention to the main causes and motives that make the patients successfully implement these systems (21).
Several studies conducted on assessing patients’ readiness to use IT in the health field indicate that patients do not have enough skill to use such technologies (18, 21-25) and they reach the required readiness level to use and accept technology by having access to e-health programs and receiving related training (20, 23, 26). Also, the adoption of new technologies by patients’ needs collaboration and support from care providers, hospitals, health plans, and the government (6). In Iran, many studies are performed on evaluating the skills of using the internet in the healthy shell of the community, including the youth and adolescents (27-29), but the skills of how to use IT in patients are not studied yet. Since the burden of chronic diseases is much higher than other diseases, application of IT can play an important role in the management of such diseases. Therefore, the current study aimed at assessing the readiness of patients with chronic diseases referring to clinics of educational hospitals in Khorramabad, Iran to employ HIT. The results of the current study can help to predict chronic patients’ utilization of IT resources and its challenges. Removal of IT adoption challenges by patients can lead to lifestyle changes and self-management of chronic diseases through the application of such technologies.
2. Methods
The current cross sectional study was conducted on patients with chronic respiratory, cardiovascular, renal, and diabetes diseases at a local level in 2016. The inclusion criteria to select patients with chronic diseases were: age range of 18 - 65 years, reading and writing literacy, history of at least one visit in the selected clinics, and signing informed consent of participating in the current study.
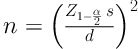
To determine the sample size, the following formula was employed; considering the error level = 0.05, standard deviation (SD) = 0.67, and d = 0.06, the sample size was approximately set to 475 subjects.
The SD was calculated based on a pilot study with a sample size of 20. The subjects were selected among patients referring to the clinics and outpatient dialysis unit of educational hospitals of Khorramabad, within three months, based on the convenience sampling method.
The data gathering tool was the valid questionnaire of the patient readiness to engage in health internet technology (PRE-HIT) developed by Koopman et al. aimed at assessing chronic patients’ readiness to interact with HIT (mobile technologies and internet). The questionnaires were completed by the patients and in some cases by the interviewers. Koopman et al. used methods of primary focus groups, item development and refinement, and exploratory factor analysis (EFA) to determine the final items and factors structure (10). It is noteworthy that the internal consistency of the whole eight factors was verified based on the mean of Cronbach’s alpha coefficient (0.74), the reliability of the eight subscales was verified based on test-retest with Pearson correlation coefficient that ranged 0.60 - 0.85, and its construct validity was also approved (5).
In order to confirm the true translation of PRE-HIT questionnaire and ensure to have the main concept of the original version of the questionnaire, the translation and back-translation technique was employed. Therefore, at first the mentioned tool was translated by two bilingual translators from English into Persian and then, a common Persian version was provided based on the comparison of the two translated texts and consultation with two translators. Then, its back-translation was performed by a translator fluent in the two languages from Persian into English, and the similarity of the translation with the original version was examined and necessary amendments were made. Also, the validity of the content of this tool for its application in Iran was approved by a panel consisting five experts of medical librarianship and notification, health information management (HIM), and medical informatics. The reliability of the tool was confirmed by Cronbach’s alpha of 0.79 and the correlation coefficient of 0.83. The PRE-HIT questionnaire is composed of two parts; the first part includes sociodemographic characteristics including gender, age, marital status, level of education, living place, job, self-reporting of health status, and disease type, and the second part has 28 items summarized in eight factors as health information needs (five items), computer/internet experience (four items), computer anxiety (four items), preferred interactive method (five items), relationship with doctor (three items), cell-phone expertise (two items), internet privacy concerns (two items), and health news (three items). A four-point Likert-scale (totally agree, agree, disagree, totally disagree) was used to assess patients’ views. To score the answers, number 1 is considered for totally disagree, number 2 for disagree, number 3 for agree, and number 4 was assigned for totally agree for all items except items 1 - 4 for computer usage, item 2 for preferred interactive method, items 1 - 3 for relationship with doctor, items 1 and 2 for internet privacy concerns, and item 1 - 3 for receiving health related news. The readiness level was interpreted according to the mean score of each factor and total mean score by dividing into three categories: low (1 - 1.99), medium (2 - 2.99), and high (3 - 4).
The results were analyzed by descriptive and analytic statistics. Data analysis was performed with SPSS version 20. Chi-square was used to test the association of computer work experience with socio-demographic attributes. The correlation between the factor of relationship with doctor and type of chronic disease and sociodemographic characteristics were investigated by the nonparametric Mann-Whitney and Kruskal-Wallis tests, and the independent t test and ANOVA were employed to examine the relationship between other patients’ readiness factors with these variables. The criteria to use statistical test was a normality test (Kolmogorov-Smirnov test). The significance level was considered as P < 0.05 in the current study.
3. Results
Out of the 475 questionnaires distributed among the patients, 410 questionnaires were completed (response rate was 0.86%); from the total number of participants, 54.88% were male and 45.12% female. Most of participants were married (84.16%), with self-employed jobs (40%), below high school or high school level of education (55.12%), and living in urban areas (75.36%). The results showed that only 24.4 % (n = 100) of participants had computer work experience. The frequency of participants based on sociodemographic characteristics and also the relationship between computer work experience and these characteristics are shown in Table 1.
| Demographic Characteristic | Computer Work Experiencea | Total | P Value | |
|---|---|---|---|---|
| Yes | No | |||
| Gender | 0.978 | |||
| Female | 45 (24.3) | 140 (75.7) | 185 | |
| Male | 55 (24.4) | 170 (75.6) | 225 | |
| Marital status | 0.000 | |||
| Single | 33 (50.8) | 32 (49.2) | 65 | |
| Married | 67 (19.4) | 278 (80.6) | 345 | |
| Job | 0.000 | |||
| State employment | 46 (46.5) | 53 (53.5) | 99 | |
| Self-employed | 29 (17.7) | 135 (82.3) | 164 | |
| Academician | 5 (71.4) | 2 (28.6) | 7 | |
| Housewife | 18 (13.3) | 113 (86.7) | 135 | |
| Level of education | 0.000 | |||
| High school or lower | 8 (3.5) | 218 (96.5) | 226 | |
| High school diploma | 26 (25) | 78 (75) | 104 | |
| Associate’s or bachelor’s degree | 58 (79.5) | 15 (20.5) | 73 | |
| Master’s degree or higher | 7 (100) | 0 (0) | 7 | |
| Living place | 0.001 | |||
| Urban | 86 (27.8) | 223 (72.2) | 309 | |
| Rural | 12 (12) | 88 (88) | 100 | |
| Sum | 100 (24.4) | 310 (75.6) | 410 | |
The Relationship Between Sociodemographic Variables and Computer Work Experience
Among the patients that took part in the study, 106 subjects had cardiovascular diseases (25.8%), 98 had respiratory diseases (23.9%), 85 underwent dialysis (20.7%), 74 had diabetes (18.1%), and 47 patients had two or more chronic diseases (11.5%).
The computer work experience had a significant relationship with age, marital status, job, level of education, living place, health status, and type of illness (P = 0.001), but not with gender (P = 0.978).
The total readiness to apply HIT in patients with chronic diseases and a history of computer work experience was in medium level with the mean of 2.77. The highest and the lowest mean scores of HIT application were allocated to the relationship with doctor (3.37), and computer anxiety (2.30), respectively. The readiness of patients with chronic diseases to have experience and skill in working with computer and the internet, communication with doctor, and mobile related skills were at high levels (Table 2).
| The Chronic Patients Factor to Use HIT | The Readiness Score | |||
|---|---|---|---|---|
| Mean ± SDa | Maximumb | Minimumb | Readiness Level | |
| Online health information needs | 2.98 ± 0.56 | 4 | 1.67 | Medium |
| Computer/internet expertise | 3.01 ± 0.60 | 4 | 1 | High |
| Computer anxiety | 2.30 ± 0.60 | 4 | 1 | Medium |
| Preferred mode of interaction | 2.40 ± 0.47 | 3.6 | 1.2 | Medium |
| Relationship with doctor | 3.37 ± 0.52 | 4 | 1 | High |
| Cell-phone expertise | 3.03 ± 0.70 | 4 | 1 | High |
| Internet privacy concerns | 2.50 ± 0.77 | 4 | 1 | Medium |
| Receiving health related news | 2.63 ± 0.48 | 4 | 1.67 | Medium |
| Total | 2.77 ± 0.59 | 4 | 1 | Medium |
The Score of Patients with Chronic Diseases to Use HIT Based on the Patient Readiness Factors
Computer anxiety, preferred interactive method, and cell-phone expertise did not have any significant relationship with sociodemographic variables (P = 0.37). But, the factor of online health information needs had a significant relationship with job, educational level, relationship with doctor, disease type, and the living place. Also, the computer/internet expertise had a significant relationship only with the educational level. In addition, privacy concerns and receiving health related news had a significant relationship with job and gender, respectively (Table 3).
| Patient Readiness Factor | Total Score | P Valuea |
|---|---|---|
| Online health information needs (total score = 20) | ||
| Job | 0.048 | |
| State employment | 15.5 | |
| Self-employed | 13.8 | |
| Academician | 15 | |
| Housewife | 16.4 | |
| Educational level | 0.002 | |
| Under the high school diploma | 13 | |
| High school diploma | 13.1 | |
| Associate’s or Bachelor’s degree | 15.7 | |
| Master’s degree or higher | 16 | |
| Computer/internet expertise (total score = 16) | ||
| Education level | 0.048 | |
| Under the high school diploma | 12.6 | |
| High school diploma | 10.9 | |
| Associate’s or Bachelor’s degree | 12.1 | |
| Master’s degree or higher | 13.5 | |
| Relationship with doctor (total score = 12) | ||
| Disease type | 0.04 | |
| Respiratory disease | 4.9 | |
| Heart disease | 4.5 | |
| Kidney disease | 5.3 | |
| Diabetes | 4.8 | |
| Concomitant diseases | 5 | |
| Living place | 0.005 | |
| Urban | 4.7 | |
| Rural | 5.3 | |
| Job | 0.023 | |
| State employment | 4.6 | |
| Self-employed | 4.9 | |
| Academician | 6.3 | |
| Housewife | 4.9 | |
| Privacy concerns (total score = 8) | ||
| Job | 0.029 | |
| State employment | 4.9 | |
| Self-employed | 5.6 | |
| Academician | 5.2 | |
| Housewife | 4.3 | |
| Receiving health related news (total score = 12) | ||
| Gender | 0.024 | |
| Female | 6.7 | |
| Male | 7.3 |
The Relationship Between Characteristics and Readiness Factors of Patients with Chronic Diseases to Use HIT
The results of investigating the correlation between patients’ readiness factors to use HIT and the observed variables showed that housewives (16.4) and patients with Master’s or higher degrees of education (4) had more online health information needs compared with other job related and educational groups. Also, these patients had more readiness for computer/internet expertise compared with other groups (5, 13). The highest patients’ readiness for online relationship with the doctor was allocated to patients with kidney diseases (5.3), rural habitation (5.3), and patients with an academic job (6.3). The lowest privacy concerns were allocated to self-employed patients (5.6). Furthermore, there was more readiness to receive health related news in male patients (7.3) (Table 3).
4. Discussion
The studies on the level of patient’s readiness to use IT are important to provide better services by health care providers. The results of the current study showed that the readiness to use HIT in patients with chronic diseases and computer expertise was in medium level; most of the patients had no computer work experience, especially the patients with lower education, which is a serious problem and should be considered by policy-makers. Also, in some countries, various studies assessed the readiness of patients to use HIT, and their results indicated adequate skill to use such technologies among the studied population (18, 21, 25). Evaluation of the patients' readiness regarding the use of HIT showed their capability and tendency toward utelizing such technologies and helped researchers to select the appropriate group of patients for this particular purpose (10). Also, the preliminary review of the HIT implementation results in saving time, money, and energy, and can increase the chance of successful technology implementation in addition to determining the communities not able to successfully implement technology immediately (30, 31).
According to the results of the current study, less than 25% of participants had the computer work experience. Also, Seplovich from Bronx of New York in a study developed an interventional approach to improve the attitude and use of internet and computer in females with HIV and reported same results about the very low computer skills and internet use among the patients (32). Although in the studies conducted in this field, more than 60% of patients with chronic diseases were reported as internet users (10, 23, 33). This difference can be due to lack of computer usage knowledge, lack of computer access, high mean age, and low educational level of participants in studies that reported very low level of computer skills and internet usage. Kruse et al. showed that age and educational level were among the important factors of using internet in patients with chronic diseases (4).
The patients’ readiness to use technology (internet and email) as the preferred interactive method was in medium level in the current study. However, in several studies, the use of email for communication between patients and health care professionals is emphasized due to ease-of-use, wideness, and low-cost (34-38), although the email communication in health care practices is still very poor (39). Hence, persuading patients to use new technologies can lead to care continuity, supporting self-care, and improving quality of life in such patients.
The results of the current study showed that the readiness of the housewives and patients with Master’s degree or higher levels of education in fulfilling online health information needs was more than those of the other jobs and educational groups. Also, the ability and experience to work with computer/internet in people with Master`s degree or higher levels of education was more than those of the others. The studies conducted in this field show that the educational level is among the most important factors of technology adoption (4, 40, 41). According to these studies, females have higher tendency toward searching and utilizing electronic health information, participating in online care programs, and developing and sharing information and content (42-50). The housewives readiness can be attributed to their enough free time, and the reason of people with Master’s degree or higher educational levels can be the capability to work with health technologies and their ease-of-use for them. Therefore, more attention should be paid to such differences in order to achieve more success in technology adoption by patients and develop HIT application based on the readiness of different cortexes of the community.
In the current study, rural patients had the most readiness to have online relationships with doctors. According to the performed researches, the online relationship between doctor and patients with chronic diseases has lots of benefits such as supporting self-care and improving patients’ quality of life (34, 36-38). Although some of the studies mentioned rural habitation as a positive factor in technology adoption and claimed that IT can provide the health care necessary resources for rural deprived areas (13, 40, 51), in some other studies, it is mentioned that there are lots of gaps, including the large number of elderly people, the lack of knowledge about using the computer, and the lack of appropriate internet bandwidth for village residents to access digital technologies (4, 52). The high patient’s readiness for online relationship with doctor in rural habitants in the current study can be due to the more distance of these patients from the doctor and lack of access to specialists in rural areas. Therefore, the improvement of the access of villagers to technologies such as the internet can promote the management of the patients with chronic diseases.
The successful deployment of IT in patients requires considering the topics such as the difference in their level of readiness to use IT, ease-of-use, ability to save time, and cost of technology. Also, it is suggested that the required planning be performed to increase the application of computers and access of patients to the internet, improve their readiness to use IT, and inform about the advantages of HIT use through full audience media. IT adoption by patients results in changes in lifestyles and self-care improvement. In addition, it is suggested that other studies be performed to determine the effective factors in HIT adoption in patients with chronic diseases using technology adoption theories, in line with the study goals.